
Can you take weight loss injections with ulcerative colitis? This question arises as obesity rates increase among inflammatory bowel disease patients, prompting interest in GLP-1 receptor agonists like semaglutide (Wegovy) and liraglutide (Saxenda). Whilst there is no formal contraindication to using these medications in ulcerative colitis, important considerations exist. The gastrointestinal side effects of weight loss injections—including nausea, diarrhoea, and delayed gastric emptying—may complicate symptom management in patients with pre-existing bowel inflammation. Limited clinical evidence in this population means prescribing decisions require careful individualised assessment, ideally involving both gastroenterology and weight management specialists to balance potential benefits against risks.
Quick Answer: There is no formal contraindication to using GLP-1 receptor agonist weight loss injections in patients with ulcerative colitis, but individualised clinical assessment is essential due to limited evidence and potential gastrointestinal side effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly popular for managing obesity. These medications work by mimicking natural hormones that regulate appetite and blood sugar levels, slowing gastric emptying and promoting feelings of fullness. These treatments are UK-licensed for weight management as an adjunct to reduced-calorie diet and increased physical activity in adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities. Saxenda is also licensed for some adolescents according to specific criteria in its Summary of Product Characteristics (SmPC).
NICE Technology Appraisal 875 recommends semaglutide (Wegovy) only within specialist weight management services, with treatment typically limited to a maximum of two years on the NHS.
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterising inflammation and ulceration of the colon and rectum. Patients experience symptoms including bloody diarrhoea, abdominal pain, urgency, and fatigue. The condition follows a relapsing-remitting course, with periods of active disease (flares) and remission. Management typically involves aminosalicylates, corticosteroids, immunosuppressants, or biological therapies, depending on disease severity and extent.
The relationship between obesity and ulcerative colitis is complex. Whilst UC has traditionally been associated with weight loss during active disease, obesity rates among IBD patients have risen in line with general population trends. Some patients may gain weight during remission or following corticosteroid treatment. This creates a clinical scenario where patients with UC may seek weight management solutions, including pharmacological interventions.
Understanding how these weight loss medications interact with the gastrointestinal tract is crucial for patients with pre-existing bowel conditions. The mechanism of action—particularly delayed gastric emptying and effects on gut motility—raises important considerations for those with inflammatory bowel disease.
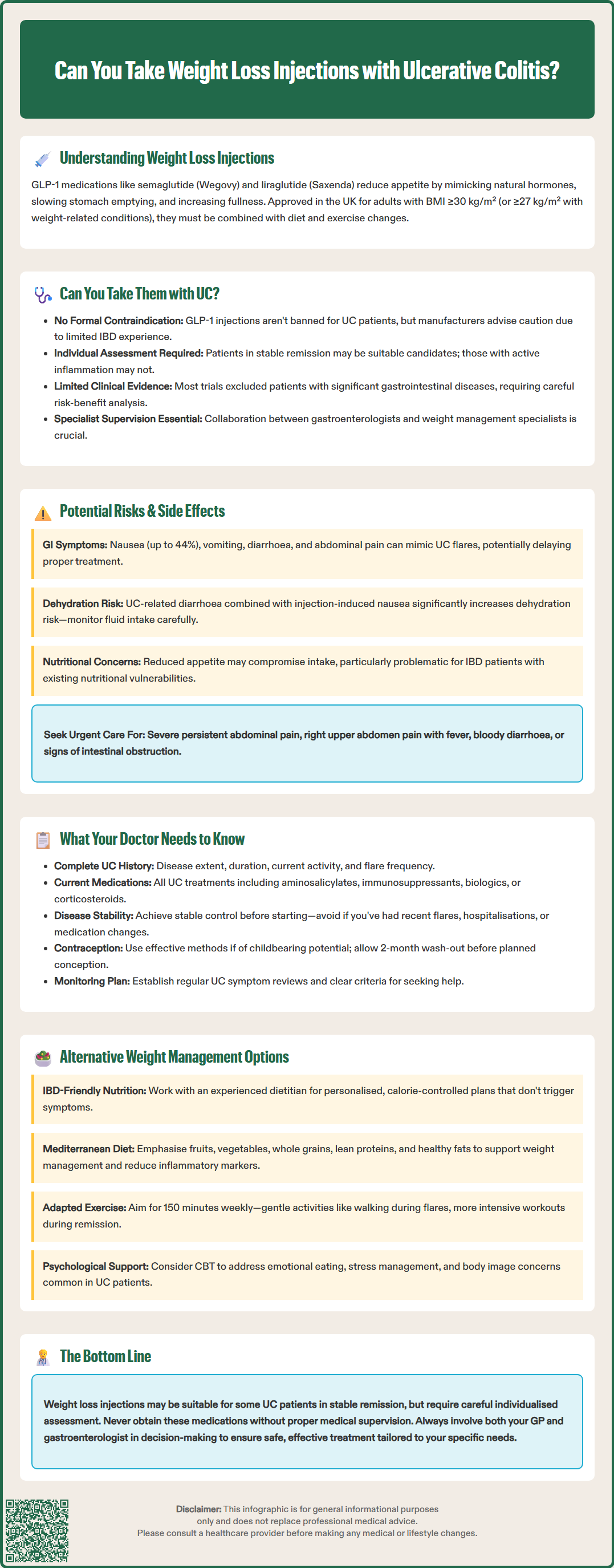
There is no formal contraindication to using GLP-1 receptor agonist weight loss injections in patients with ulcerative colitis. However, the SmPCs for these medications include important cautions regarding use in patients with significant gastrointestinal disease. The liraglutide (Saxenda) SmPC specifically notes limited experience in inflammatory bowel disease and advises against use in certain gastrointestinal conditions. These cautions should be carefully considered when assessing suitability.
The decision to prescribe weight loss injections to someone with ulcerative colitis requires individualised clinical assessment. Key factors include disease activity status, current symptom control, medication regimen, and the patient's overall gastrointestinal tolerance. Patients in stable remission with well-controlled disease may be considered differently from those experiencing active inflammation or frequent flares.
Clinical evidence specifically examining GLP-1 receptor agonists in UC populations remains limited. Most clinical trials for these weight loss medications have excluded patients with significant gastrointestinal diseases, including active IBD. This creates an evidence gap, meaning prescribing decisions must be based on careful risk-benefit analysis rather than robust trial data in this specific population.
NICE guidance on obesity management acknowledges that pharmacological interventions should be considered as part of a multicomponent approach. For patients with comorbidities, including chronic inflammatory conditions, specialist input may be appropriate. In line with NICE TA875, semaglutide (Wegovy) should only be prescribed within specialist weight management services, with treatment typically limited to two years on the NHS.
Gastroenterologists and weight management specialists should ideally collaborate when considering these treatments for UC patients, ensuring both the inflammatory bowel condition and weight management goals are appropriately addressed. This shared decision-making approach is particularly important if your disease is not in stable remission.
Patients should never initiate weight loss injections without medical supervision, particularly when managing a chronic condition like ulcerative colitis. Self-prescribing or obtaining these medications through unregulated sources poses significant safety risks.
Gastrointestinal side effects are the most commonly reported adverse reactions with GLP-1 receptor agonist weight loss injections, occurring in a substantial proportion of users. These include nausea (affecting up to 44% of patients), vomiting, diarrhoea, constipation, abdominal pain, and dyspepsia. The mechanism—delayed gastric emptying and altered gut motility—directly affects the digestive system that is already compromised in ulcerative colitis.
For patients with UC, distinguishing between medication side effects and disease flares presents a significant challenge. Symptoms such as diarrhoea, abdominal cramping, and nausea could indicate either a reaction to the weight loss injection or worsening inflammatory bowel disease. This diagnostic uncertainty may delay appropriate treatment adjustments or lead to unnecessary medication changes.
Dehydration risk warrants particular attention in UC patients using these injections. The combination of UC-related diarrhoea and injection-induced nausea or vomiting can significantly increase fluid loss. Dehydration may worsen UC symptoms, potentially trigger disease flares, and in severe cases lead to acute kidney injury. Patients must maintain adequate hydration and recognise warning signs including reduced urine output, dizziness, or increased thirst.
Gallbladder disease including cholelithiasis (gallstones) and cholecystitis (gallbladder inflammation) has been reported with GLP-1 receptor agonists. Patients should seek prompt medical attention for symptoms such as right upper quadrant pain, fever, or jaundice.
Rare cases of intestinal obstruction or ileus have been reported with these medications. Patients should seek urgent medical assessment for severe, persistent abdominal pain with vomiting or bloating, as distinguishing this from UC-related pain requires clinical evaluation.
There is no established evidence that GLP-1 receptor agonists directly cause or worsen ulcerative colitis inflammation. However, the gastrointestinal side effects could theoretically impact disease management and nutritional status. Some patients may experience reduced appetite to the extent that nutritional intake becomes inadequate, which is particularly concerning for those with IBD who may already have nutritional vulnerabilities.
Pancreatitis, though rare, has been reported with GLP-1 receptor agonists. Patients should be counselled to seek immediate medical attention if experiencing severe, persistent abdominal pain.
Patients taking insulin or sulfonylureas alongside GLP-1 receptor agonists should be aware of potential hypoglycaemia risk and discuss appropriate monitoring with their healthcare team.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Comprehensive disclosure of your complete medical history is essential before starting weight loss injections. Your prescribing doctor must know about your ulcerative colitis diagnosis, including disease extent (proctitis, left-sided colitis, or pancolitis), duration, current disease activity, and frequency of flares. This information helps assess whether you are a suitable candidate for these medications.
Current medication regimens require careful review. Inform your doctor of all UC treatments, including aminosalicylates (mesalazine), immunosuppressants (azathioprine, mercaptopurine), biological therapies (infliximab, adalimumab, vedolizumab), or corticosteroids. While clinically significant interactions with subcutaneous GLP-1 receptor agonists are generally limited, your doctor may wish to review medications with a narrow therapeutic index on a case-by-case basis.
Your doctor should assess recent disease activity and symptom patterns. If you have experienced recent flares, hospitalisations, or changes to UC medication, it may be prudent to achieve stable disease control before introducing weight loss injections. Active inflammation or poorly controlled symptoms increase the risk of complications and make monitoring more difficult.
Medical history of pancreatitis, gallbladder disease, renal impairment, or gastroparesis should be disclosed, as these may influence the suitability of GLP-1 receptor agonists.
Pregnancy planning and contraception are important considerations. GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding. If you are of childbearing potential, effective contraception is advised during treatment. For planned pregnancies, a wash-out period is typically recommended (approximately 2 months for semaglutide) before conception.
Nutritional status and weight history provide important context. Some UC patients experience weight fluctuations related to disease activity, corticosteroid use, or dietary modifications. Your doctor needs to understand whether weight gain is recent, medication-related, or longstanding, and whether previous weight loss attempts have been undertaken.
Establishing a monitoring plan is crucial. This should include regular review of UC symptoms, weight loss progress, gastrointestinal tolerance, and hydration status. Agree on clear criteria for when to contact your gastroenterology team—for example, if you develop bloody diarrhoea, severe abdominal pain, or symptoms suggesting a UC flare. Coordinated care between your GP, gastroenterologist, and weight management service optimises safety and treatment outcomes.
Dietary modification remains a cornerstone of weight management for patients with ulcerative colitis, though it requires careful individualisation. Working with a registered dietitian experienced in IBD can help develop a nutritionally adequate, calorie-controlled eating plan that avoids triggering UC symptoms. Many patients identify specific food triggers during active disease, but dietary restrictions should not be overly restrictive during remission, as this may compromise nutritional status.
The Mediterranean diet pattern—emphasising fruits, vegetables, whole grains, lean proteins, and healthy fats—has shown benefits for both weight management and potentially reducing inflammatory markers. While evidence is supportive, it is not considered disease-modifying for UC. Whilst there is no definitive "UC diet," anti-inflammatory eating patterns may support overall health. Patients should maintain adequate fibre intake during remission, though this may need modification during flares.
Physical activity provides numerous benefits for UC patients, including weight management, improved bone health (important given corticosteroid use), reduced fatigue, and potentially decreased inflammation. NICE recommends adults achieve 150 minutes of moderate-intensity activity weekly. For UC patients, exercise should be tailored to current disease activity—gentle activities like walking or swimming may be more appropriate during flares, whilst more intensive exercise can be pursued during remission.
Psychological support addresses the emotional aspects of weight management and chronic disease. Cognitive behavioural therapy (CBT) can help modify eating behaviours, manage stress (which may influence UC activity), and address body image concerns. Many UC patients experience anxiety or depression, which can affect eating patterns and motivation for lifestyle changes.
Alternative pharmacological options may be considered if lifestyle interventions prove insufficient. Orlistat, which reduces fat absorption, is available but may exacerbate diarrhoea in UC patients and is contraindicated in chronic malabsorption and cholestasis, which may affect some IBD patients. Naltrexone-bupropion (Mysimba) is UK-licensed but not routinely commissioned by NICE; it has important contraindications including uncontrolled hypertension and seizure disorders. Any pharmacological intervention should be discussed with both your GP and gastroenterologist to ensure compatibility with UC management.
Referral to tiered weight management services according to NICE guidance may provide structured support. Bariatric surgery represents another option for severe obesity, though requires specialist multidisciplinary assessment in IBD patients.
There is no formal contraindication, but safety depends on individual disease activity and symptom control. Patients in stable remission may be considered differently from those with active inflammation, and specialist assessment is recommended before starting treatment.
The primary concerns include gastrointestinal side effects (nausea, diarrhoea, abdominal pain) that may be difficult to distinguish from UC flares, increased dehydration risk, and the challenge of monitoring disease activity whilst on treatment.
Yes, collaboration between your gastroenterologist and prescribing doctor is essential to assess your current disease status, review medications, and establish appropriate monitoring plans to ensure both your ulcerative colitis and weight management are safely addressed.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.