
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist widely prescribed for type 2 diabetes mellitus in the UK. Whilst it effectively improves glycaemic control, its mechanism of slowing gastric emptying can cause gastrointestinal side effects. Most digestive symptoms—such as nausea, vomiting, and constipation—are mild and self-limiting. However, recognising the warning signs of serious complications, including bowel obstruction, is essential for patient safety. This article explains how Ozempic affects the digestive system, identifies key symptoms of bowel obstruction, and provides guidance on when to seek urgent medical help.
Quick Answer: Bowel obstruction symptoms in patients taking Ozempic include severe cramping abdominal pain, persistent vomiting, marked abdominal distension, and inability to pass wind or stool—requiring urgent medical assessment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of naturally occurring GLP-1, a hormone that regulates blood glucose levels. Ozempic improves glycaemic control in adults with type 2 diabetes, and while cardiovascular outcomes benefits were observed in clinical trials (SUSTAIN-6), this is not a separate licensed indication in the UK.
The mechanism of action of semaglutide directly influences gastrointestinal function. GLP-1 receptors are abundant throughout the digestive tract, and when activated, they slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying contributes to improved post-prandial glucose control and promotes satiety. However, this same mechanism is responsible for the gastrointestinal side effects commonly reported with Ozempic.
Common digestive effects include:
Nausea (reported in approximately 15-20% of patients according to the SmPC)
Vomiting
Diarrhoea
Constipation
Abdominal discomfort or bloating
These symptoms typically emerge during dose initiation or escalation and often improve over several weeks as the body adapts. The prescribing information recommends gradual dose titration to minimise gastrointestinal intolerance. Whilst most digestive side effects are mild to moderate and self-limiting, there have been very rare post-marketing reports of more serious gastrointestinal complications, including gastroparesis (severe delayed gastric emptying) and intestinal obstruction, though causality has not been established.
Importantly, the SmPC states that Ozempic is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. Healthcare professionals should maintain vigilance for any serious abdominal symptoms in patients taking GLP-1 receptor agonists.
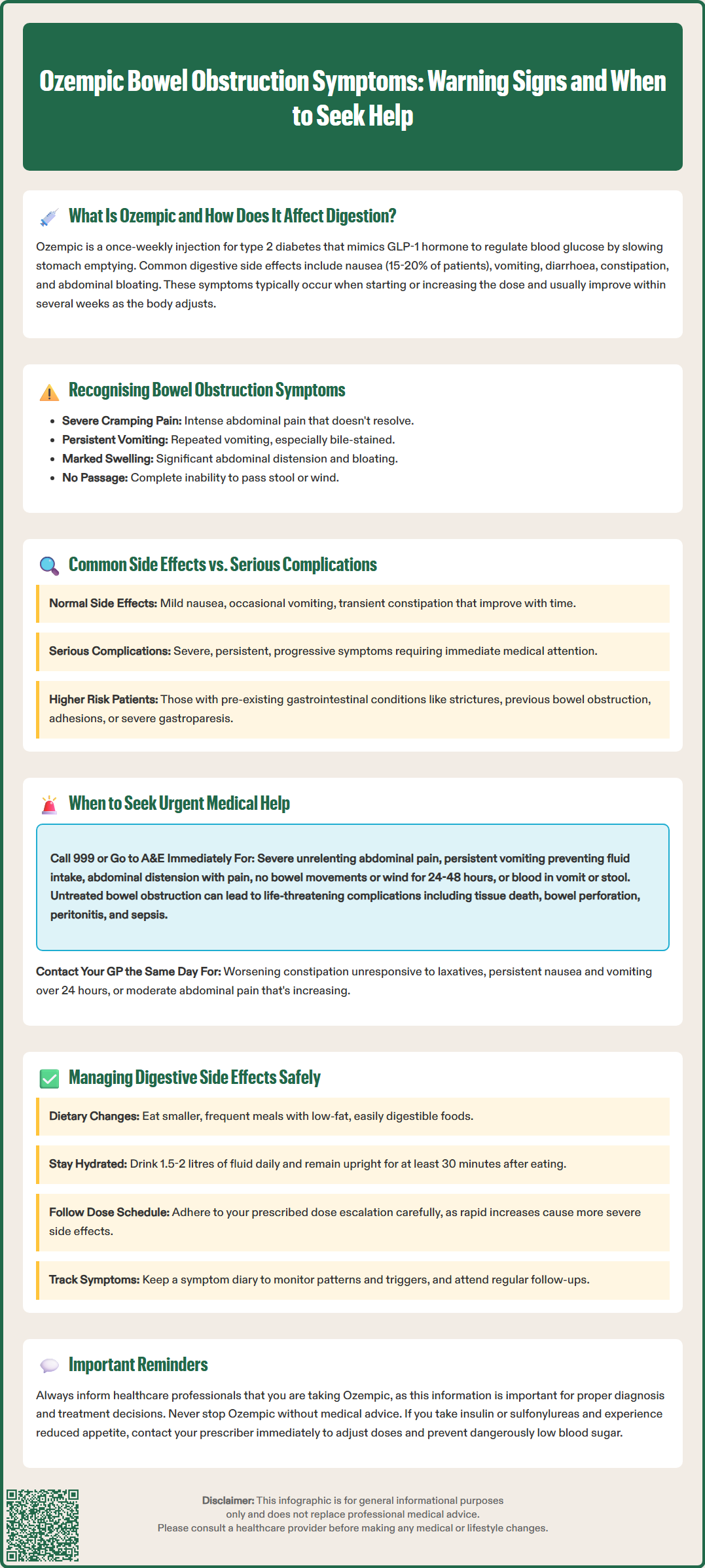
Bowel obstruction—also known as intestinal obstruction—occurs when there is a blockage that prevents the normal passage of digestive contents through the intestines. This can be mechanical (physical blockage) or functional (impaired motility). Whilst bowel obstruction is not listed as a common adverse effect of Ozempic, understanding the warning signs is essential for patient safety, particularly given the drug's effect on gastrointestinal motility.
Key symptoms of bowel obstruction include:
Severe, cramping abdominal pain that comes in waves
Persistent nausea and vomiting, especially if vomit appears bile-stained or faeculent
Marked abdominal distension (swelling or bloating that worsens)
Inability to pass wind or open bowels (absolute constipation)
It is crucial to distinguish between the common, expected side effects of Ozempic—such as mild nausea, occasional vomiting, or transient constipation—and symptoms that may indicate a more serious complication. Mild gastrointestinal symptoms typically improve with time, dietary adjustments, and adequate hydration. In contrast, bowel obstruction symptoms are usually severe, persistent, and progressive.
Patients taking Ozempic who experience severe abdominal pain that does not resolve, repeated vomiting that prevents oral intake, or complete inability to pass stool or flatus should not dismiss these as routine side effects. The slowed gastric emptying caused by semaglutide may theoretically increase the risk of complications in patients with pre-existing gastrointestinal conditions, such as known strictures, previous bowel obstruction, or significant intra-abdominal adhesions. People with severe gastroparesis may warrant a lower threshold for assessment. If you notice a significant change in the pattern or severity of digestive symptoms, it warrants prompt medical assessment.
Recognising when digestive symptoms require urgent medical attention can be lifesaving. Bowel obstruction is a medical emergency requiring urgent hospital assessment; some cases need surgery. If left untreated, it can lead to bowel ischaemia (tissue death), perforation, peritonitis, and sepsis. Patients taking Ozempic should be aware of red flag symptoms that necessitate immediate medical evaluation.
Seek emergency care (attend A&E or call 999) if you experience:
Severe, unrelenting abdominal pain that is not relieved by position changes or over-the-counter analgesia
Persistent vomiting that prevents you from keeping down fluids or medications
Abdominal distension accompanied by severe pain or tenderness
No bowel movements or passage of wind for more than 24–48 hours, especially with pain and vomiting
Signs of dehydration: dizziness, reduced urine output, dry mouth, confusion
Fever in conjunction with severe abdominal symptoms
Blood in vomit or stool, or vomit that looks like coffee grounds
Contact your GP urgently (same day) if you have:
Worsening constipation that does not respond to laxatives
Persistent nausea and vomiting lasting more than 24 hours
Moderate abdominal pain that is increasing in intensity
Inability to tolerate oral fluids
Diagnosis of bowel obstruction typically involves clinical assessment and, where indicated, imaging. CT abdomen/pelvis is commonly used to confirm diagnosis and identify the cause; imaging is guided by clinical judgement. Do not delay seeking help in the hope that symptoms will resolve spontaneously. Early diagnosis and intervention significantly improve outcomes. If you are uncertain whether your symptoms warrant urgent attention, err on the side of caution and contact NHS 111 for advice, or speak to your GP or diabetes specialist nurse. Always inform healthcare professionals that you are taking Ozempic, as this information is relevant to clinical decision-making.
Most patients taking Ozempic will experience some degree of gastrointestinal side effects, but these can often be managed effectively with practical strategies and close communication with healthcare professionals. The goal is to optimise treatment adherence whilst minimising discomfort and reducing the risk of complications.
Dietary and lifestyle modifications:
Eat smaller, more frequent meals rather than large portions, which can exacerbate nausea and delayed gastric emptying
Choose low-fat, easily digestible foods; high-fat meals may worsen nausea and bloating
Stay well hydrated, aiming for at least 1.5–2 litres of fluid daily unless otherwise advised
Increase dietary fibre gradually to help prevent constipation, including fruits, vegetables, and whole grains (if marked bloating or early satiety occurs, very high-fibre foods may aggravate symptoms; consider softer/low-fat options and individualise with clinician/dietitian advice)
Avoid lying down immediately after eating; remain upright for at least 30 minutes post-meal
Limit alcohol and caffeine, which can irritate the digestive system
Medication management:
Follow the dose escalation schedule recommended by your prescriber; rapid dose increases are associated with more severe side effects
If nausea is problematic, discuss anti-emetic medications with your GP. Note that prescription options like domperidone should be used at the lowest effective dose for the shortest duration due to cardiac side effect risks, and metoclopramide is typically limited to short-term use (≤5 days) due to neurological adverse effects
For constipation, consider osmotic laxatives (e.g., macrogol) or stimulant laxatives if needed, but avoid long-term use without medical advice
Do not stop semaglutide without medical advice; if severe or concerning symptoms occur, seek urgent medical help—clinicians may advise withholding the medication
Monitoring and communication:
Keep a symptom diary to track the pattern, severity, and triggers of digestive symptoms
Attend regular follow-up appointments with your GP or diabetes specialist nurse
Report any new or worsening symptoms promptly
Be aware of your individual risk factors for gastrointestinal complications, such as previous abdominal surgery or chronic digestive conditions
If you experience reduced oral intake, contact your prescriber to review insulin or sulfonylurea doses to avoid hypoglycaemia
Report suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app)
NICE recommends individualised treatment plans for people with type 2 diabetes, taking into account tolerability and patient preference. If gastrointestinal side effects remain troublesome despite supportive measures, your healthcare team may consider alternative GLP-1 receptor agonists or other glucose-lowering therapies. Patient safety and quality of life are paramount in diabetes management.
Warning signs include severe cramping abdominal pain, persistent vomiting (especially bile-stained), marked abdominal distension, and complete inability to pass wind or open bowels. These symptoms differ from common Ozempic side effects by being severe, persistent, and progressive, requiring urgent medical assessment.
Attend A&E or call 999 if you experience severe unrelenting abdominal pain, persistent vomiting preventing fluid intake, abdominal distension with severe pain, no bowel movements or wind for 24–48 hours with pain, signs of dehydration, fever with abdominal symptoms, or blood in vomit or stool.
Eat smaller frequent meals, choose low-fat easily digestible foods, stay well hydrated, increase dietary fibre gradually, and follow the recommended dose escalation schedule. Discuss anti-emetic medications or laxatives with your GP if needed, and report any new or worsening symptoms promptly.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.