
Many women approaching or experiencing menopause are exploring both hormone replacement therapy (HRT) and weight loss injections to manage different aspects of their health. The question of whether you can take HRT with weight loss injections is increasingly common, particularly as newer medications such as semaglutide (Wegovy) and liraglutide (Saxenda) become more widely available. In most cases, these treatments can be safely combined under proper medical supervision, as there is no absolute contraindication preventing their concurrent use. However, both affect metabolic and hormonal processes, making individualised assessment and careful monitoring essential for safe, effective treatment.
Quick Answer: HRT and weight loss injections can generally be taken together safely under medical supervision, as there are no direct contraindications between hormone replacement therapy and GLP-1 receptor agonists.
Many women approaching or experiencing menopause are exploring both hormone replacement therapy (HRT) and weight loss injections to manage different aspects of their health. The question of whether these treatments can be safely combined is increasingly common, particularly as newer weight loss medications become more widely available through the NHS and private prescribers.
The short answer is that, in most cases, HRT and weight loss injections can be taken together, but this decision must be made on an individual basis with proper medical supervision. There is no absolute contraindication preventing their concurrent use, and UK product information does not specifically prohibit this combination. However, both treatments affect metabolic and hormonal processes, which means careful monitoring is essential.
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), work through different mechanisms than HRT. Whilst HRT replaces declining oestrogen and progesterone levels, weight loss injections primarily affect appetite regulation and glucose metabolism.
It's important to note that on the NHS, GLP-1 receptor agonists for weight management are only available through specialist weight management services for people meeting specific NICE criteria. These medications are also contraindicated during pregnancy and breastfeeding, and effective contraception is advised during treatment.
This article examines the mechanisms of both treatments, explores potential interactions, discusses safety considerations, and outlines the important conversations you should have with your GP before embarking on combined treatment. Understanding how these medications work individually and together will help you make informed decisions about your healthcare.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereHormone Replacement Therapy (HRT) works by supplementing the body's declining levels of oestrogen and, where appropriate, progesterone during perimenopause and menopause. Oestrogen can be delivered through various routes including tablets, patches, gels, or sprays, whilst progesterone (or progestogens) is typically given as tablets or via the Mirena intrauterine system. Combined patches contain both oestrogen and progestogen. The primary aim is to alleviate menopausal symptoms such as hot flushes, night sweats, mood changes, and vaginal dryness, whilst also providing protection against osteoporosis.
Oestrogen influences numerous bodily systems beyond reproductive function. It affects cardiovascular health, bone density, cognitive function, and metabolic processes including fat distribution and insulin sensitivity. During menopause, hormonal changes can make weight management more challenging for some women, though HRT itself is not a weight loss treatment.
Weight loss injections approved in the UK primarily belong to the GLP-1 receptor agonist class. Semaglutide (Wegovy) and liraglutide (Saxenda) mimic the action of glucagon-like peptide-1, a naturally occurring hormone that regulates appetite and blood sugar levels. These medications work by:
Slowing gastric emptying, which prolongs feelings of fullness
Acting on appetite centres in the brain to reduce hunger
Improving insulin secretion and reducing glucagon release
These injections are administered subcutaneously, typically once weekly (semaglutide) or once daily (liraglutide). They were originally developed for type 2 diabetes management but are now licensed for weight management in individuals with a BMI of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities.
On the NHS, access to these medications is restricted to patients meeting specific NICE criteria (TA875 for semaglutide, TA664 for liraglutide) and is typically provided through specialist weight management services. Treatment must be part of a comprehensive weight management programme including dietary modification and increased physical activity.
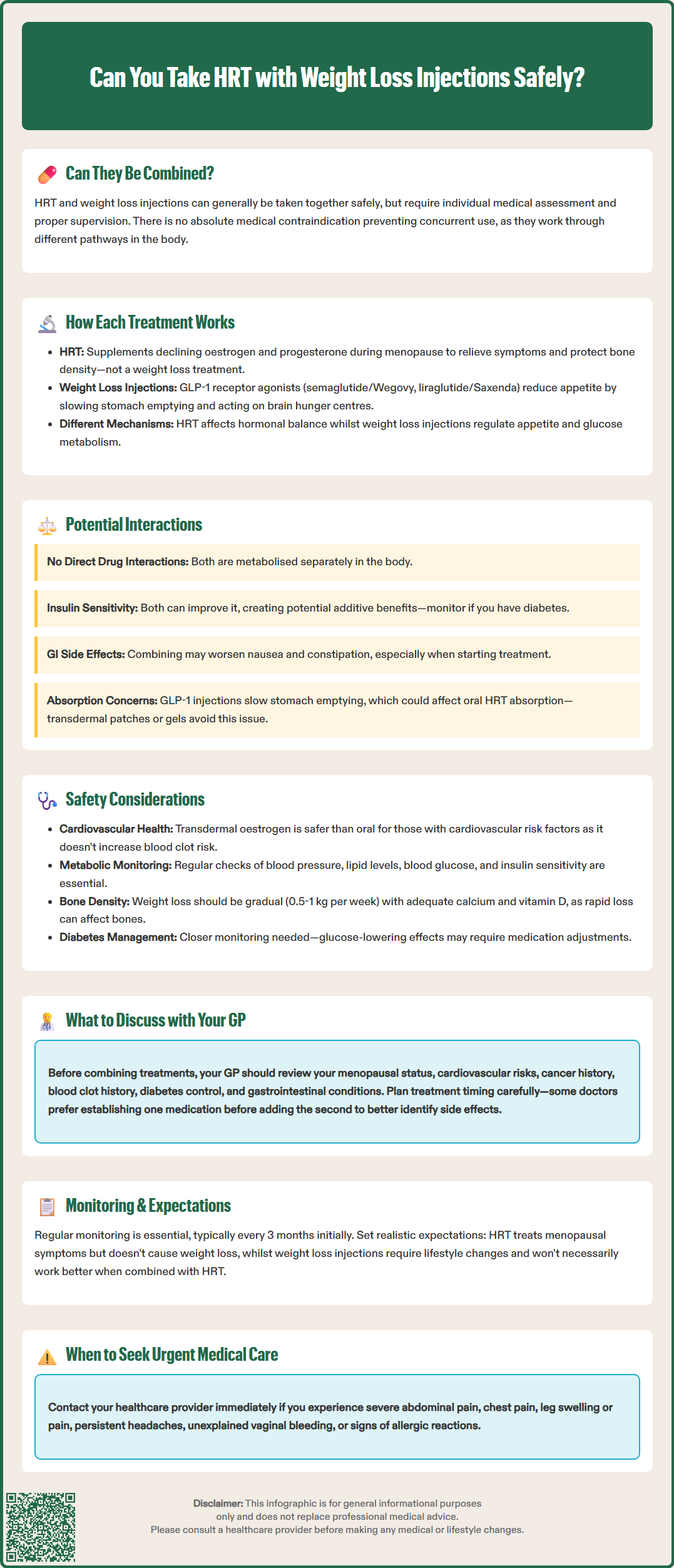
Currently, there is no official evidence of direct pharmacological interactions between HRT and GLP-1 receptor agonist weight loss injections. These medications work through distinct pathways: HRT primarily affects hormone receptors throughout the body, whilst weight loss injections target GLP-1 receptors in the gut, pancreas, and brain. They are metabolised differently, with minimal overlap in their pharmacokinetic profiles.
However, indirect interactions warrant consideration. Both treatments can influence metabolic parameters, though in different ways. HRT may improve insulin sensitivity in some women, particularly when oestrogen is delivered transdermally (through patches or gels), which avoids first-pass liver metabolism. Weight loss injections also improve insulin sensitivity and glycaemic control. When combined, these effects could theoretically be additive, which is generally beneficial but requires monitoring, especially in women with diabetes or prediabetes.
Gastrointestinal effects represent another consideration. Weight loss injections commonly cause nausea, particularly during dose escalation, and can lead to reduced appetite, constipation, or diarrhoea. Some women also experience gastrointestinal symptoms when starting HRT, though these are generally less pronounced. Taking both medications simultaneously, especially when initiating treatment, could potentially compound digestive discomfort.
The absorption of oral medications can be affected by the delayed gastric emptying caused by GLP-1 agonists, as noted in the UK product information. For women taking oral HRT preparations, this could theoretically alter absorption patterns. Transdermal HRT (patches or gels) bypasses the digestive system entirely, eliminating this potential concern and may be preferable when using GLP-1 receptor agonists.
If you're considering combined treatment, it may be beneficial to establish one treatment before introducing the second, allowing clearer assessment of individual responses and side effects. This approach can help identify which medication might be responsible for any adverse effects.
Cardiovascular considerations are paramount when combining these treatments. HRT carries varying cardiovascular risks depending on factors including age at initiation, time since menopause, route of administration, and individual risk factors. Women who start HRT before age 60 or within 10 years of menopause generally have a favourable benefit-risk profile. Transdermal oestrogen is preferred for women with cardiovascular risk factors as it doesn't increase clotting risk like oral preparations.
Weight loss injections have demonstrated cardiovascular outcomes in clinical trials, with semaglutide showing reduced risk of major adverse cardiovascular events in certain populations. However, these medications can increase heart rate modestly, and rare cases of acute pancreatitis have been reported. When combining treatments, your cardiovascular risk profile requires comprehensive assessment, including blood pressure, lipid levels, and any history of thromboembolism.
Metabolic monitoring becomes particularly important with combined therapy. Both treatments can affect:
Blood glucose levels and insulin sensitivity
Lipid profiles (cholesterol and triglycerides)
Body composition and fat distribution
Women with diabetes or prediabetes require closer monitoring, as the glucose-lowering effects of weight loss injections combined with HRT's metabolic influences may necessitate adjustments to other medications, particularly insulin or sulphonylureas. Those with diabetic retinopathy should be monitored carefully, as rapid improvement in glucose control can temporarily worsen retinopathy.
Bone health considerations also apply. Whilst HRT protects against osteoporosis, rapid weight loss can potentially affect bone density. NHS advice suggests that healthy weight loss should be gradual (0.5-1 kg per week) to minimise adverse effects. Women combining these treatments should ensure adequate calcium and vitamin D intake and may benefit from bone density monitoring, particularly if other risk factors for osteoporosis exist.
Additional safety considerations for GLP-1 receptor agonists include:
Gallbladder disease: These medications may increase the risk of gallstones and cholecystitis
Dehydration: Gastrointestinal side effects can lead to dehydration and potential acute kidney injury
Pregnancy/breastfeeding: GLP-1 receptor agonists are contraindicated during pregnancy and breastfeeding, and should be discontinued well before planned conception
Contraindications for either treatment must be respected. HRT is contraindicated in women with current or previous breast cancer (with some exceptions), active liver disease, unexplained vaginal bleeding, or untreated endometrial hyperplasia. These contraindications remain absolute regardless of combination therapy.
Before combining HRT with weight loss injections, a comprehensive medical assessment is essential. Your GP should review your complete medical history, including:
Menopausal status and symptom severity
Current weight, BMI, and weight loss goals
Cardiovascular risk factors (blood pressure, cholesterol, smoking status, family history)
Personal or family history of breast cancer, ovarian cancer, or endometrial cancer
History of venous thromboembolism or stroke
Diabetes status and glycaemic control
Thyroid function and any thyroid disorders
Gastrointestinal conditions, particularly gastroparesis or inflammatory bowel disease
Current medications and potential drug interactions
Previous experience with either HRT or weight loss treatments
Pregnancy status or plans for conception
Timing and sequencing of treatment initiation should be discussed. Some clinicians prefer to establish one treatment before introducing the second, allowing clearer assessment of individual responses and side effects. This approach can help identify which medication might be responsible for any adverse effects. Alternatively, if you're already stable on one treatment, adding the second may be straightforward with appropriate monitoring.
Monitoring plans should be clearly established, including:
Frequency of follow-up appointments (typically 3-monthly initially)
Blood tests to monitor metabolic parameters, liver function, and lipid profiles
Blood pressure monitoring
Assessment of symptom control for menopausal symptoms
Weight loss progress and body composition changes
Screening for adverse effects from either medication
Review of treatment response against NICE criteria for continuing GLP-1 receptor agonists (e.g., minimum weight loss targets at specific timepoints)
Realistic expectations about outcomes should be discussed. HRT effectively manages menopausal symptoms but is not a weight loss treatment. Weight loss injections can produce significant weight reduction but require commitment to lifestyle changes. The combination won't necessarily produce additive weight loss effects, as HRT's metabolic benefits are distinct from the appetite-suppressing effects of GLP-1 agonists.
Your GP should also discuss when to seek urgent medical attention, including signs of:
Severe abdominal pain (potential pancreatitis or gallbladder disease)
Chest pain or severe breathlessness
Leg pain, swelling, or redness (potential thrombosis)
Severe persistent headaches or visual disturbances
Unexplained vaginal bleeding (which requires urgent 2-week-wait referral pathway)
Severe allergic reactions
Right upper abdominal pain, fever, or jaundice (potential gallbladder disease)
Finally, ensure you understand the costs and availability of both treatments. HRT is available on NHS prescription, whilst weight loss injections may be available through NHS specialist weight management services for eligible patients or via private prescription. Discuss the sustainability of treatment, as both may require long-term use to maintain benefits, and consider how this fits with your personal circumstances and healthcare goals.
Any suspected side effects from either medication should be reported through the MHRA Yellow Card scheme.
There are no direct pharmacological interactions between HRT and GLP-1 receptor agonist weight loss injections, as they work through different pathways. However, both treatments affect metabolic processes, so comprehensive medical assessment and regular monitoring are essential to ensure safe combined use.
Many clinicians prefer to establish one treatment before introducing the second, allowing clearer assessment of individual responses and side effects. This approach helps identify which medication might be responsible for any adverse effects, though starting both simultaneously may be appropriate in certain circumstances with close monitoring.
Yes, combined treatment requires regular monitoring including blood pressure checks, metabolic parameters (glucose and lipid profiles), assessment of menopausal symptom control, and screening for adverse effects. Follow-up appointments are typically recommended every three months initially, with adjustments based on individual response.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.