LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many individuals with hypothyroidism struggle with weight management due to the condition's impact on metabolism. Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have emerged as effective treatments for obesity in the UK. If you have hypothyroidism and are considering these medications, you can generally use them safely provided your thyroid function is well-controlled with levothyroxine. This article examines the compatibility of weight loss injections with hypothyroidism, important safety considerations, how thyroid conditions may influence treatment outcomes, and alternative weight management strategies available through the NHS and private services.
Quick Answer: Yes, individuals with hypothyroidism can generally have weight loss injections provided their thyroid function is well-controlled with levothyroxine and TSH levels are within the appropriate reference range.
Weight loss injections have become increasingly prominent in the management of obesity and weight-related conditions in the UK. The most commonly prescribed medications in this category are GLP-1 receptor agonists (glucagon-like peptide-1), including semaglutide (marketed as Wegovy for weight management) and liraglutide (Saxenda). These medications work by mimicking natural hormones that regulate appetite and blood glucose levels, helping individuals feel fuller for longer and reducing overall calorie intake.
Hypothyroidism is a condition where the thyroid gland produces insufficient thyroid hormones—primarily thyroxine (T4) and triiodothyronine (T3). These hormones are crucial for regulating metabolism, energy expenditure, and numerous bodily functions. When thyroid hormone levels are low, individuals often experience symptoms including fatigue, cold intolerance, dry skin, constipation, and notably, unexplained weight gain or difficulty losing weight. This metabolic slowdown makes weight management particularly challenging for people with hypothyroidism.
The connection between hypothyroidism and weight difficulties is well-established. The reduced metabolic rate means the body burns fewer calories at rest, and fluid retention can contribute to weight increase. Many patients with hypothyroidism find that despite dietary modifications and increased physical activity, achieving meaningful weight loss remains frustratingly difficult. This has led to growing interest in whether weight loss injections might offer additional support for this patient group, particularly when conventional approaches have proven insufficient. Understanding both conditions is essential before considering combined treatment approaches.
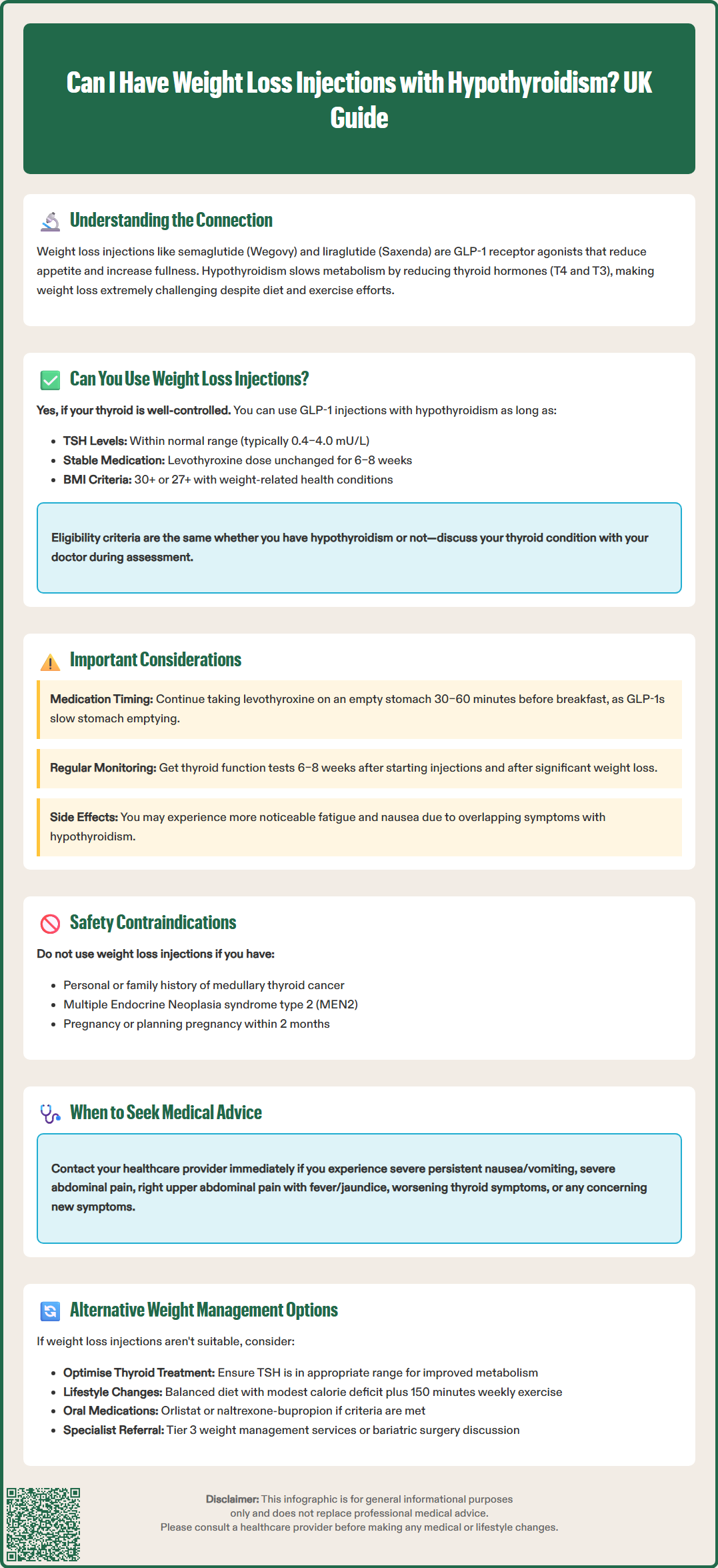
Yes, individuals with hypothyroidism can generally have weight loss injections, provided their thyroid condition is well-controlled with appropriate medication. There is no absolute contraindication to using GLP-1 receptor agonists in patients with hypothyroidism, and these medications work through different pathways than thyroid hormone replacement therapy (levothyroxine).
However, several important considerations apply. Firstly, your thyroid function must be optimised before initiating weight loss treatment. This means your thyroid-stimulating hormone (TSH) levels should be within your local laboratory reference range (typically around 0.4–4.0 mU/L, with some clinicians aiming for 0.4–2.5 mU/L in younger adults), and you should be on a stable dose of levothyroxine for at least 6–8 weeks. Attempting weight loss interventions whilst thyroid function remains poorly controlled is unlikely to be effective and may complicate clinical management.
While GLP-1 receptor agonists are licensed in the UK for:
Body mass index (BMI) of 30 kg/m² or above, or
BMI of 27 kg/m² or above with weight-related comorbidities (such as type 2 diabetes or hypertension)
It's important to note that NHS-funded access is more restricted, following NICE technology appraisals. These medications are typically available through NHS specialist weight management services (tier 3) when:
Specific BMI thresholds are met (often higher than licensing criteria)
Weight-related comorbidities are present
Lifestyle interventions alone have been insufficient
Eligibility criteria remain the same for people with hypothyroidism as for the general population. Your GP or specialist will assess whether weight loss injections are appropriate based on your overall health status, current medications, and treatment goals. It's essential to have an open discussion about your thyroid condition during this assessment to ensure safe and effective treatment planning.
Hypothyroidism can influence both the effectiveness and experience of weight loss treatment in several ways. Even with optimised thyroid hormone replacement, some individuals may experience differences in their metabolic response to weight management interventions compared to those without thyroid conditions.
The mechanism of action of weight loss injections works independently of thyroid hormone pathways. GLP-1 receptor agonists primarily affect appetite regulation through the central nervous system and slow gastric emptying, which are processes not directly controlled by thyroid hormones. However, the overall metabolic context created by hypothyroidism means the body's energy expenditure baseline may be different, potentially influencing individual weight loss outcomes.
Medication considerations are important to note. While there is no direct pharmacological interaction between injectable GLP-1 receptor agonists and levothyroxine, the delayed gastric emptying caused by these medications could potentially affect the absorption of levothyroxine. Additionally, the SmPC for oral semaglutide (Rybelsus, licensed for diabetes, not weight management) notes increased levothyroxine exposure. For these reasons, it's advisable to:
Maintain the standard practice of taking levothyroxine on an empty stomach, typically 30–60 minutes before breakfast
Take levothyroxine consistently at the same time each day
Have thyroid function tests (TFTs) checked 6–8 weeks after starting GLP-1 therapy and after significant weight loss, as your levothyroxine requirements may change
Patients with hypothyroidism may also experience overlapping side effects. Both conditions can cause fatigue, and the initial side effects of GLP-1 medications (nausea, reduced appetite, tiredness) might be more noticeable. Close monitoring during the initial treatment phase is therefore particularly important for this patient group.
Before starting weight loss injections with hypothyroidism, a comprehensive medical assessment is essential. Your healthcare provider will need to evaluate several factors to ensure treatment safety and appropriateness.
Thyroid function monitoring should include recent blood tests showing:
TSH levels within your local laboratory reference range (typically around 0.4–4.0 mU/L)
Free T4 (thyroxine) levels, if previously abnormal
Confirmation of stable levothyroxine dosing for at least 6–8 weeks
Your doctor will also assess for contraindications to GLP-1 receptor agonists, which include personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN2). Whilst these are rare conditions, they represent absolute contraindications to this class of medication. There is no evidence that having hypothyroidism itself increases the risk of these conditions, but the assessment must be thorough.
Additional safety considerations include:
Pregnancy and contraception: GLP-1 receptor agonists are contraindicated in pregnancy and should be discontinued at least 2 months before planned conception for semaglutide
Kidney function tests, though GLP-1 receptor agonists generally don't require dose adjustment in renal impairment
Assessment for diabetic retinopathy if you have diabetes
Review of all current medications, particularly insulin or sulfonylureas which may increase hypoglycaemia risk when combined with GLP-1 receptor agonists
Evaluation of cardiovascular health and gallbladder disease risk
Ongoing monitoring is crucial once treatment begins. You should expect:
Regular weight and BMI measurements
Periodic thyroid function tests (typically 6–8 weeks after starting GLP-1 therapy, after significant weight loss, and then every 6–12 months)
Assessment of side effects and treatment tolerance
Review of overall health status and comorbidities
When to seek medical advice: Contact your GP promptly if you experience severe or persistent nausea and vomiting, signs of pancreatitis (severe abdominal pain), right upper abdominal pain with fever or jaundice (possible gallbladder disease), symptoms suggesting worsening thyroid function, or any concerning new symptoms. Suspected side effects should be reported via the MHRA Yellow Card scheme. Regular follow-up appointments are essential to ensure both your thyroid condition and weight management remain optimally controlled.
For individuals with hypothyroidism who are not suitable candidates for weight loss injections, or who prefer alternative approaches, several evidence-based strategies can support effective weight management.
Optimising thyroid hormone replacement is the foundational step. Some patients may benefit from dose adjustments to ensure TSH is within the appropriate range. Combination therapy with T3 (liothyronine) alongside T4 (levothyroxine) is not routinely recommended by NICE (NG145) but may be considered in specific circumstances by specialists. Ensuring your thyroid medication is optimally dosed can significantly improve metabolic function and make weight loss more achievable.
Structured lifestyle interventions remain the cornerstone of weight management. For people with hypothyroidism, this includes:
Dietary modifications: A balanced, calorie-controlled diet rich in whole foods, vegetables, lean proteins, and complex carbohydrates. Some individuals find that reducing processed foods and managing portion sizes yields better results. There is no specific "hypothyroid diet", but ensuring adequate nutrition whilst creating a modest calorie deficit is key.
Regular physical activity: Aim for at least 150 minutes of moderate-intensity exercise weekly, as recommended by UK Chief Medical Officers. Resistance training can be particularly beneficial for building muscle mass, which helps increase metabolic rate.
Behavioural support: NHS-funded weight management programmes offer structured support including dietary advice, physical activity guidance, and behavioural strategies. The NHS Digital Weight Management Programme is available for eligible patients with specific conditions such as hypertension or type 2 diabetes.
Pharmacological alternatives to injectable medications include orlistat, a lipase inhibitor that reduces fat absorption from the diet. This medication may be prescribed when BMI criteria are met and is taken orally rather than by injection. Naltrexone-bupropion (Mysimba) is another licensed option in the UK, though it is not routinely funded by the NHS.
Specialist referral may be appropriate if weight management remains challenging despite optimised thyroid treatment and lifestyle interventions. Tier 3 weight management services can provide multidisciplinary support, and in cases of severe obesity with complications, bariatric surgery might be considered following NICE guidelines (CG189). Always discuss your individual circumstances with your healthcare provider to determine the most appropriate approach for your situation.
There is no direct pharmacological interaction between GLP-1 receptor agonists and levothyroxine. However, delayed gastric emptying caused by these medications may affect levothyroxine absorption, so continue taking thyroid medication on an empty stomach 30–60 minutes before breakfast and have thyroid function tests checked 6–8 weeks after starting treatment.
GLP-1 receptor agonists can be effective for people with hypothyroidism, particularly when thyroid function is optimised with levothyroxine. Individual responses may vary due to metabolic differences, but the medications work through appetite regulation pathways independent of thyroid hormones.
NHS eligibility for weight loss injections follows NICE guidance and is typically available through specialist weight management services (tier 3) when specific BMI thresholds are met alongside weight-related comorbidities. Having hypothyroidism does not change these eligibility criteria, though your thyroid condition must be well-controlled before treatment can begin.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.