
Can I take weight loss injections with underactive thyroid? This is a common question for individuals managing both hypothyroidism and obesity in the UK. Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become established treatments for obesity management. For patients with underactive thyroid taking levothyroxine, understanding whether these medications can be safely combined is essential. This article examines the evidence, safety considerations, and medical guidance for using weight loss injections alongside thyroid hormone replacement therapy, helping you make informed decisions about your weight management options.
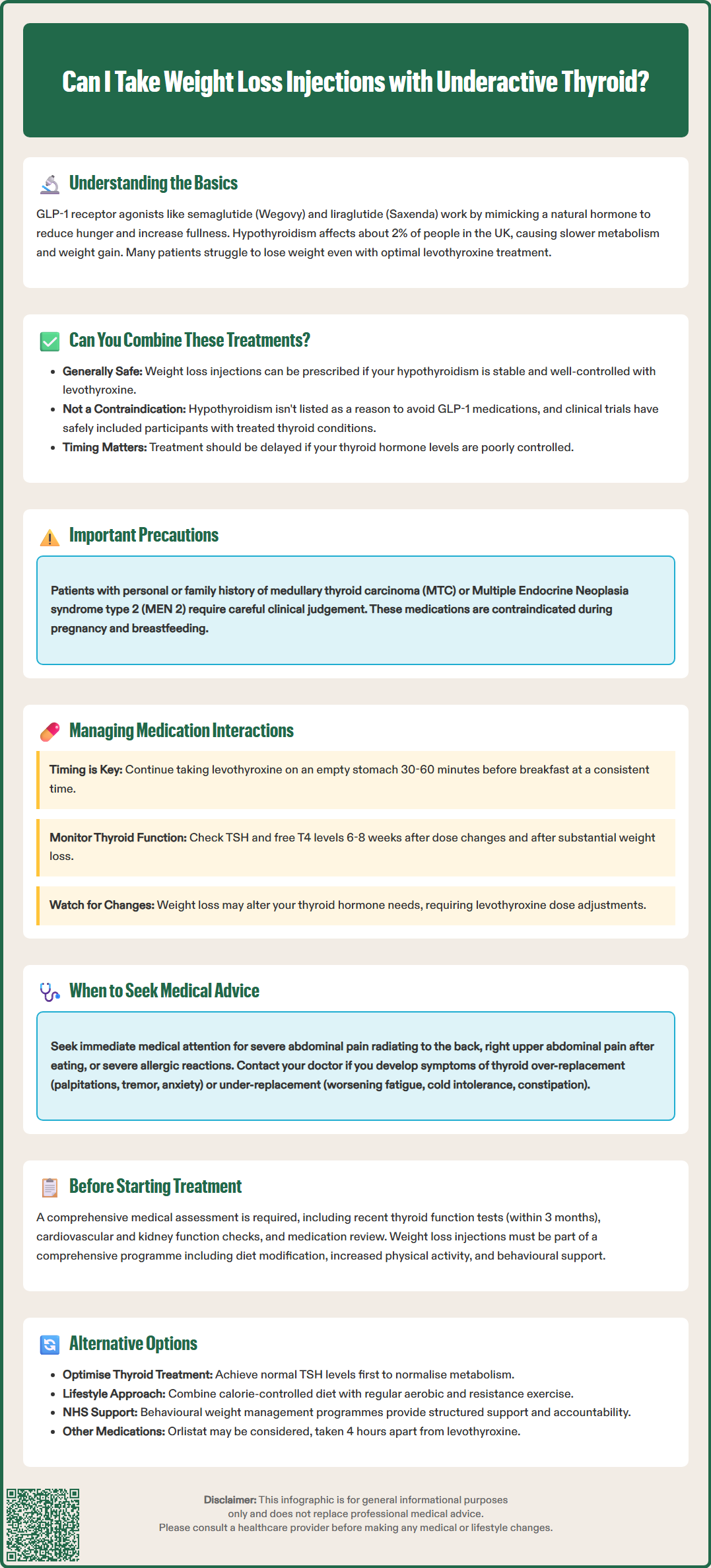
Quick Answer: Weight loss injections can generally be prescribed to patients with well-controlled hypothyroidism taking levothyroxine, as there is no absolute contraindication to using GLP-1 receptor agonists alongside thyroid hormone replacement therapy.
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are treatments for obesity management in the UK. These medications work by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone that regulates appetite and food intake. They slow gastric emptying, increase feelings of fullness, and reduce hunger signals to the brain, thereby facilitating weight reduction when combined with lifestyle modifications.
Underactive thyroid, or hypothyroidism, affects approximately 2% of the UK population according to NHS estimates. It occurs when the thyroid gland fails to produce sufficient thyroid hormones. These hormones—primarily thyroxine (T4) and triiodothyronine (T3)—play crucial roles in regulating metabolism, energy expenditure, and body weight. Diagnosis is based on biochemical testing (raised TSH, low free T4) alongside symptoms such as unexplained weight gain, fatigue, cold intolerance, and difficulty losing weight despite dietary efforts.
The relationship between hypothyroidism and weight management is complex. Whilst thyroid hormone deficiency does contribute to weight gain through reduced metabolic rate, the extent varies considerably between individuals. Many patients find that even with optimal thyroid hormone replacement therapy (typically levothyroxine), achieving and maintaining a healthy weight remains challenging. NICE guidance (NG145) emphasises that optimising levothyroxine treatment should be the first step before considering adjunctive weight management strategies.
For individuals with both obesity and hypothyroidism, understanding how these conditions interact—and whether weight loss medications can be safely used alongside thyroid treatment—is essential for making informed healthcare decisions. The interplay between thyroid function, metabolism, and weight loss pharmacotherapy requires careful medical consideration and monitoring.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe short answer is yes—weight loss injections can generally be prescribed to patients with well-controlled hypothyroidism, provided certain conditions are met. There is no absolute contraindication to using GLP-1 receptor agonists in individuals taking thyroid hormone replacement therapy. However, this decision must be made on an individual basis following thorough medical assessment.
The MHRA-approved prescribing information for semaglutide and liraglutide does not list hypothyroidism as a contraindication. Clinical trials of these medications, such as the STEP and SCALE programmes, have included participants with stable, treated thyroid conditions, though they typically excluded those with uncontrolled thyroid disease. Real-world evidence suggests they can be effective and safe when thyroid function is adequately managed. The key consideration is that your hypothyroidism must be stable and well-controlled with appropriate levothyroxine dosing before initiating weight loss treatment.
It's important to note that in the UK, the SmPCs for GLP-1 receptor agonists include precautionary information about thyroid C-cell tumours observed in rodent studies. While the human relevance remains uncertain, patients should be counselled to report any symptoms such as a neck mass, dysphagia, or persistent hoarseness. Clinical judgement should be exercised in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Additionally, if your hypothyroidism is poorly controlled—evidenced by abnormal thyroid function tests or ongoing symptoms—weight loss injections should typically be deferred until thyroid hormone levels are optimised. Uncontrolled thyroid disease can complicate weight management and may mask or exacerbate side effects from weight loss medications.
Importantly, GLP-1 receptor agonists are contraindicated during pregnancy and breastfeeding. Women of childbearing potential should use effective contraception while taking these medications, and treatment should be discontinued before planned conception (following specific SmPC guidance on washout periods). Your GP or endocrinologist should confirm stable thyroid function through recent blood tests (TSH, free T4) before prescribing weight loss injections.
GLP-1 receptor agonists and levothyroxine work through different mechanisms and are metabolised via separate pathways. Levothyroxine is absorbed in the small intestine and does not undergo significant hepatic metabolism, whilst GLP-1 agonists are protein-based medications broken down by proteolytic enzymes.
However, potential indirect interactions warrant consideration. GLP-1 receptor agonists slow gastric emptying, which could affect the absorption of oral medications including levothyroxine if taken simultaneously. The UK SmPCs for these products note that delayed gastric emptying may influence the absorption of concomitantly administered oral medicines. To minimise this potential issue, patients should continue following standard guidance for levothyroxine administration: take it on an empty stomach, typically 30–60 minutes before breakfast, and maintain consistent timing. Weight loss injections are usually administered weekly (semaglutide) or daily (liraglutide) and can be given at different times from thyroid medication.
As you lose weight with GLP-1 therapy, your thyroid hormone requirements may change. Weight loss can alter thyroid hormone metabolism and distribution, potentially necessitating adjustments to your levothyroxine dose. Some patients require dose reductions as they lose weight, whilst others may need increases. This underscores the importance of regular monitoring.
Monitoring recommendations should align with NICE guidance (NG145): check thyroid function tests (TSH and free T4) 6–8 weeks after any levothyroxine dose change, consider re-checking after substantial weight loss or if symptoms develop, and then every 6–12 months once stable. Signs requiring prompt medical review include palpitations, tremor, anxiety (suggesting over-replacement), or worsening fatigue, cold intolerance, or constipation (suggesting under-replacement). Your GP or endocrinologist will adjust levothyroxine dosing based on these results and your clinical presentation, aiming to maintain TSH within the reference range.
Before starting weight loss injections with hypothyroidism, a comprehensive medical assessment is essential. Your healthcare provider should review your complete medical history, current medications, thyroid function status, and weight management goals. Baseline investigations typically include recent thyroid function tests (ideally within the past 3 months), assessment of cardiovascular risk factors, renal function tests, and screening for relevant risk factors.
Patients should be aware of common side effects associated with GLP-1 receptor agonists, which include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These gastrointestinal effects are usually most pronounced during dose escalation and often improve with time. Starting with a low dose and gradually increasing, as per standard protocols, helps minimise these effects. Adequate hydration and dietary adjustments can also help manage symptoms. Severe gastrointestinal symptoms may lead to dehydration and acute kidney injury in susceptible individuals, so renal function monitoring may be appropriate for those with risk factors.
Serious but rare adverse effects require immediate medical attention. These include signs of pancreatitis (severe, persistent abdominal pain radiating to the back), gallbladder problems (right upper abdominal pain, particularly after eating), or severe allergic reactions. Patients should report any suspected side effects to their healthcare provider and can also report them directly to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
NICE guidance recommends that weight loss medications should only be prescribed as part of a comprehensive weight management programme including dietary modification, increased physical activity, and behavioural support. For semaglutide (Wegovy), NICE specifies that it should be prescribed within specialist weight management services for adults with a BMI of at least 35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) and at least one weight-related comorbidity.
Regular follow-up appointments—typically every 4–12 weeks initially—allow monitoring of weight loss progress, medication tolerance, and thyroid function. Treatment should be discontinued if you do not achieve the product-specific weight loss target (e.g., for liraglutide, <5% weight loss after 12 weeks at the 3.0 mg dose; for semaglutide, follow the Wegovy SmPC criteria), or if intolerable side effects develop.
For individuals with hypothyroidism who are not suitable candidates for weight loss injections, or who prefer alternative approaches, several evidence-based options exist. Optimising thyroid hormone replacement is the foundational step. Ensuring your levothyroxine dose achieves a TSH within the reference range, as recommended by NICE guidance (NG145), can help normalise metabolism and facilitate weight management. Some patients benefit from switching to combination T4/T3 therapy, though this remains controversial and is not routinely recommended by NICE.
Structured lifestyle interventions form the cornerstone of weight management for thyroid patients. A balanced, calorie-controlled diet emphasising whole foods, adequate protein intake, and reduced processed foods can be effective. Some patients with hypothyroidism find that addressing specific nutritional deficiencies may support overall wellbeing, though supplementation should only be undertaken following appropriate testing and medical advice. Routine supplementation with selenium, zinc, or vitamin D is not recommended unless deficiency is confirmed. Patients should avoid iodine/kelp supplements without specialist advice. Regular physical activity, combining both aerobic exercise and resistance training, helps preserve lean muscle mass and supports metabolic health.
Behavioural weight management programmes, such as those offered through NHS Tier 2 services or the NHS Digital Weight Management Programme, provide structured support, accountability, and education. These programmes can be particularly valuable for addressing emotional eating, establishing sustainable habits, and providing peer support. Cognitive behavioural therapy (CBT) approaches may help patients identify and modify unhelpful thoughts and behaviours around food and weight.
Pharmacological alternatives to GLP-1 agonists include orlistat, a lipase inhibitor that reduces dietary fat absorption. Orlistat is available both on prescription and over-the-counter in lower doses. Importantly, orlistat can reduce levothyroxine absorption, so doses should be separated by at least 4 hours, and thyroid function should be monitored. Orlistat requires adherence to a low-fat diet and can cause gastrointestinal side effects. For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not responded to other interventions, bariatric surgery may be considered according to NICE guidance. Procedures such as gastric bypass or sleeve gastrectomy can achieve substantial, sustained weight loss, though they require lifelong dietary modifications and monitoring, including careful attention to levothyroxine absorption post-surgery.
Regardless of the approach chosen, regular medical follow-up is essential for patients with hypothyroidism pursuing weight management. This ensures thyroid function remains optimised, allows early detection of any complications, and provides opportunity to adjust treatment strategies as needed. Patients should maintain realistic expectations, as weight loss may be slower for individuals with thyroid conditions compared to those without, even with optimal management.
GLP-1 receptor agonists and levothyroxine work through different mechanisms and are metabolised separately. However, weight loss injections slow gastric emptying, which could affect levothyroxine absorption if taken simultaneously, so continue taking thyroid medication on an empty stomach 30–60 minutes before breakfast as usual.
As you lose weight with GLP-1 therapy, your thyroid hormone requirements may change, potentially requiring levothyroxine dose adjustments. Regular thyroid function monitoring (TSH and free T4) every 6–12 months, or after substantial weight loss, allows your GP to optimise your dose based on results and symptoms.
Your healthcare provider should review recent thyroid function tests (TSH and free T4), ideally within the past 3 months, to confirm your hypothyroidism is stable and well-controlled before prescribing weight loss injections. Uncontrolled thyroid disease typically requires optimisation before starting GLP-1 therapy.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.