Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst gastrointestinal side effects such as nausea, diarrhoea, and abdominal discomfort are common with Wegovy treatment, concerns occasionally arise about whether the medication can cause colitis—inflammation of the colon. Understanding the distinction between expected gastrointestinal reactions and inflammatory bowel conditions is essential for patients and healthcare professionals. This article examines the evidence linking Wegovy to colitis, explores common digestive side effects, and provides guidance on when to seek medical advice.
Quick Answer: There is currently no established causal link between Wegovy (semaglutide) and colitis in UK regulatory guidance, clinical trials, or post-marketing surveillance data.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. The Medicines and Healthcare products Regulatory Agency (MHRA) approved Wegovy following clinical trials demonstrating significant weight reduction when combined with lifestyle modifications.
In the UK, semaglutide 2.4 mg is recommended by NICE (TA875) for use within specialist weight management services with scheduled monitoring. The mechanism of action of semaglutide involves mimicking the naturally occurring GLP-1 hormone, which regulates appetite and food intake. By binding to GLP-1 receptors in the brain, Wegovy reduces hunger signals and increases feelings of fullness. Additionally, it slows gastric emptying—the rate at which food leaves the stomach—which contributes to prolonged satiety but also accounts for many of its gastrointestinal effects.
Gastrointestinal side effects are amongst the most commonly reported adverse reactions with Wegovy treatment. Clinical trial data reveals that nausea, diarrhoea, vomiting, constipation, and abdominal pain affect a substantial proportion of patients, particularly during dose escalation. These effects typically occur because GLP-1 receptor agonists directly influence gastrointestinal motility and secretion throughout the digestive tract.
The prescribing information for Wegovy emphasises a gradual dose titration schedule specifically designed to minimise gastrointestinal tolerability issues. Patients begin with a 0.25 mg weekly dose, increasing incrementally over 16–20 weeks to reach the maintenance dose of 2.4 mg. Some patients may remain on the 1.7 mg dose if the 2.4 mg dose is not tolerated, as permitted in the Summary of Product Characteristics (SmPC). This approach allows the digestive system to adapt progressively to the medication's effects. Understanding these common gastrointestinal reactions is essential for patients and healthcare professionals to distinguish expected side effects from potentially more serious conditions.
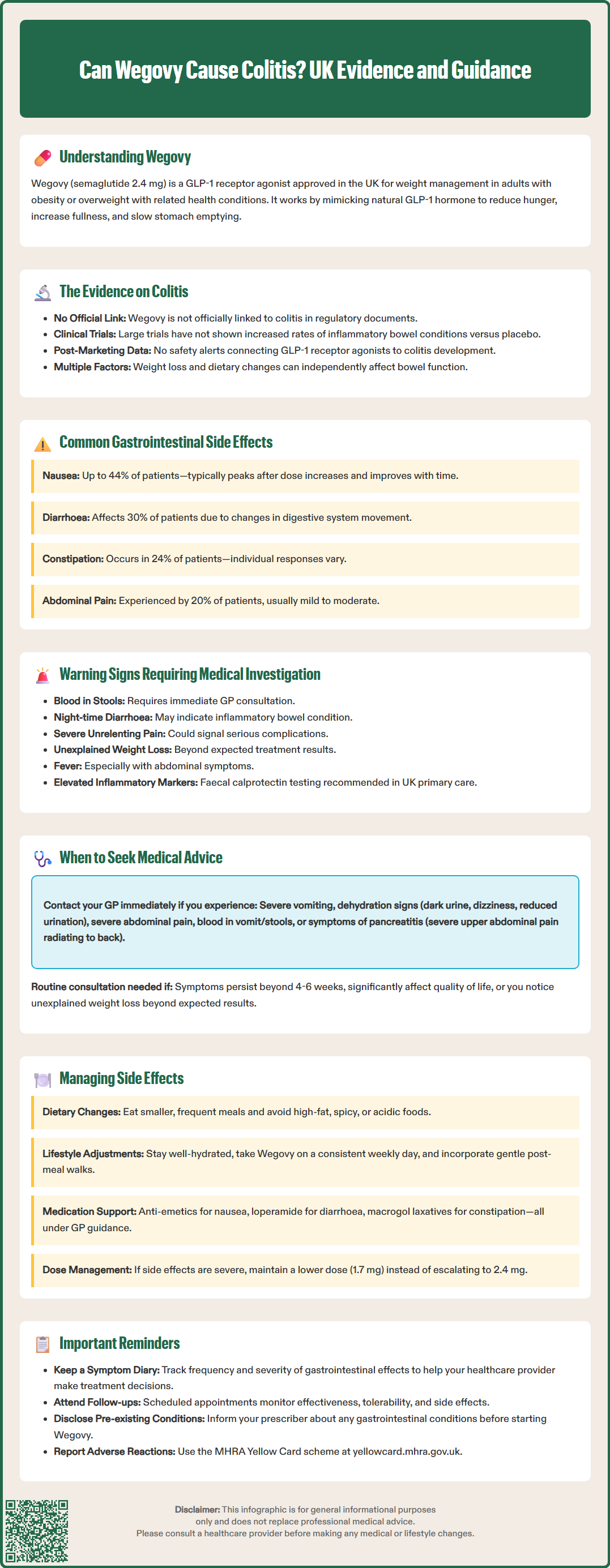
There is currently no established causal association between Wegovy and colitis in the Wegovy SmPC, EMA assessment, or NICE guidance. Colitis—inflammation of the colon—encompasses various conditions including ulcerative colitis, Crohn's disease affecting the colon, microscopic colitis, and infectious or ischaemic colitis. None of these conditions are listed as recognised adverse effects in the Wegovy Summary of Product Characteristics approved by the MHRA or European Medicines Agency (EMA).
Clinical trials involving thousands of participants receiving semaglutide for weight management have not identified colitis as a treatment-emergent adverse event. The STEP (Semaglutide Treatment Effect in People with obesity) trial programme, which formed the basis for Wegovy's approval, documented gastrointestinal symptoms extensively but did not report increased incidence of inflammatory bowel conditions compared to placebo groups.
Post-marketing surveillance and pharmacovigilance systems continuously monitor for unexpected adverse reactions following medication approval. While isolated case reports may exist in post-marketing surveillance, regulatory authorities have not issued safety alerts linking GLP-1 receptor agonists to colitis development. Healthcare professionals should remain vigilant and report any suspected adverse reactions to the MHRA via the Yellow Card scheme (yellowcard.mhra.gov.uk).
Patients with pre-existing inflammatory bowel disease may experience symptom fluctuations for various reasons, including disease activity, dietary changes, stress, or concurrent medications. Weight loss itself can influence gastrointestinal function, and the dietary modifications accompanying Wegovy treatment may independently affect bowel habits. If colitis symptoms develop during Wegovy treatment, a thorough clinical evaluation is necessary to identify the underlying cause rather than automatically attributing symptoms to the medication.
In the UK, the diagnostic approach typically includes faecal calprotectin testing (as per NICE DG11) to distinguish between inflammatory and functional bowel disorders in primary care, alongside blood tests and stool examinations. Gastroenterological referral and further investigations such as colonoscopy may be warranted to establish an accurate diagnosis if inflammatory markers are elevated or symptoms persist.
The most frequently reported gastrointestinal side effects of Wegovy include nausea (affecting up to 44% of patients), diarrhoea (approximately 30%), vomiting (24%), constipation (24%), and abdominal pain (20%), according to the Wegovy SmPC and STEP trial data. These typically represent mild to moderate severity, with most symptoms improving over time as the body adjusts to treatment.
Nausea usually peaks during the first few weeks following dose increases and often diminishes with continued treatment. Patients describe sensations ranging from mild queasiness to significant nausea that may interfere with eating. This effect results from delayed gastric emptying and central nervous system effects on appetite regulation centres.
Diarrhoea and altered bowel habits occur due to changes in gastrointestinal motility and fluid secretion. Some patients experience loose stools or increased bowel frequency, whilst others develop constipation. These opposing effects reflect individual variation in how the digestive system responds to GLP-1 receptor stimulation. Wegovy-related diarrhoea is generally watery, intermittent, and not associated with blood or inflammatory markers.
Abdominal discomfort may manifest as cramping, bloating, or generalised pain, typically related to delayed gastric emptying and altered intestinal transit. This differs from colitis-associated pain, which often localises to the lower abdomen and may be relieved temporarily by bowel movements.
Distinguishing features that suggest inflammatory bowel conditions rather than expected Wegovy side effects include:
Blood in stools (though some forms of colitis, such as microscopic colitis, typically present with persistent non-bloody diarrhoea)
Persistent nocturnal diarrhoea disrupting sleep
Severe, unremitting abdominal pain
Unintentional weight loss beyond expected therapeutic effects
Fever accompanying gastrointestinal symptoms
Elevated inflammatory markers (CRP, ESR) or faecal calprotectin
Progressive worsening rather than improvement over time
Recognising these distinctions enables appropriate clinical decision-making regarding symptom management versus further investigation. In the UK, faecal calprotectin testing (NICE DG11) is recommended in primary care to help distinguish between inflammatory and functional bowel disorders.
Patients should contact their GP or prescribing clinician promptly if they experience severe or persistent gastrointestinal symptoms whilst taking Wegovy. Whilst mild nausea and altered bowel habits are anticipated, certain presentations warrant urgent medical evaluation to exclude serious complications or alternative diagnoses.
Immediate medical attention is necessary for:
Severe, persistent vomiting preventing adequate fluid or medication intake, which may lead to dehydration and electrolyte disturbances
Signs of dehydration including reduced urination, dark urine, dizziness, confusion, or extreme thirst
Severe abdominal pain, particularly if sudden onset, progressively worsening, or accompanied by abdominal rigidity
Blood in vomit or stools, which may indicate gastrointestinal bleeding requiring urgent investigation
Symptoms suggesting pancreatitis, such as severe upper abdominal pain radiating to the back, as GLP-1 receptor agonists carry a small risk of acute pancreatitis. The Wegovy SmPC advises that semaglutide should be discontinued if pancreatitis is suspected
Signs of gallbladder disease including right upper quadrant pain, fever, or jaundice, as GLP-1 receptor agonists and weight loss can increase the risk of gallstones
Routine GP consultation is advisable for:
Gastrointestinal symptoms persisting beyond 4–6 weeks without improvement
Symptoms significantly impacting quality of life or nutritional intake
Unexplained weight loss exceeding expected therapeutic effects
New onset of symptoms differing from initial side effects
Concerns about symptom severity or medication tolerability
NICE guidance on obesity management (TA875) emphasises the importance of regular monitoring during pharmacological weight management interventions. Patients prescribed Wegovy should have scheduled follow-up appointments to assess treatment response, tolerability, and adverse effects. These consultations provide opportunities to discuss gastrointestinal symptoms and determine whether dose adjustment, temporary treatment interruption, or additional investigation is appropriate.
Patients with pre-existing gastrointestinal conditions, including inflammatory bowel disease, should inform their prescriber before starting Wegovy, as baseline symptoms may complicate assessment of treatment-related effects. Collaborative care between weight management services and gastroenterology specialists may be beneficial in such cases to optimise both conditions safely.
Any suspected adverse reactions to Wegovy should be reported to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
Effective management strategies can significantly improve tolerability of Wegovy and reduce the impact of gastrointestinal side effects. Healthcare professionals typically recommend a combination of dietary modifications, lifestyle adjustments, and symptomatic treatments to support patients through the initial treatment period.
Dietary modifications form the cornerstone of symptom management:
Eat smaller, more frequent meals rather than large portions, which accommodates delayed gastric emptying
Avoid high-fat foods, as these slow digestion further and may exacerbate nausea
Limit spicy, acidic, or heavily seasoned foods that may irritate the digestive system
Stay well-hydrated with water throughout the day, particularly important if experiencing diarrhoea
Identify and avoid personal trigger foods that worsen symptoms
Eat slowly and chew thoroughly to aid digestion and reduce bloating
Practical lifestyle measures include:
Taking Wegovy once weekly on a consistent day (the time of day is not critical, per the SmPC)
Avoiding lying down immediately after eating to prevent reflux and nausea
Gentle physical activity, such as short walks after meals, to support digestion
Stress management techniques, as anxiety can exacerbate gastrointestinal symptoms
Pharmacological interventions may be appropriate for persistent symptoms, but should be used under GP direction:
Domperidone has cardiac risk (QT prolongation) and specific contraindications; MHRA advises restricted use
Loperamide for diarrhoea management when appropriate, but should be avoided if blood in stools, fever, or suspected inflammatory/infectious diarrhoea
Laxatives for constipation, with macrogol (polyethylene glycol) preparations typically first-line in UK practice, alongside optimising dietary fibre and hydration
Dose adjustment strategies include temporarily maintaining a lower dose if gastrointestinal side effects are problematic, allowing additional time for adaptation before escalation. The SmPC permits maintenance at 1.7 mg if 2.4 mg is not tolerated. In some cases, treatment interruption followed by reinitiation at a lower dose may be necessary.
Communication with healthcare providers is essential throughout treatment. Patients should maintain symptom diaries documenting the nature, frequency, and severity of gastrointestinal effects, which assists clinical decision-making regarding treatment continuation, modification, or cessation. The balance between therapeutic benefit and tolerability requires individualised assessment, and not all patients will tolerate the full maintenance dose of Wegovy despite management strategies.
No, colitis is not listed as a recognised adverse effect in the Wegovy Summary of Product Characteristics approved by the MHRA or in clinical trial data. Regulatory authorities have not issued safety alerts linking GLP-1 receptor agonists to colitis development.
The most common gastrointestinal side effects include nausea (up to 44%), diarrhoea (30%), vomiting (24%), constipation (24%), and abdominal pain (20%). These typically improve over time as the body adjusts to treatment.
Seek immediate medical attention for severe persistent vomiting, blood in stools or vomit, severe abdominal pain, signs of dehydration, or symptoms suggesting pancreatitis. Contact your GP for symptoms persisting beyond 4–6 weeks or significantly impacting quality of life.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.