
Many people with Hashimoto's thyroiditis who develop type 2 diabetes wonder whether Ozempic (semaglutide) is a safe treatment option for them. Hashimoto's disease, the most common cause of hypothyroidism in the UK, affects thyroid hormone production and metabolism, whilst Ozempic is a GLP-1 receptor agonist licensed for managing type 2 diabetes. Understanding how these conditions interact is essential for safe, effective treatment. This article explores the relationship between Hashimoto's and Ozempic, examining safety considerations, potential interactions with thyroid medication, and when to seek medical advice for combined management of both conditions.
Quick Answer: Hashimoto's thyroiditis is not an absolute contraindication to Ozempic, and many patients with well-controlled thyroid disease can safely use semaglutide under medical supervision.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone that regulates blood sugar levels and appetite.
The medication works through several complementary mechanisms. Primarily, semaglutide stimulates insulin secretion from pancreatic beta cells when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. This dual action helps maintain more stable glycaemic control throughout the day. Additionally, Ozempic slows gastric emptying, meaning food remains in the stomach longer, which contributes to increased satiety and reduced appetite.
Ozempic is administered as a once-weekly subcutaneous injection, starting at 0.25 mg for 4 weeks (initiation dose only), then increasing to 0.5 mg. The dose may be increased to 1 mg after at least 4 weeks, and to 2 mg after at least another 4 weeks if needed for glycaemic control. The MHRA has licensed it as an adjunct to diet and exercise for adults with type 2 diabetes, either as monotherapy when metformin is inappropriate, or in combination with other glucose-lowering medications.
Whilst weight loss is a common effect of Ozempic treatment, it is important to note that in the UK, the medication is licensed primarily for diabetes management. A related formulation (Wegovy, also semaglutide) is specifically licensed for weight management. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which typically diminish over time as the body adjusts to treatment.
Important safety information: Ozempic is not for use in type 1 diabetes or diabetic ketoacidosis. It carries risks of acute pancreatitis, gallbladder disease, and potential diabetic retinopathy complications with rapid improvement in blood glucose. It should be avoided in pregnancy and breastfeeding.
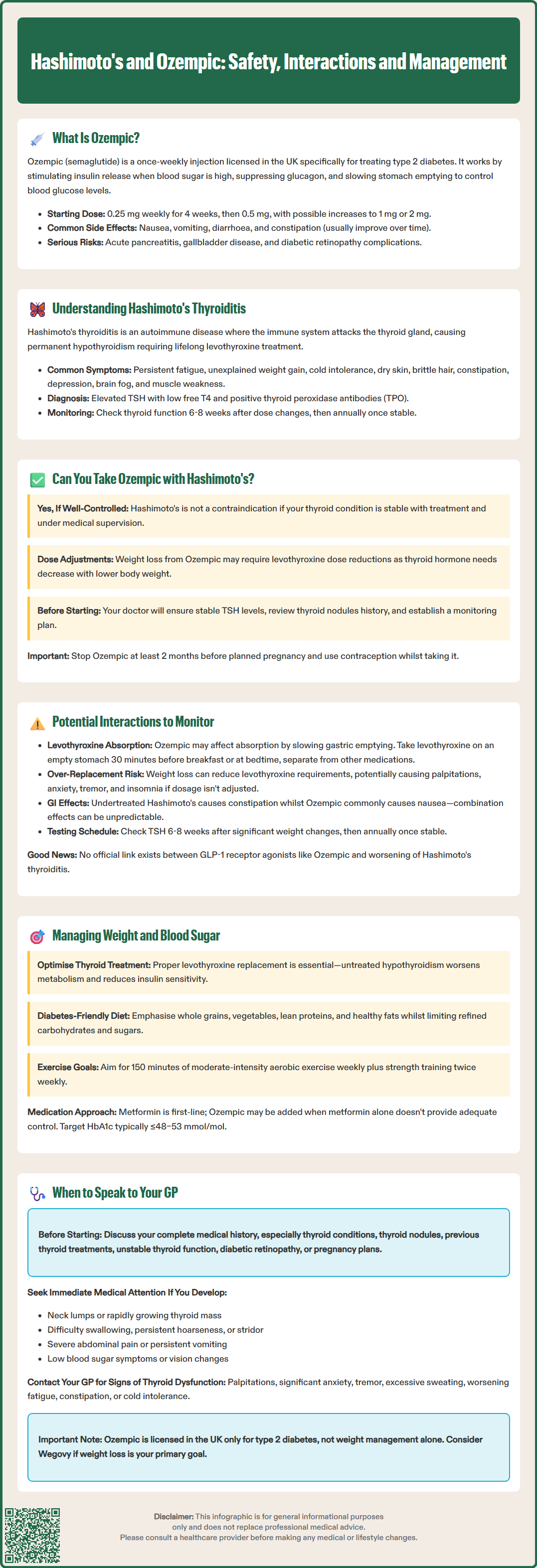
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, is the most common cause of hypothyroidism (underactive thyroid) in the UK and other iodine-sufficient regions. This autoimmune condition occurs when the body's immune system mistakenly attacks the thyroid gland, gradually destroying thyroid tissue and impairing its ability to produce essential thyroid hormones—primarily thyroxine (T4) and triiodothyronine (T3).
The condition typically develops slowly over months or years. In the early stages, some individuals may experience temporary hyperthyroidism (overactive thyroid) as damaged thyroid cells release stored hormones, a phase called "hashitoxicosis". However, as thyroid destruction progresses, most patients develop permanent hypothyroidism requiring lifelong thyroid hormone replacement therapy, usually with levothyroxine.
Common symptoms of Hashimoto's thyroiditis include:
Persistent fatigue and lethargy
Unexplained weight gain or difficulty losing weight
Cold intolerance
Dry skin and brittle hair
Constipation
Depression and cognitive difficulties ("brain fog")
Muscle weakness and joint pain
Heavy or irregular menstrual periods
Diagnosis involves blood tests measuring thyroid-stimulating hormone (TSH) and free T4; raised TSH with low free T4 confirms hypothyroidism. Positive thyroid peroxidase antibodies (TPO) support an autoimmune cause, while thyroglobulin antibodies may also be present but are less specific. According to NICE guidance (NG145), thyroid function should be monitored 6-8 weeks after any dose changes and annually when stable. The presence of a goitre (enlarged thyroid gland) may also be detected on physical examination, though this is not universal.
Certain symptoms warrant urgent medical attention, including a rapidly growing thyroid mass, persistent hoarseness, stridor, or difficulty swallowing, as these may require referral via the urgent suspected cancer pathway.
Having Hashimoto's thyroiditis is not an absolute contraindication to taking Ozempic, provided your thyroid condition is well-managed with appropriate treatment. Many individuals with both type 2 diabetes and Hashimoto's disease can safely use semaglutide under proper medical supervision. However, several important considerations must be addressed before initiating treatment.
According to the UK Summary of Product Characteristics (SmPC) for Ozempic, the only formal contraindication is hypersensitivity to semaglutide or any of the excipients. However, the SmPC does include a warning regarding thyroid C-cell tumours observed in rodent studies, though the relevance to humans remains uncertain and no causal relationship has been established in clinical trials. Patients should be advised to report symptoms such as a neck mass, difficulty swallowing, persistent hoarseness, or neck pain.
For patients with Hashimoto's thyroiditis specifically, there is no official link suggesting that Ozempic worsens autoimmune thyroid disease or interferes directly with thyroid function. However, weight loss induced by Ozempic may affect levothyroxine requirements. As body weight decreases, some patients may need adjustments to their thyroid hormone replacement dose, as levothyroxine dosing is partially weight-dependent.
Before prescribing Ozempic to someone with Hashimoto's disease, your GP or endocrinologist will:
Ensure your thyroid function is optimally controlled with stable TSH levels
Review your complete medical history, including any thyroid nodules
Assess whether the benefits of improved glycaemic control outweigh potential risks
Establish a monitoring plan for both diabetes and thyroid function
Discuss diabetic retinopathy screening, especially if rapid glycaemic improvement is expected
Advise on contraception, as Ozempic should be avoided in pregnancy and stopped at least 2 months before planned conception
Understanding the potential interactions between Ozempic and thyroid conditions requires consideration of both direct pharmacological effects and indirect metabolic consequences. Whilst there is no official link between GLP-1 receptor agonists and worsening of Hashimoto's thyroiditis or autoimmune thyroid disease, several clinically relevant interactions warrant attention.
Thyroid hormone absorption may be affected by Ozempic's mechanism of slowing gastric emptying. Levothyroxine is typically absorbed in the small intestine, and delayed gastric emptying could theoretically alter absorption patterns. However, clinical evidence for significant interaction is limited. The BNF and NHS recommend taking levothyroxine on an empty stomach, ideally 30 minutes before breakfast or at bedtime, and separate from other medicines to optimise absorption.
Weight loss induced by semaglutide represents the most clinically significant consideration for patients with Hashimoto's disease. As body weight decreases, levothyroxine requirements may change. Levothyroxine dosing is individualised, with lower starting doses often used in older patients or those with cardiac conditions, and maintenance doses guided by TSH levels. Significant weight reduction could lead to relative over-replacement. Symptoms of excessive thyroid hormone include palpitations, anxiety, tremor, and insomnia.
Additionally, both hypothyroidism and GLP-1 receptor agonists can affect gastrointestinal motility. Patients with undertreated Hashimoto's often experience constipation, whilst Ozempic commonly causes nausea and altered bowel habits. The combination may produce unpredictable gastrointestinal effects requiring careful symptom monitoring.
Thyroid function monitoring becomes particularly important during Ozempic treatment. NICE guidance (NG145) recommends checking TSH levels approximately 6–8 weeks after any significant weight change or dose adjustment of levothyroxine, then annually once stable. More frequent testing may be appropriate if symptoms develop or during pregnancy or intercurrent illness.
Managing weight and glycaemic control in patients with both Hashimoto's thyroiditis and type 2 diabetes presents unique challenges, as hypothyroidism itself contributes to weight gain, insulin resistance, and metabolic dysfunction. A comprehensive, multifaceted approach is essential for optimal outcomes.
Optimising thyroid hormone replacement forms the foundation of effective management. Inadequately treated hypothyroidism significantly impairs metabolism, making weight loss extremely difficult and worsening insulin sensitivity. Regular monitoring of thyroid function tests ensures levothyroxine dosing maintains TSH within the reference range (typically 0.4–4.0 mU/L), with targets individualised according to clinical response.
Dietary modifications for type 2 diabetes management include:
Emphasising whole grains, vegetables, lean proteins, and healthy fats
Limiting refined carbohydrates and added sugars
Maintaining consistent meal timing to support stable blood glucose
Avoiding routine iodine supplementation unless deficiency is confirmed
Considering referral to a registered dietitian for personalised advice
Physical activity plays a crucial role despite the fatigue often associated with Hashimoto's disease. The UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, alongside strength exercises on two or more days weekly. Starting gradually and building tolerance is important, particularly if thyroid function has been suboptimal.
Pharmacological interventions beyond levothyroxine may be necessary. Metformin remains the first-line medication for type 2 diabetes according to NICE NG28. When metformin alone proves insufficient, medications like Ozempic may be considered, offering both glycaemic control and weight management benefits.
Regular monitoring of HbA1c (individualised targets, typically ≤48–53 mmol/mol depending on therapy and hypoglycaemia risk), body weight, and thyroid function allows timely treatment adjustments and helps identify when additional interventions are needed.
Knowing when to seek medical advice is crucial for safe and effective management of both conditions. Several situations warrant prompt consultation with your GP or specialist endocrinologist.
Before starting Ozempic, you should discuss your complete medical history with your healthcare provider, particularly if you have:
Hashimoto's thyroiditis or any thyroid condition
Thyroid nodules or concerning neck symptoms
Previous thyroid surgery or radioactive iodine treatment
Difficulty achieving stable thyroid function despite levothyroxine treatment
Pre-existing diabetic retinopathy
Plans for pregnancy (semaglutide should be stopped at least 2 months before planned conception)
During Ozempic treatment, contact your GP if you experience:
Symptoms suggesting thyroid dysfunction: palpitations, significant anxiety, tremor, excessive sweating, or worsening fatigue, constipation, and cold intolerance
Neck symptoms: a lump in the neck, difficulty swallowing, persistent hoarseness, or neck pain (which may require urgent cancer referral per NICE NG12)
Severe gastrointestinal effects: persistent vomiting preventing adequate nutrition or medication absorption, severe abdominal pain, or signs of pancreatitis
Hypoglycaemia symptoms: particularly if taking Ozempic alongside insulin or sulphonylureas
Significant, rapid weight loss: requiring potential adjustment of levothyroxine dose
Visual changes or deterioration: which could indicate diabetic retinopathy complications
Routine monitoring should include thyroid function tests 6–8 weeks after significant weight changes or levothyroxine dose adjustments, then annually when stable (per NICE NG145). Your GP will also monitor HbA1c, renal function, and overall diabetes control according to NICE quality standards.
If you are considering Ozempic primarily for weight management rather than diabetes control, discuss this openly with your GP. Whilst off-label prescribing occurs, the licensed indication in the UK is for type 2 diabetes, and alternative approaches or the specifically licensed weight management formulation (Wegovy) may be more appropriate.
If you experience any suspected side effects from Ozempic, report them via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Yes, Hashimoto's thyroiditis is not a contraindication to Ozempic. Many patients with well-controlled thyroid disease can safely use semaglutide under medical supervision, though thyroid function monitoring may need to be more frequent, particularly if significant weight loss occurs.
Ozempic slows gastric emptying, which could theoretically affect levothyroxine absorption. To optimise absorption, take levothyroxine on an empty stomach, ideally 30 minutes before breakfast or at bedtime, and separate from other medicines.
Possibly. As body weight decreases with Ozempic treatment, levothyroxine requirements may change, as dosing is partially weight-dependent. Your GP should check thyroid function tests 6–8 weeks after significant weight loss to determine if dose adjustment is needed.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.