
Can you drink alcohol on weight loss injections? This is a common question for patients prescribed GLP-1 receptor agonists such as semaglutide (Wegovy) or liraglutide (Saxenda) for obesity management in the UK. Whilst moderate alcohol consumption is not explicitly contraindicated, several important safety and efficacy considerations must be understood. Alcohol is calorically dense and can undermine weight loss efforts, whilst the delayed gastric emptying caused by these medications may alter how alcohol is absorbed. Individual factors including medical history, concurrent medications, and treatment goals should guide personalised advice. Always discuss alcohol consumption with your prescribing clinician or GP before starting treatment.
Quick Answer: Moderate alcohol consumption is not explicitly contraindicated with weight loss injections, but it can undermine treatment effectiveness and may exacerbate side effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for obesity management in the UK. A common question amongst patients is whether alcohol consumption is safe whilst using these medications. The short answer is that moderate alcohol consumption is not explicitly contraindicated with weight loss injections, but several important considerations must be understood.
These medications work by mimicking the glucagon-like peptide-1 hormone, which regulates appetite, slows gastric emptying, reduces glucagon secretion, and increases glucose-dependent insulin secretion. The UK Summary of Product Characteristics (SmPC) for both Wegovy and Saxenda do not list alcohol as a contraindication or interaction. However, the relationship between alcohol and weight loss injections can affect both treatment efficacy and patient safety.
Alcohol itself is calorically dense, providing approximately 7 kilocalories per gram—nearly as much as fat. This can significantly undermine weight loss efforts. Additionally, the delayed gastric emptying caused by GLP-1 agonists may delay alcohol absorption; there is no established effect on alcohol metabolism. Patients should be aware that alcohol can also mask or exacerbate certain side effects of these medications, particularly gastrointestinal symptoms such as nausea and vomiting.
It is essential to discuss alcohol consumption with your prescribing clinician or GP before starting treatment. Individual factors such as medical history, concurrent medications, and treatment goals will influence personalised advice. The decision to consume alcohol should be made with full awareness of potential risks and impact on weight management outcomes.
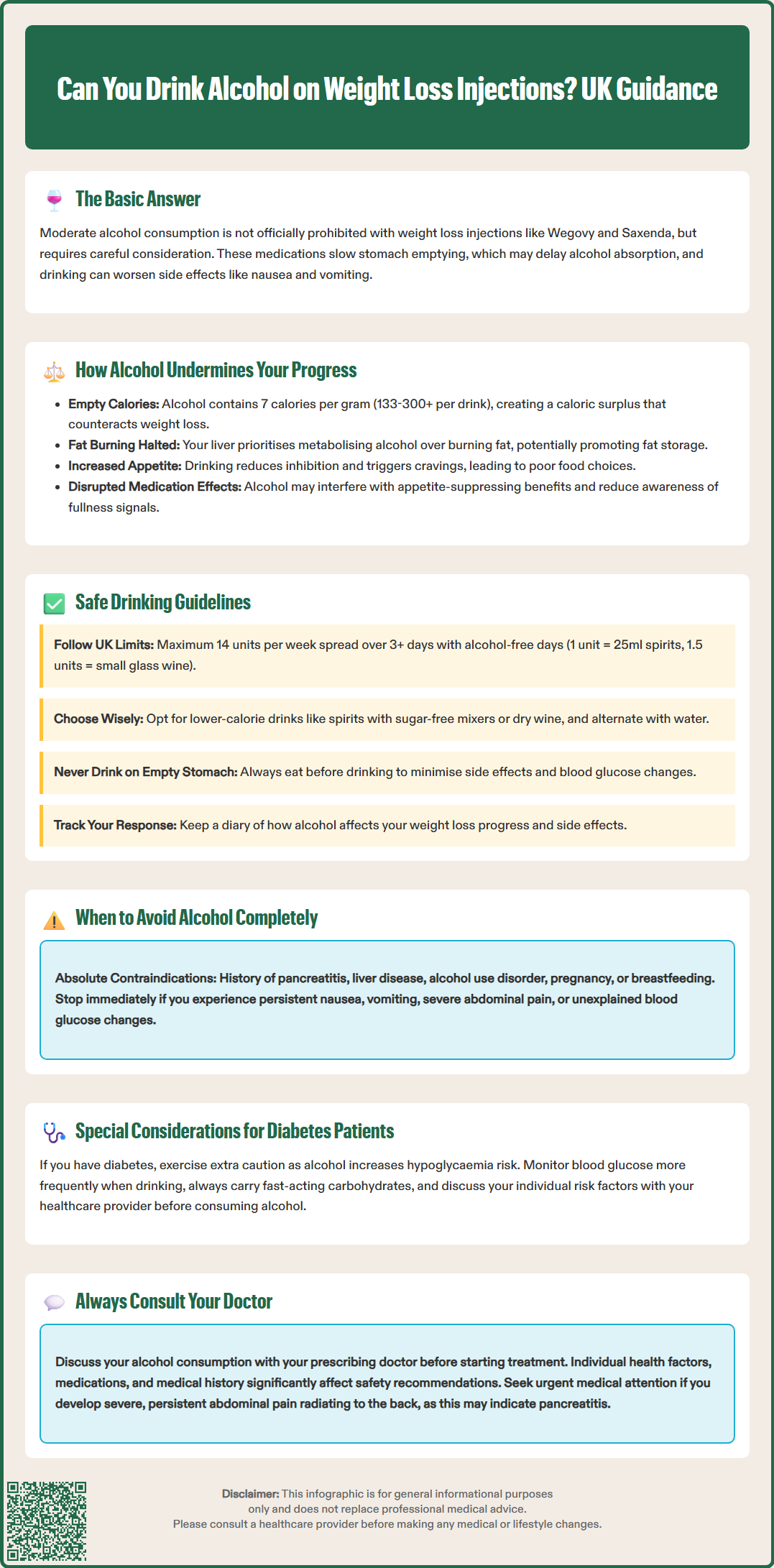
Understanding how alcohol interferes with weight loss injection effectiveness requires consideration of both pharmacological and behavioural factors. Caloric contribution represents the most direct impact—alcoholic beverages add substantial energy intake without nutritional benefit. According to NHS guidance, a standard glass (175ml) of wine contains approximately 133 kilocalories, whilst cocktails and spirits mixed with sugary beverages can exceed 200-300 kilocalories per serving. For patients working towards a caloric deficit necessary for weight loss, regular alcohol consumption can significantly impede progress.
Alcohol also affects metabolic processes that are central to weight management. The liver prioritises metabolising alcohol over other nutrients, temporarily halting fat oxidation and potentially promoting fat storage. This metabolic shift can transiently affect glycaemia, though evidence that it specifically counteracts GLP-1 receptor agonist pharmacology is limited. Furthermore, alcohol consumption often leads to poor dietary choices—the phenomenon of reduced inhibition and increased appetite for high-calorie, nutrient-poor foods is well-documented.
Alcohol may influence the appetite-suppressing effects of weight loss injections. Whilst GLP-1 agonists work to reduce hunger signals and increase satiety, alcohol can potentially disrupt these pathways. Some patients report that alcohol consumption triggers cravings or reduces their awareness of fullness cues, leading to overeating, though individual responses vary.
Additionally, alcohol can affect medication adherence and lifestyle modifications. Patients who consume alcohol regularly may be less likely to maintain the dietary changes, physical activity, and behavioural modifications that are essential components of comprehensive weight management programmes recommended by NICE guidance. The combination of pharmacotherapy with lifestyle intervention produces superior outcomes compared to medication alone, and alcohol can undermine this synergistic approach.
For patients who choose to consume alcohol whilst using weight loss injections, adhering to UK Chief Medical Officers' low-risk drinking guidelines is essential. These recommend not regularly drinking more than 14 units of alcohol per week, spread over three or more days, with several alcohol-free days each week. One unit equals 10ml or 8g of pure alcohol—approximately a single measure (25ml) of 40% spirits (1 unit), a small glass (125ml) of 12% wine (1.5 units), or half a pint (284ml) of 4% beer (1.1 units).
Patients may consider reducing their intake below these guidelines when using weight loss medications, particularly during the initial titration phase when side effects such as nausea, vomiting, and gastrointestinal discomfort are most common. Starting with smaller quantities and monitoring individual tolerance is advisable. The delayed gastric emptying caused by GLP-1 agonists may mean alcohol absorption is slower, potentially affecting how quickly you feel its effects.
Practical strategies for safer alcohol consumption include:
Choosing lower-calorie options such as spirits with sugar-free mixers or dry wine rather than sweet cocktails or creamy liqueurs
Alternating alcoholic drinks with water to maintain hydration and reduce overall consumption
Avoiding drinking on an empty stomach, as this may exacerbate gastrointestinal side effects
Minimising alcohol consumption during dose escalation or when experiencing GI symptoms
Keeping a diary to monitor how alcohol affects weight loss progress and medication side effects
Patients with diabetes using these medications require particular caution, as alcohol can increase the risk of hypoglycaemia, especially when combined with insulin or sulfonylureas. Blood glucose monitoring should be more frequent when consuming alcohol, and patients should carry fast-acting carbohydrates and avoid driving if at risk of hypoglycaemia. If you experience increased side effects, reduced weight loss, or any concerning symptoms, discuss reducing or eliminating alcohol with your healthcare provider.
Certain circumstances necessitate complete alcohol abstinence whilst using weight loss injections. Patients with a history of pancreatitis should avoid alcohol entirely, as both GLP-1 receptor agonists and alcohol independently carry a risk of precipitating acute pancreatitis. The combination may compound this risk, though definitive evidence remains limited. If pancreatitis is suspected (severe, persistent abdominal pain, possibly radiating to the back, with or without vomiting), stop the medication immediately and seek urgent medical attention.
Individuals with liver disease should generally avoid alcohol on clinical grounds. While GLP-1 receptor agonists are not hepatically metabolised (they are broken down by general proteolysis in the body) and usually do not require dose adjustment in hepatic impairment, alcohol could worsen underlying liver conditions. Your healthcare provider may recommend liver function monitoring if you have pre-existing liver disease.
Alcohol use disorder or problematic drinking patterns represent absolute contraindications to alcohol consumption during treatment. Weight loss injections require commitment to comprehensive lifestyle modification, and active alcohol misuse undermines treatment efficacy and patient safety. If you struggle with alcohol consumption, discuss this openly with your healthcare provider—support services and specialist referral may be appropriate.
Patients should temporarily abstain from alcohol if experiencing:
Persistent or severe nausea and vomiting
Dehydration or difficulty maintaining adequate fluid intake
Dizziness (which may be related to dehydration from GI symptoms)
Any signs of pancreatitis (severe abdominal pain, fever, rapid pulse)
Unexplained changes in blood glucose levels (for diabetic patients)
Pregnancy and breastfeeding represent additional situations requiring complete alcohol avoidance. Weight loss injections are contraindicated during these periods. Women of childbearing potential should use effective contraception during treatment. Semaglutide should be discontinued at least 2 months before a planned pregnancy, while liraglutide should be stopped if pregnancy is planned or occurs.
If you are taking multiple medications, particularly those affecting the central nervous system, metabolism, or blood glucose, consult your GP or pharmacist about potential interactions with alcohol. The cumulative effect of alcohol with various medications may necessitate complete abstinence. Always prioritise open communication with your healthcare team to ensure safe, effective treatment tailored to your individual circumstances.
If you experience any suspected side effects from your medication, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Moderate alcohol consumption is not contraindicated, but it can reduce treatment effectiveness and worsen side effects such as nausea. Always follow UK low-risk drinking guidelines (maximum 14 units weekly) and discuss your individual circumstances with your prescribing clinician.
Alcohol provides substantial calories (approximately 7 kilocalories per gram) without nutritional benefit, which can significantly impede weight loss progress. It may also disrupt appetite regulation, promote poor dietary choices, and temporarily halt fat oxidation as the liver prioritises metabolising alcohol.
Complete alcohol abstinence is necessary if you have a history of pancreatitis, liver disease, or alcohol use disorder. You should also temporarily avoid alcohol if experiencing severe nausea, vomiting, dehydration, or any signs of pancreatitis such as severe abdominal pain.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.