Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become widely prescribed for obesity management in the UK. Whilst these medications offer significant metabolic benefits, concerns have emerged regarding their potential association with pancreatitis—a serious inflammatory condition of the pancreas. Regulatory bodies including the MHRA and EMA have evaluated clinical trial data and post-marketing surveillance, listing pancreatitis as an uncommon adverse effect. However, establishing a definitive causal relationship remains complex, particularly as obesity itself increases pancreatitis risk. This article examines the evidence linking GLP-1 medications to pancreatic inflammation, identifies at-risk populations, and provides guidance on symptom recognition and safety monitoring.
Quick Answer: Weight loss injections containing GLP-1 receptor agonists list pancreatitis as an uncommon adverse effect, though a definitive causal relationship has not been established by UK regulatory authorities.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists, have become increasingly prescribed for obesity management in the UK. Medications licensed specifically for weight management include semaglutide (Wegovy) and liraglutide (Saxenda). These agents work by mimicking natural hormones that regulate appetite and blood glucose levels. They slow gastric emptying, enhance insulin secretion, and reduce glucagon release, leading to decreased food intake and subsequent weight reduction.
Pancreatitis—inflammation of the pancreas—is a serious medical condition that can manifest as acute (sudden onset) or chronic (persistent) disease. The pancreas plays vital roles in digestion and glucose regulation, producing enzymes and hormones including insulin. When inflamed, these enzymes can damage pancreatic tissue, potentially leading to severe complications including pancreatic necrosis, pseudocyst formation, or systemic inflammatory response.
The question of whether weight loss injections can cause pancreatitis has been subject to ongoing pharmacovigilance and clinical investigation. Regulatory bodies including the Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have evaluated post-marketing surveillance data and clinical trial evidence. Whilst pancreatitis is listed as a potential adverse effect in the product information for GLP-1 receptor agonists, establishing a definitive causal relationship remains complex.
It is important to recognise that obesity is associated with increased risk of pancreatitis, often mediated through mechanisms such as gallstone formation and hypertriglyceridaemia. Patients considering or currently using weight loss injections should be aware of this potential association whilst understanding that the absolute risk remains relatively low. Healthcare professionals must balance the metabolic benefits of these medications against potential pancreatic risks, particularly in susceptible individuals.
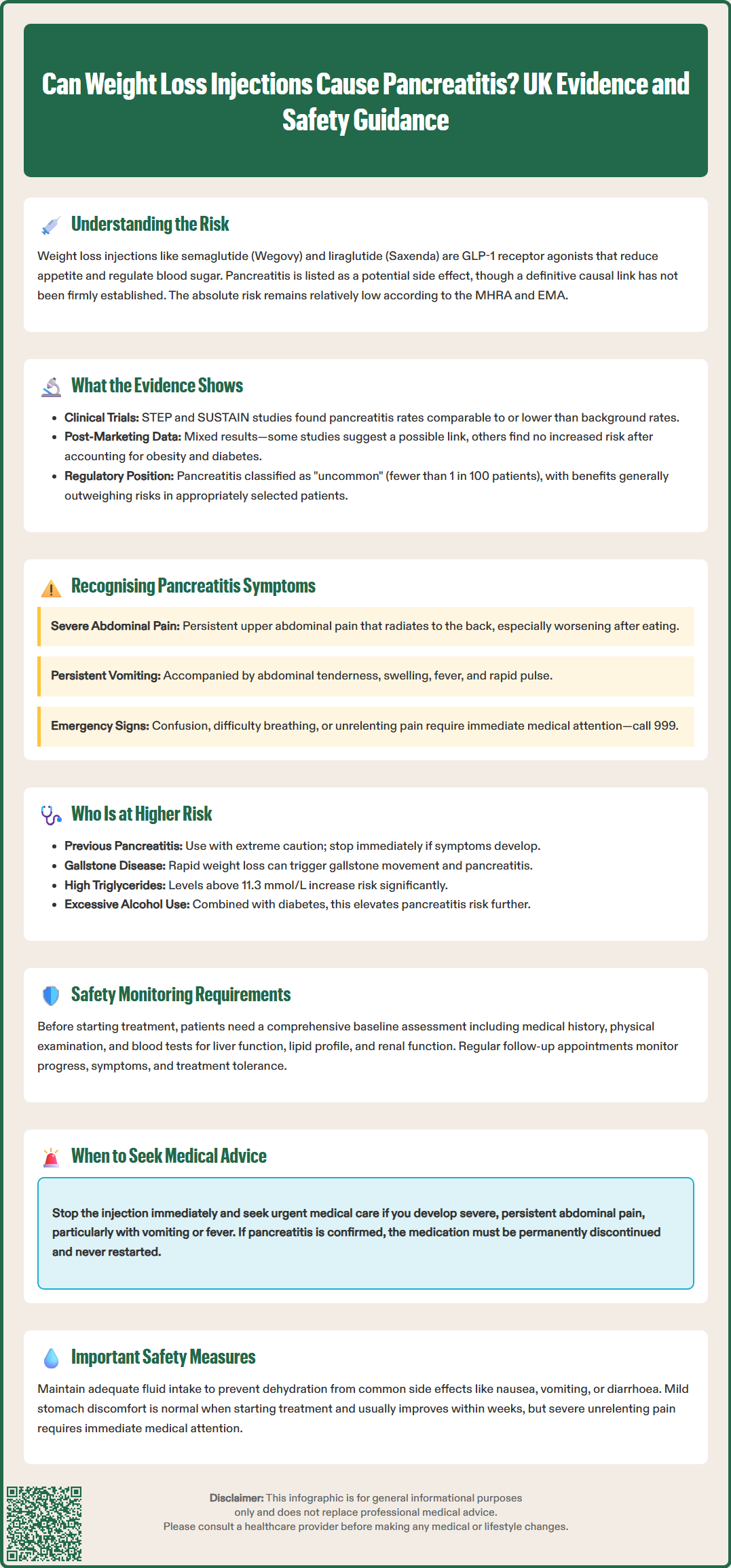
Clinical trial data and real-world evidence have provided mixed findings regarding the association between GLP-1 receptor agonists and pancreatitis. In the STEP clinical trial programme for semaglutide 2.4mg (Wegovy), pancreatitis was reported as an uncommon adverse event. Similarly, the SUSTAIN programme, which evaluated semaglutide for diabetes, found that pancreatitis events were comparable to or lower than expected background rates in the studied populations.
Post-marketing surveillance studies have yielded variable results. Some observational studies have suggested a possible association between GLP-1 receptor agonists and pancreatitis, while others have found no significant elevation in risk when appropriately adjusting for confounding factors such as obesity, diabetes duration, and concurrent medications.
The European Medicines Agency (EMA) and MHRA have conducted reviews of incretin-based therapies, including GLP-1 receptor agonists, and their potential association with pancreatic adverse events. These regulatory reviews have not established a definitive causal link but continue to recommend vigilance and appropriate patient selection.
According to the Summary of Product Characteristics (SmPC) for both Wegovy and Saxenda, pancreatitis is classified as an 'uncommon' adverse reaction (occurring in fewer than 1 in 100 but more than 1 in 1,000 patients). The SmPCs advise caution in patients with a history of pancreatitis.
Mechanistically, several theories have been proposed regarding how GLP-1 agonists might influence pancreatic function, including effects on pancreatic duct cells, alterations in enzyme secretion, or exacerbation of underlying gallstone disease (itself potentially promoted by rapid weight loss). However, there is no official consensus that these medications directly cause pancreatic inflammation. The MHRA continues to monitor safety data whilst acknowledging that the benefits of these medications generally outweigh potential risks in appropriately selected patients.
Patients using weight loss injections should be educated about the characteristic symptoms of acute pancreatitis to enable prompt recognition and medical assessment. The hallmark symptom is severe, persistent abdominal pain, typically located in the upper abdomen (epigastric region) and often radiating to the back. This pain characteristically develops suddenly, is constant rather than intermittent, and may worsen after eating.
Accompanying symptoms frequently include:
Nausea and vomiting that may be severe and persistent
Abdominal tenderness and distension
Fever and general malaise
Rapid pulse (tachycardia)
In severe cases, signs of systemic illness including confusion or breathlessness
It is crucial to distinguish pancreatitis symptoms from common gastrointestinal side effects of GLP-1 medications. Mild nausea, occasional vomiting, and transient abdominal discomfort are frequently reported during treatment initiation and typically improve over several weeks. These symptoms are generally manageable and do not indicate pancreatitis. However, severe, unrelenting abdominal pain that differs significantly from previous side effects warrants immediate medical evaluation.
Patients should be advised to stop their weight loss injection immediately and seek urgent medical attention if they develop symptoms suggestive of pancreatitis. For severe symptoms, especially if accompanied by collapse or severe breathlessness, calling 999 is appropriate. Otherwise, attending an Emergency Department or contacting NHS 111 for urgent assessment is advised. Delayed diagnosis can lead to serious complications including pancreatic necrosis, infection, or multi-organ failure.
According to the SmPCs for both Wegovy and Saxenda, if pancreatitis is confirmed, the medication should not be restarted. Healthcare professionals should maintain a low threshold for investigating suspected pancreatitis in patients receiving GLP-1 therapy.
Certain patient populations may face elevated risk of developing pancreatitis whilst using weight loss injections, necessitating careful risk-benefit assessment before treatment initiation. Previous history of pancreatitis represents a significant risk factor. According to the SmPCs for both Wegovy and Saxenda, GLP-1 receptor agonists should be used with caution in patients with a history of pancreatitis. If pancreatitis is suspected during treatment, the medication should be discontinued; if pancreatitis is confirmed, treatment should not be restarted.
Other important risk factors include:
Gallstone disease (cholelithiasis): Rapid weight loss can increase gallstone formation and migration, potentially causing gallstone pancreatitis. Patients with known gallstones require careful monitoring and should be advised about biliary symptoms.
Hypertriglyceridaemia: Severely elevated triglyceride levels (typically >11.3 mmol/L) can precipitate pancreatitis. Clinicians may consider lipid assessment in patients with risk factors for dyslipidaemia.
Excessive alcohol consumption: Alcohol is a leading cause of pancreatitis and may interact synergistically with medication-related risk.
Type 2 diabetes: Diabetes itself confers increased pancreatitis risk, though GLP-1 agents are commonly used in this population with appropriate monitoring.
Age, gender, and genetic factors may also influence susceptibility, though evidence remains limited. NICE guidance on obesity management (TA875 for semaglutide and TA664 for liraglutide) recommends thorough patient assessment before prescribing weight loss medications, including evaluation of risk factors.
Healthcare professionals should document baseline risk assessment and ensure patients understand warning symptoms. In higher-risk individuals, alternative weight management strategies—including lifestyle modification, psychological support, or bariatric surgery referral—may be more appropriate. Shared decision-making should incorporate individual risk profiles, treatment goals, and patient preferences to optimise safety whilst addressing obesity-related health complications.
Appropriate safety monitoring during weight loss injection therapy is essential for early detection of potential pancreatic complications. Before treatment initiation, healthcare professionals should conduct comprehensive baseline assessment including medical history (particularly previous pancreatitis, gallstones, or alcohol use), physical examination, and relevant investigations. Baseline blood tests may include liver function, lipid profile, and renal function, though routine pancreatic enzyme measurement is not typically recommended in asymptomatic patients.
During treatment, patients should attend follow-up appointments according to the product SmPC and local specialist weight management service protocols. For Saxenda (liraglutide), NICE TA664 specifies a 12-week stopping rule at the maintenance dose if 5% weight loss has not been achieved. For Wegovy (semaglutide), follow-up should align with the dose escalation schedule and specialist service protocols as outlined in NICE TA875. These consultations provide opportunities to:
Review symptom development, particularly gastrointestinal effects
Monitor weight loss progress and metabolic parameters
Assess treatment tolerance and adherence
Reinforce safety advice regarding pancreatitis symptoms
Patients must be clearly instructed to seek immediate medical attention if they develop severe, persistent abdominal pain, particularly if accompanied by vomiting or fever. They should attend their local Emergency Department or contact NHS 111 for urgent assessment. The weight loss injection should be discontinued pending medical evaluation.
Patients should be advised about the risk of dehydration from gastrointestinal side effects, which could potentially lead to acute kidney injury in susceptible individuals. Adequate fluid intake should be encouraged, particularly if experiencing nausea, vomiting or diarrhoea.
Diagnosis of suspected pancreatitis typically involves blood tests measuring serum amylase and lipase (pancreatic enzymes that become elevated during inflammation) and imaging studies. Abdominal ultrasound is usually the first-line investigation to assess for gallstones, while CT scanning may be used when diagnosis is uncertain or to assess severity. If pancreatitis is confirmed, the GLP-1 medication must be permanently discontinued, and alternative weight management strategies should be considered once recovery is complete.
For routine concerns or mild side effects, patients should contact their prescribing clinician or GP practice. Suspected adverse reactions should be reported through the Yellow Card Scheme (yellowcard.mhra.gov.uk) operated by the MHRA. Healthcare professionals should maintain vigilance for pancreatitis throughout treatment duration whilst recognising that, for most patients, weight loss injections provide significant metabolic benefits with acceptable safety profiles when used appropriately.
Pancreatitis is classified as an uncommon adverse reaction to GLP-1 weight loss injections, occurring in fewer than 1 in 100 but more than 1 in 1,000 patients according to UK product information. The absolute risk remains relatively low, though patients with previous pancreatitis or gallstones face elevated risk.
The hallmark symptom is severe, persistent upper abdominal pain that radiates to the back, often accompanied by nausea, vomiting, fever, and abdominal tenderness. This differs from common mild gastrointestinal side effects and requires immediate medical assessment and medication discontinuation.
GLP-1 receptor agonists should be used with caution in patients with previous pancreatitis according to UK product information. If pancreatitis is confirmed during treatment, the medication must be permanently discontinued and alternative weight management strategies should be considered after thorough risk-benefit discussion with your healthcare professional.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.