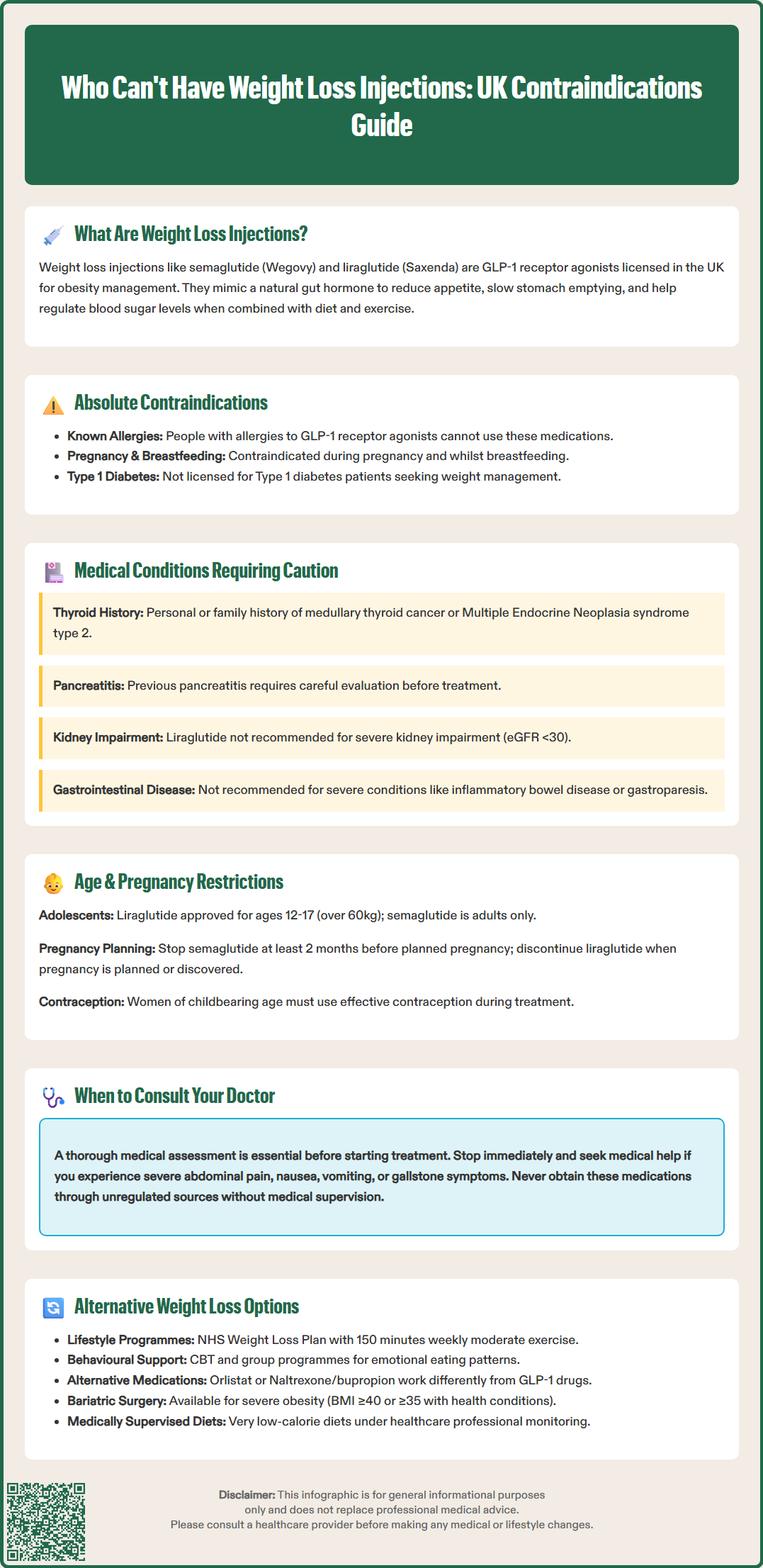
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have become important tools in obesity management across the UK. However, these GLP-1 receptor agonist medications are not suitable for everyone. Certain medical conditions, life stages, and individual circumstances mean some people cannot safely use these treatments. Understanding who can't have weight loss injections is essential for patient safety and informed decision-making. This article examines the contraindications, cautions, and restrictions surrounding these medications, alongside alternative weight management options for those unable to use injectable treatments.
Quick Answer: Weight loss injections are contraindicated in people with known hypersensitivity to GLP-1 receptor agonists, during pregnancy and breastfeeding, and require caution in those with certain thyroid, pancreatic, or severe gastrointestinal conditions.
Weight loss injections have emerged as a significant treatment option for obesity management in the UK, with medications such as semaglutide (Wegovy) and liraglutide (Saxenda) now licensed by the MHRA for weight management. These injectable medications belong to a class of drugs called GLP-1 receptor agonists (glucagon-like peptide-1), which were originally developed for type 2 diabetes management but have demonstrated substantial weight loss effects.
The mechanism of action centres on mimicking a naturally occurring hormone called GLP-1, which is released by the intestines after eating. These medications work through several pathways:
Appetite suppression: They act on receptors in the brain's appetite centres, reducing hunger signals and increasing feelings of fullness (satiety)
Delayed gastric emptying: Food moves more slowly from the stomach into the intestines, prolonging the sensation of fullness after meals
Blood glucose regulation: They enhance insulin secretion when blood sugar levels are elevated and reduce glucagon release, helping to stabilise blood glucose
Clinical trials have shown that when combined with lifestyle modifications including dietary changes and increased physical activity, these injections can lead to significant weight reduction. While the MHRA has licensed these medications for individuals with a BMI of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities, NHS access via NICE guidance is more restrictive. For example, semaglutide (Wegovy) is typically only available through specialist weight management services, with stricter BMI criteria and time-limited use (usually up to 2 years).
These medications are administered via subcutaneous injection, usually once weekly (semaglutide) or once daily (liraglutide), using pre-filled pen devices. Treatment requires ongoing medical supervision and regular monitoring. While the medications are licensed for longer-term use, NHS provision is typically time-limited according to NICE guidance and local commissioning arrangements.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections are not appropriate for everyone seeking to lose weight, and healthcare professionals must carefully assess suitability before prescribing. According to UK SmPCs (Summary of Product Characteristics), there are specific contraindications and situations where caution is required.
Absolute contraindications include:
Known hypersensitivity or previous severe allergic reaction to GLP-1 receptor agonists or any component of the medication
Pregnancy and breastfeeding (these medications should not be used during these periods)
Conditions requiring caution or where use is not recommended:
Personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) – while not formal contraindications in UK SmPCs, caution is advised due to findings of C-cell tumours in rodent studies
Type 1 diabetes – these medications are not licensed for weight management in this condition
Severe gastrointestinal disease – including inflammatory bowel disease or gastroparesis (delayed stomach emptying), where use is generally not recommended rather than absolutely contraindicated
Additionally, weight loss injections are not recommended for people seeking modest weight loss for cosmetic purposes alone. In the NHS, access is typically restricted to specialist weight management services and follows NICE guidance criteria, which are more stringent than the licensed indication.
It is essential that prescribers conduct a thorough medical history and assessment before initiating treatment. Patients should disclose all existing medical conditions, current medications, and any previous adverse reactions to similar drugs. Self-administration without medical supervision or obtaining these medications through unregulated sources poses significant health risks and should be avoided. If you are considering weight loss injections, consult your GP who can assess your eligibility and refer you to appropriate services if suitable.
Several medical conditions require careful consideration before prescribing weight loss injections. Understanding these restrictions is crucial for patient safety and optimal treatment outcomes.
Thyroid conditions warrant attention. While not formal contraindications in UK SmPCs, caution is advised with any personal or family history of medullary thyroid carcinoma. Animal studies demonstrated thyroid C-cell tumours with GLP-1 receptor agonists, though there is no definitive evidence this occurs in humans. Patients should inform their doctor of any thyroid nodules or abnormal thyroid function.
Pancreatic disease requires careful evaluation. Individuals with a history of pancreatitis (inflammation of the pancreas) should be treated with caution, as GLP-1 receptor agonists have been associated with acute pancreatitis in some cases. UK SmPCs advise discontinuing treatment if pancreatitis is suspected and not restarting if confirmed. Symptoms such as severe abdominal pain radiating to the back, nausea, and vomiting warrant immediate medical attention.
Renal impairment considerations vary by medication. According to UK SmPCs, liraglutide is not recommended in severe renal impairment (eGFR <30 mL/min/1.73m²). For semaglutide, no dose adjustment is required in renal impairment, though caution is advised due to potential dehydration risk from gastrointestinal side effects. Kidney function should be assessed before starting treatment.
Diabetic retinopathy complications require caution, particularly in people with type 2 diabetes who are on insulin therapy. Rapid improvements in blood glucose control have been associated with temporary worsening of diabetic eye disease, necessitating appropriate ophthalmological monitoring.
Gallbladder disease risk may be increased with GLP-1 receptor agonists. Patients should be informed about symptoms of gallstones and seek medical attention if these occur.
Patients with these conditions should discuss the risks and benefits with their healthcare provider. Regular monitoring and open communication about any new symptoms are vital for those deemed suitable for treatment despite these cautions.
Age-related restrictions and reproductive health considerations are important factors determining eligibility for weight loss injections.
Age restrictions apply at both ends of the spectrum. In the UK, liraglutide (Saxenda) is licensed for adolescents aged 12-17 years with a body weight above 60kg, while semaglutide (Wegovy) is currently only licensed for adults. Use in young people should only occur within specialist weight management services with appropriate expertise and monitoring capabilities.
For older adults, whilst there is no upper age limit and no routine age-based dose adjustments are required per UK SmPCs, careful assessment is necessary. Elderly patients may have multiple comorbidities, reduced renal function, and be taking numerous medications, all of which require consideration. The risk of adverse effects, particularly gastrointestinal symptoms and dehydration, may be higher. Closer monitoring is often appropriate based on individual clinical judgement.
Pregnancy represents a contraindication to weight loss injections. According to UK SmPCs, semaglutide should be discontinued at least 2 months before a planned pregnancy due to its long half-life, while liraglutide should be stopped when pregnancy is planned or occurs. Weight loss during pregnancy is not recommended, and the safety of GLP-1 receptor agonists in pregnancy has not been established. If pregnancy occurs during treatment, the medication should be stopped immediately, and the patient should contact their healthcare provider.
Women of childbearing potential should use effective contraception during treatment. It is important to note that while weight loss itself does not reduce oral contraceptive efficacy, vomiting within a few hours of taking contraceptive pills or severe diarrhoea may affect absorption. In these circumstances, additional contraceptive precautions may be needed, as advised by the Faculty of Sexual and Reproductive Healthcare (FSRH).
Breastfeeding mothers should not use weight loss injections. It is unknown whether these medications pass into breast milk, and potential effects on the nursing infant cannot be excluded. Women wishing to breastfeed should discuss alternative weight management approaches with their healthcare provider.
For individuals who cannot have weight loss injections due to contraindications or personal preference, numerous evidence-based alternatives exist. NICE recommends a multicomponent approach to weight management that addresses diet, physical activity, and behavioural factors.
Lifestyle modification programmes form the foundation of weight management. NHS-supported programmes such as the NHS Weight Loss Plan provide structured guidance on healthy eating, portion control, and sustainable dietary changes. Referral to specialist dietitians can provide personalised nutritional advice tailored to individual medical conditions and preferences. Increasing physical activity gradually, aiming for at least 150 minutes of moderate-intensity exercise weekly, supports weight loss and improves overall health.
Behavioural interventions address the psychological aspects of eating and weight management. Cognitive behavioural therapy (CBT) can help identify and modify unhelpful eating patterns, emotional eating, and barriers to lifestyle change. Group-based programmes offer peer support and accountability, which many find beneficial.
Alternative medications may be suitable for some individuals. Orlistat is a lipase inhibitor that reduces fat absorption from the diet and is available both on prescription and over-the-counter. Naltrexone/bupropion (Mysimba) is another licensed option in the UK, though availability varies according to local commissioning arrangements. These medications work differently from GLP-1 receptor agonists and may be appropriate for those with contraindications to injections.
Bariatric surgery represents an option for individuals with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) when other interventions have been unsuccessful. NICE guidance includes lower BMI thresholds for certain ethnic groups and for people with recent-onset type 2 diabetes. Procedures such as gastric bypass or sleeve gastrectomy can achieve substantial, sustained weight loss. Assessment by specialist multidisciplinary teams is essential.
Very low-calorie diets (VLCDs) under medical supervision may be appropriate for some patients, particularly those with type 2 diabetes. These intensive programmes require careful monitoring and should only be undertaken with healthcare professional guidance.
The NHS offers tiered weight management services, from community-based support to specialist multidisciplinary teams. Contact your GP to discuss which weight management options are most suitable for your individual circumstances, medical history, and personal goals.
If you experience any suspected side effects from weight management medications, report them through the MHRA Yellow Card scheme.
No, weight loss injections are contraindicated during pregnancy and breastfeeding. Semaglutide should be stopped at least 2 months before planned pregnancy, whilst liraglutide should be discontinued when pregnancy is planned or confirmed.
Caution is required for individuals with previous pancreatitis, as GLP-1 receptor agonists have been associated with acute pancreatitis. Treatment should be discontinued if pancreatitis is suspected and not restarted if confirmed.
Alternatives include NHS lifestyle modification programmes, alternative medications such as orlistat or naltrexone/bupropion, behavioural interventions like CBT, and bariatric surgery for those with severe obesity who meet NICE criteria.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.