Weight loss injections such as semaglutide and liraglutide have become increasingly popular for managing obesity in the UK. However, if you have diverticulitis—inflammation of small pouches in the bowel wall—you may wonder whether these medications are safe for you. Whilst there is no specific contraindication preventing their use in people with a history of diverticulitis, careful consideration is essential. These injections can cause gastrointestinal side effects that may overlap with diverticulitis symptoms, and they should be avoided during acute flare-ups. This article explores whether you can take weight loss injections with diverticulitis, the potential risks, and safer weight management alternatives.
Quick Answer: Weight loss injections are not specifically contraindicated in people with diverticulitis, but they should be avoided during acute flare-ups and require careful medical supervision due to overlapping gastrointestinal side effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections have become increasingly popular in the UK for managing obesity and related metabolic conditions. The most commonly prescribed medications include GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda). These medications work by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone that regulates appetite and blood sugar levels. They slow gastric emptying, increase feelings of fullness, and reduce hunger signals to the brain, leading to reduced calorie intake and subsequent weight loss.
Diverticular disease encompasses two conditions: diverticulosis (the presence of small pouches or diverticula in the bowel wall) and diverticulitis, which occurs when these pouches become inflamed or infected. Symptoms of diverticulitis typically include abdominal pain (often in the lower left side), fever, nausea, and changes in bowel habits. The condition can range from mild inflammation managed with supportive care to severe cases requiring antibiotics, hospitalisation or surgery.
The relationship between weight management and diverticular disease is complex. Obesity is recognised as a risk factor for developing diverticulitis and experiencing more severe complications, according to NHS guidance. Maintaining a healthy weight can potentially reduce the frequency and severity of diverticulitis episodes. However, the question of whether weight loss injections are safe and appropriate for individuals with diverticulitis requires careful consideration of how these medications affect the gastrointestinal system and whether they might influence the course of diverticular disease. Understanding both conditions is essential before considering any weight loss treatment.
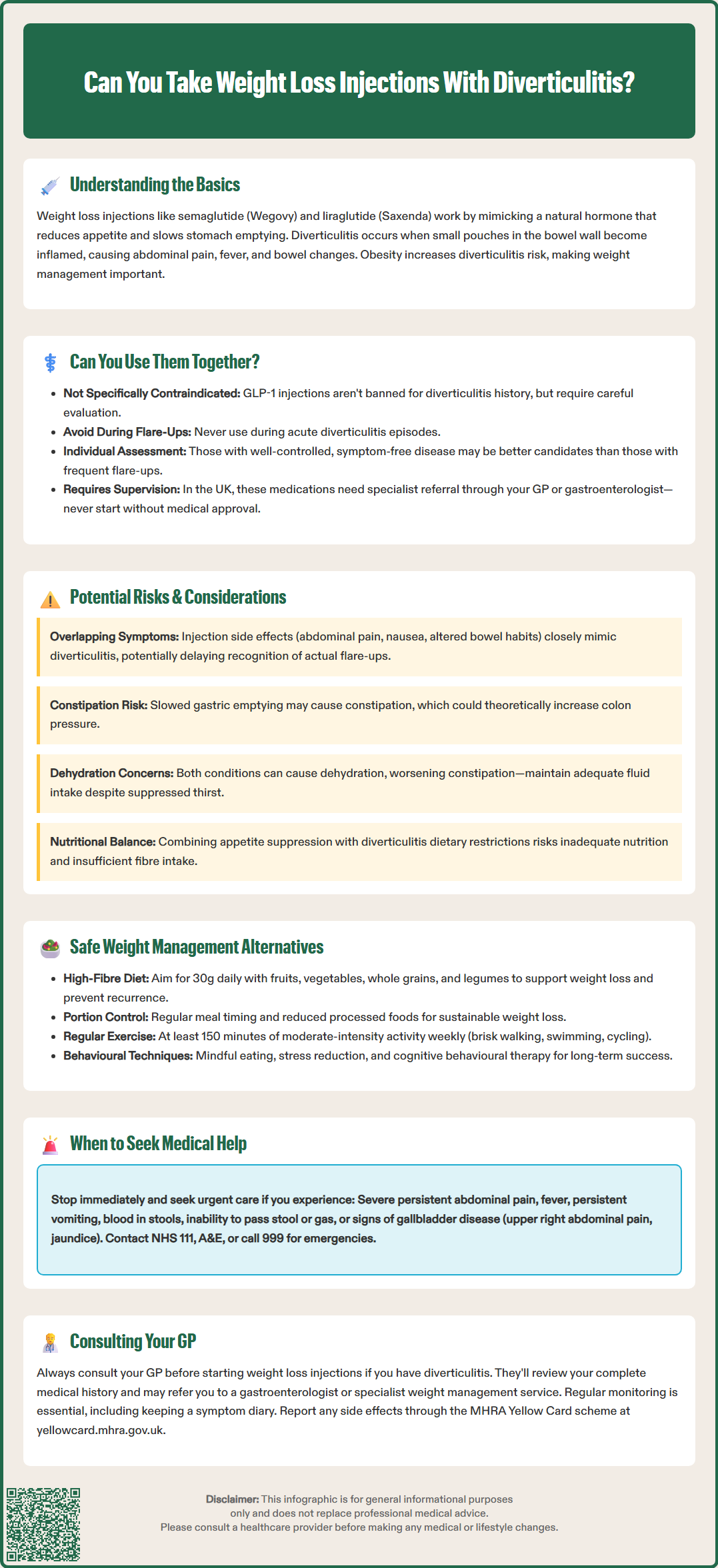
There is currently no specific contraindication preventing the use of GLP-1 receptor agonist weight loss injections in patients with a history of diverticulitis. The MHRA-approved prescribing information for medications like semaglutide and liraglutide does not specifically list diverticulitis as a condition that precludes their use. However, these medications should be avoided during an acute diverticulitis flare-up, and the SmPCs advise caution in people with severe gastrointestinal disease (such as gastroparesis).
The primary consideration centres on the gastrointestinal side effects commonly associated with weight loss injections. GLP-1 receptor agonists frequently cause nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, particularly during the initial weeks of treatment. For someone with active diverticulitis or a recent flare-up, these side effects could potentially exacerbate symptoms or make it difficult to distinguish between medication side effects and disease progression.
Importantly, these medications carry warnings about serious conditions that can present with abdominal pain, including pancreatitis and gallbladder disease. Patients should stop treatment and seek urgent medical advice if they experience severe, persistent abdominal pain (which may radiate to the back) or symptoms of gallbladder disease such as pain in the upper right abdomen, fever, or jaundice.
Individual circumstances matter significantly. A person with well-controlled diverticular disease who has been symptom-free for an extended period may be in a different position compared to someone experiencing frequent flare-ups or who has recently recovered from acute diverticulitis. The decision should be made on a case-by-case basis, taking into account the severity and frequency of diverticulitis episodes, current symptom status, and overall health profile.
In the UK, NICE technology appraisals (TA875 for semaglutide and TA664 for liraglutide) restrict these medications to specialist weight management services with specific eligibility criteria and time-limited treatment courses. Your GP or gastroenterologist is best placed to assess whether weight loss injections are appropriate for your specific situation and can refer you to specialist services if appropriate. Never start weight loss injections without medical supervision, particularly if you have a chronic gastrointestinal condition.
Several important factors require consideration when evaluating weight loss injections for individuals with diverticulitis. Gastrointestinal motility changes represent a primary concern. GLP-1 receptor agonists deliberately slow gastric emptying as part of their mechanism of action. Whilst this contributes to increased satiety and weight loss, it also affects bowel function. Some patients experience constipation, which could theoretically increase intra-colonic pressure and potentially trigger diverticulitis symptoms, though there is no established clinical evidence directly linking these medications to diverticulitis flare-ups.
Distinguishing symptoms poses another challenge. The common side effects of weight loss injections—including abdominal pain, nausea, and altered bowel habits—overlap considerably with diverticulitis symptoms. This similarity could delay recognition of a genuine diverticulitis flare-up, potentially leading to delayed treatment. Additionally, severe, persistent abdominal pain could indicate pancreatitis or gallbladder disease (both recognised risks with GLP-1 receptor agonists) rather than diverticulitis. Patients and clinicians must remain vigilant in monitoring symptoms and maintaining clear communication about any changes.
Nutritional considerations are particularly relevant. During acute diverticulitis, dietary modifications are often recommended, sometimes including a temporary low-fibre or liquid diet. Weight loss injections already reduce appetite and food intake significantly. Combining reduced caloric intake from medication with dietary restrictions for diverticulitis management could potentially lead to inadequate nutrition, particularly regarding fibre intake, which is important for long-term diverticular disease management.
Hydration status requires careful attention. Both diverticulitis and the gastrointestinal side effects of weight loss injections (particularly vomiting and diarrhoea) can affect hydration. Dehydration may worsen constipation, potentially contribute to diverticular complications, and in some cases lead to acute kidney injury. Patients must maintain adequate fluid intake throughout treatment, which can be challenging when appetite and thirst signals are suppressed by medication.
Patients should be alert to signs of possible bowel obstruction or ileus (progressive abdominal distension, inability to pass stool or wind, severe cramping), which require urgent medical assessment and could be confused with diverticulitis symptoms.
For individuals with diverticulitis seeking to lose weight, several evidence-based approaches can be pursued safely alongside appropriate management of their bowel condition. Dietary modification remains the cornerstone of both weight management and diverticular disease control. Current NICE guidance and research support a high-fibre diet for preventing diverticulitis recurrence, though during acute flares, a temporary low-residue diet is often recommended with gradual reintroduction of fibre as symptoms improve. A diet rich in fruits, vegetables, whole grains, and legumes can support both healthy weight loss and digestive health. Aim for 30g of fibre daily, increasing intake gradually to minimise bloating.
Structured eating patterns can facilitate weight loss without requiring medication. Portion control, regular meal timing, and reducing processed foods and added sugars contribute to sustainable weight reduction. Working with a registered dietitian who understands both weight management and diverticular disease can provide personalised guidance that addresses both conditions simultaneously.
Physical activity offers multiple benefits for individuals with diverticulitis. Regular exercise supports weight loss, improves bowel function, and may reduce the risk of diverticulitis complications. The NHS recommends at least 150 minutes of moderate-intensity activity weekly, or 75 minutes of vigorous activity, plus strength exercises on at least two days per week. Activities such as brisk walking, swimming, or cycling are generally well-tolerated and can be adapted to individual fitness levels.
Behavioural approaches including cognitive behavioural therapy (CBT) for weight management, mindful eating practices, and stress reduction techniques can support long-term weight control. Stress may influence both eating behaviours and gastrointestinal symptoms, making these approaches particularly valuable.
If lifestyle modifications prove insufficient, your GP may consider referring you to NHS Tier 2 or Tier 3 weight management services for additional support. If weight loss medication is being considered, alternative options such as orlistat might be discussed. Orlistat works by reducing fat absorption rather than affecting appetite hormones, but it's important to note that it commonly causes gastrointestinal side effects (including steatorrhoea and urgency) and is contraindicated in chronic malabsorption conditions and cholestasis. Any medication approach requires careful medical supervision and consideration of your specific digestive health needs.
Seeking professional medical advice is essential before starting any weight loss treatment when you have diverticulitis. Schedule an appointment with your GP if you are considering weight loss injections and have a history of diverticular disease. Your doctor will need to review your complete medical history, including the frequency and severity of diverticulitis episodes, any complications you have experienced, and your current symptom status.
Specific circumstances requiring urgent consultation include: if you develop severe abdominal pain, fever, persistent vomiting, blood in your stools, or significant changes in bowel habits whilst taking weight loss medication. These symptoms could indicate either a diverticulitis flare-up or serious medication side effects requiring immediate assessment. Contact NHS 111 for urgent advice, or attend A&E or call 999 if you experience severe pain with fever, rigors, marked tenderness, or signs of sepsis. Do not wait for a routine appointment if you experience these warning signs.
Your GP may recommend referral to specialist services depending on your situation. A gastroenterologist can provide expert assessment of your diverticular disease and advise on the safety of weight loss treatments. If weight loss medication is deemed appropriate, you may be referred to a specialist weight management service where healthcare professionals experienced in managing complex cases can provide supervised treatment and monitoring, in line with NICE technology appraisal guidance.
Regular monitoring is crucial if you proceed with weight loss injections. GLP-1 receptor agonist doses are typically escalated gradually with reviews to assess tolerability. Arrange follow-up appointments as recommended by your healthcare team to assess treatment response, monitor for side effects, and ensure your diverticular disease remains stable. Keep a symptom diary noting any abdominal symptoms, bowel habit changes, or concerns that arise during treatment. If you experience significant gastrointestinal adverse effects, your doctor may recommend pausing or reducing the dose.
Remember that weight management is a long-term commitment requiring sustainable approaches. Your GP can help you explore all available options, considering both the potential benefits of weight loss for your overall health and the specific needs related to managing your diverticular disease safely and effectively.
If you suspect you are experiencing side effects from any medication, you can report these through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Weight loss injections are not specifically contraindicated for people with diverticulitis, but they should be avoided during acute flare-ups. Individual assessment by your GP or gastroenterologist is essential, as these medications can cause gastrointestinal side effects that may overlap with diverticulitis symptoms.
The main risks include gastrointestinal side effects such as nausea, constipation, and abdominal pain that may be difficult to distinguish from diverticulitis symptoms. These medications also slow gastric emptying, which could potentially affect bowel function, though no direct link to diverticulitis flare-ups has been established.
Safer options include a high-fibre diet (aiming for 30g daily), regular physical activity (at least 150 minutes of moderate-intensity exercise weekly), portion control, and behavioural approaches such as mindful eating. Working with a registered dietitian and your GP can provide personalised guidance that addresses both weight management and diverticular disease.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.