LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have transformed obesity management in the UK, but many patients wonder whether they can stop these treatments safely. The answer is yes—you can discontinue weight loss injections without serious physical harm, as GLP-1 receptor agonists do not cause dangerous withdrawal symptoms. However, stopping treatment often leads to weight regain as appetite-suppressing effects diminish. This article explores the safety considerations, physiological changes, and practical strategies for discontinuing weight loss injections whilst minimising weight regain. Understanding what happens when you stop and how to maintain results through sustainable lifestyle changes is essential for long-term success.
Quick Answer: You can safely stop weight loss injections such as semaglutide or liraglutide without dangerous withdrawal symptoms, though most patients experience weight regain after discontinuation.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists, have become increasingly prescribed for obesity management in the UK. The most commonly used medications include semaglutide (marketed as Wegovy for weight management) and liraglutide (Saxenda). These medications were originally developed for type 2 diabetes management but have demonstrated significant efficacy in weight reduction.
These injections work through several complementary mechanisms. GLP-1 receptor agonists mimic a naturally occurring hormone that regulates appetite and food intake. They slow gastric emptying, meaning food remains in the stomach longer, promoting feelings of fullness. Additionally, they act on appetite centres in the brain, particularly the hypothalamus, reducing hunger signals and food cravings. This dual action helps patients consume fewer calories without experiencing the intense hunger often associated with traditional calorie restriction.
According to NICE guidance, these medications are prescribed within specialist weight management services and are recommended as part of a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support. Eligibility typically requires a BMI of at least 35 kg/m² (or 30 kg/m² with weight-related comorbidities) and previous unsuccessful weight loss attempts. Clinical trials have shown that patients using semaglutide alongside lifestyle interventions can achieve average weight loss of 10-15% of their initial body weight over 68 weeks (STEP 1 trial), while liraglutide typically produces more modest weight loss of 5-8%.
It is important to understand that weight loss injections are typically intended as treatments with ongoing review rather than permanent solutions. NICE guidance recommends time-limited use (typically up to 2 years for Wegovy) with regular assessment of benefits. The medications do not permanently alter metabolism or appetite regulation, which has significant implications for anyone considering stopping treatment. Healthcare professionals emphasise that these injections work best when integrated into sustainable lifestyle changes that can be maintained after treatment cessation.
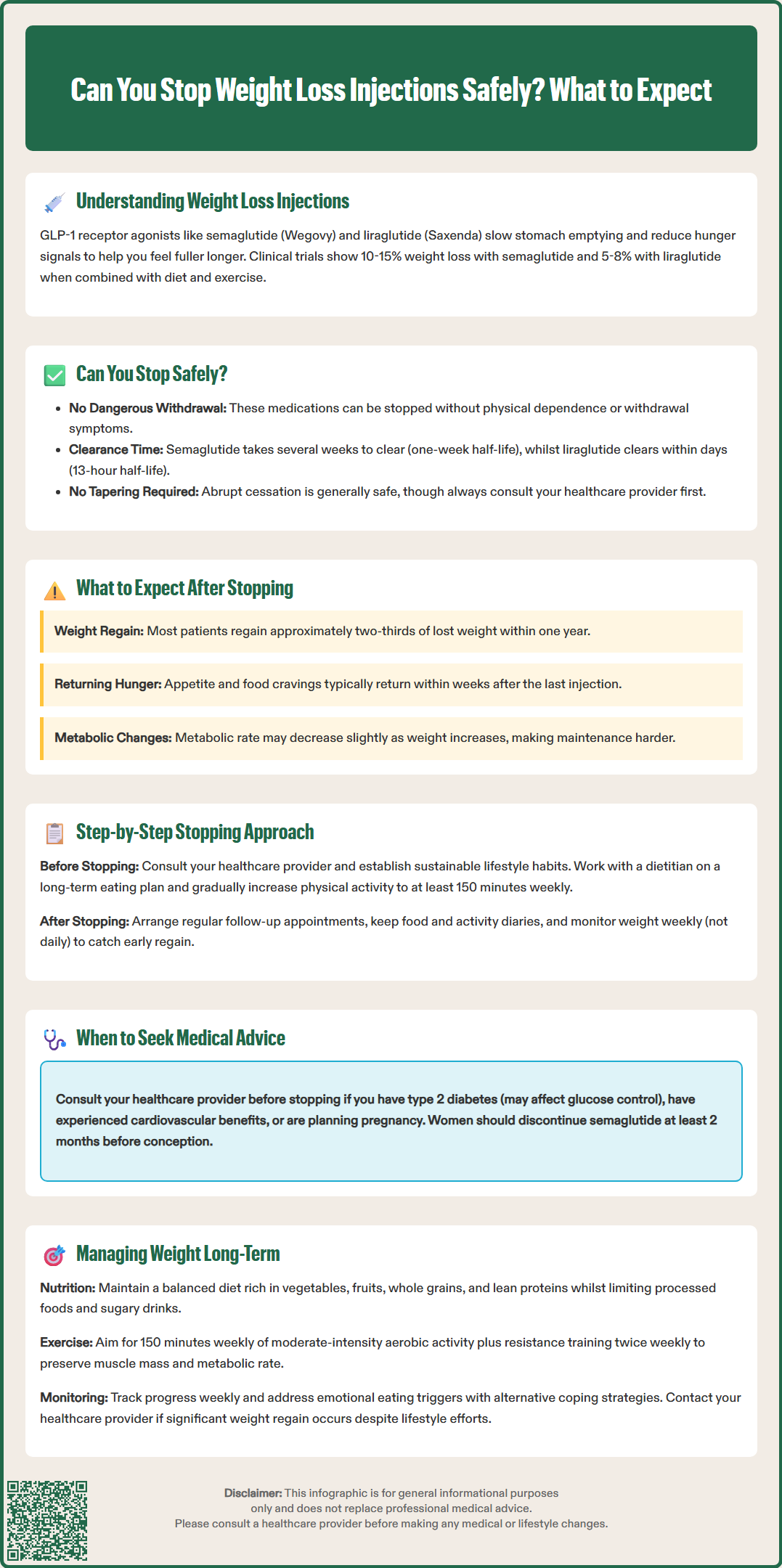
Yes, you can stop weight loss injections safely, and there is no medical requirement to continue them indefinitely. Unlike some medications that cause dangerous withdrawal symptoms when discontinued abruptly, GLP-1 receptor agonists can generally be stopped without serious physical harm. However, the decision to discontinue treatment should ideally be made in consultation with your prescribing healthcare professional rather than independently.
Safety considerations when stopping these injections are generally favourable. There is no evidence of physical dependence or withdrawal syndrome associated with GLP-1 receptor agonists. The medications gradually clear from the body—semaglutide has a half-life of approximately one week with effects diminishing over several weeks, whilst liraglutide has a half-life of around 13 hours with more rapid clearance.
Several factors should inform the decision to stop treatment. According to the Summary of Product Characteristics (SmPC), liraglutide (Saxenda) should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3mg dose. For semaglutide (Wegovy), response should be evaluated after 16 weeks at the maintenance dose. If you have achieved your target weight and maintained it for several months whilst developing sustainable lifestyle habits, discontinuation may be appropriate. Conversely, if you are experiencing intolerable side effects such as persistent nausea, vomiting, or other adverse reactions, stopping may be medically advisable. Financial considerations and medication availability also influence many patients' decisions.
Certain situations warrant immediate medical consultation before stopping. If you have type 2 diabetes and use these medications for glucose control as well as weight management, stopping without medical supervision could affect your diabetes management and require adjustment of other diabetes medications. Similarly, if you have experienced significant cardiovascular benefits from weight loss, your doctor should assess the risks of discontinuation.
For women of childbearing potential, effective contraception is recommended during treatment. According to the SmPC, semaglutide should be discontinued at least 2 months before a planned pregnancy, and neither medication is recommended during breastfeeding.
Seek urgent medical attention if you experience severe, persistent abdominal pain (with or without vomiting) which could indicate pancreatitis or gallbladder problems—known rare but serious side effects of these medications. Always inform your GP or specialist before making changes to your prescribed treatment regimen, and report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
When you stop taking weight loss injections, the most significant and common consequence is weight regain. Clinical studies consistently demonstrate that most patients experience some degree of weight increase after discontinuing GLP-1 receptor agonists. Research from the STEP 1 extension study published in JAMA (2022) showed that patients may regain approximately two-thirds of their lost weight within one year of stopping semaglutide treatment, though individual variation is considerable.
This weight regain occurs because the medication's appetite-suppressing effects gradually diminish. As the drug clears from your system, gastric emptying returns to normal speed, and the signals to appetite centres in the brain are no longer modified. Many patients report a return of hunger and food cravings within weeks of their last injection, though the timing varies considerably between individuals. Some experience a gradual increase in appetite whilst others notice more abrupt changes.
Beyond appetite changes, some patients report alterations in energy levels and mood. While there is no established causal link between stopping GLP-1 receptor agonists and depression or anxiety, the psychological impact of weight regain can affect mental wellbeing. Some individuals experience frustration, disappointment, or reduced self-esteem as they observe changes on the scales. If you experience significant mood changes or thoughts of self-harm after stopping treatment, seek medical help promptly. Regulatory authorities including the MHRA continue to monitor the safety of these medications.
Physiologically, metabolic rate may decrease slightly as body weight increases, creating a challenging cycle. Additionally, if you had experienced improvements in obesity-related conditions such as sleep apnoea, joint pain, or fatty liver disease, these benefits may diminish with weight regain. Blood pressure and cholesterol levels, which often improve during weight loss, may also return towards baseline values.
For people with diabetes, blood glucose levels may worsen after stopping treatment, requiring closer monitoring and possibly adjustment of other diabetes medications. However, any sustained lifestyle improvements—such as increased physical activity or improved dietary habits—can help mitigate these effects and preserve some health benefits even after stopping injections.
Step 1: Consult your healthcare provider. Before making any changes to your medication regimen, schedule an appointment with your GP or the specialist who prescribed your weight loss injections. Discuss your reasons for wanting to stop, whether related to side effects, cost, achievement of goals, or other factors. Your healthcare professional can assess your individual circumstances and provide personalised guidance.
Step 2: Consider the stopping approach. According to the SmPCs for these medications, no specific tapering is required when discontinuing treatment. Abrupt cessation is generally safe from a physiological perspective. Some clinicians may suggest dose reduction before stopping completely, but this would be an off-label approach not specifically supported by product licensing. Any changes to dosing should be directed by your prescribing healthcare professional.
Step 3: Strengthen lifestyle foundations before stopping. In the weeks leading up to discontinuation, focus intensively on establishing sustainable habits. Work with a dietitian to develop a realistic eating plan that you can maintain long-term. Increase your physical activity gradually, aiming for at least 150 minutes of moderate-intensity exercise weekly, as recommended by the UK Chief Medical Officers' Physical Activity Guidelines. Consider joining support groups or working with a behavioural therapist to address emotional eating patterns.
Step 4: Plan for monitoring and support. Arrange regular follow-up appointments with your healthcare team after stopping. Schedule regular weigh-ins and consider keeping a food and activity diary. Identify specific triggers for overeating and develop coping strategies in advance. Some patients benefit from continued involvement with NHS weight management services (Tier 2 or 3) or the NHS Digital Weight Management Programme that provide ongoing accountability and support. If you notice significant weight regain, contact your healthcare provider to discuss intervention options before further gain occurs.
For people with diabetes, work with your diabetes team to establish a monitoring plan for blood glucose levels after stopping treatment, as adjustments to other diabetes medications may be necessary. Remember that NICE guidance for Wegovy (semaglutide) typically recommends time-limited treatment of up to 2 years, with ongoing review of benefits, so planned stopping may be part of your treatment pathway.
Successfully maintaining weight loss after stopping injections requires a comprehensive, long-term strategy that addresses multiple aspects of weight management. The most critical factor is adherence to sustainable lifestyle modifications that were ideally established during treatment.
Dietary management forms the cornerstone of weight maintenance. Focus on a balanced diet rich in vegetables, fruits, whole grains, and lean proteins whilst limiting processed foods, sugary beverages, and excessive portions. The NHS Eatwell Guide provides an excellent framework for healthy eating patterns. Many patients find that continuing to use strategies learned during treatment—such as eating slowly, using smaller plates, and planning meals in advance—helps manage appetite without medication. Consider working with a registered dietitian who can provide personalised nutrition guidance tailored to your preferences and lifestyle.
Regular physical activity is equally essential for weight maintenance. Beyond the recommended 150 minutes of moderate-intensity aerobic activity weekly (UK Chief Medical Officers' Physical Activity Guidelines), incorporate resistance training at least twice weekly to preserve muscle mass, which supports metabolic rate. Find activities you genuinely enjoy, whether walking, swimming, cycling, dancing, or team sports, as enjoyment predicts long-term adherence. Even small increases in daily movement—taking stairs, walking during lunch breaks, or active hobbies—contribute meaningfully to energy expenditure.
Behavioural strategies and psychological support often determine long-term success. Self-monitoring through regular weighing (weekly rather than daily to avoid obsessive patterns) helps detect early weight regain when intervention is most effective. Identify and address emotional eating triggers, developing alternative coping mechanisms for stress, boredom, or difficult emotions. Cognitive behavioural therapy techniques can be particularly helpful for changing thought patterns around food and body image.
If weight regain occurs despite consistent lifestyle efforts, discuss options with your healthcare provider. These may include consideration of restarting weight loss medications (subject to meeting NICE eligibility criteria and local prescribing policies) or referral to specialist NHS weight management services. Remember that obesity is a chronic condition, and requiring ongoing medical support is neither a failure nor unusual—it reflects the complex biological, psychological, and environmental factors that influence body weight. Your GP can advise on local NHS weight management services and support options available to you.
No specific tapering is required when stopping semaglutide or liraglutide according to their product licences. Abrupt cessation is generally safe from a physiological perspective, though you should always consult your prescribing healthcare professional before making changes to your treatment.
Weight regain varies considerably between individuals, but clinical studies show patients may regain approximately two-thirds of their lost weight within one year of stopping semaglutide. Appetite typically returns within weeks as the medication clears from the body.
Yes, you may be able to restart weight loss injections if you meet NICE eligibility criteria and local prescribing policies permit. Discuss this option with your GP or specialist, particularly if weight regain occurs despite consistent lifestyle efforts.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.