LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do GLP-1 affect bone density? This question has gained prominence as GLP-1 receptor agonists—medications for type 2 diabetes and weight management—become increasingly prescribed across the UK. Whilst these drugs offer significant metabolic benefits, understanding their potential impact on skeletal health is essential for comprehensive patient care. Current evidence suggests GLP-1 receptor agonists have a neutral effect on fracture risk, though bone mineral density changes may occur indirectly through substantial weight loss. This article examines the research evidence, monitoring recommendations aligned with NICE guidance, and practical strategies for maintaining bone health during GLP-1 treatment.
Quick Answer: GLP-1 receptor agonists do not directly increase fracture risk, but substantial weight loss during treatment may indirectly reduce bone mineral density at weight-bearing sites.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for type 2 diabetes mellitus and, more recently, for weight management in adults with obesity. These drugs mimic the action of the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake.
The mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which stimulates glucose-dependent insulin secretion. This means insulin is released only when blood glucose levels are elevated, reducing the risk of hypoglycaemia compared with some other diabetes medications. However, this risk may increase when GLP-1 receptor agonists are combined with insulin or sulfonylureas, and dose adjustments of these medications may be needed. GLP-1 receptor agonists also suppress glucagon secretion, slow gastric emptying, and promote satiety through central nervous system pathways, leading to reduced appetite and food intake.
GLP-1 receptor agonists available in the UK include:
Semaglutide (Ozempic®, Wegovy®, Rybelsus®) - Ozempic and Rybelsus for diabetes, Wegovy for weight management
Dulaglutide (Trulicity®)
Liraglutide (Victoza®, Saxenda®) - Victoza for diabetes, Saxenda for weight management
Lixisenatide (Lyxumia®)
Exenatide (Byetta®, Bydureon®) - though usage has declined in recent years
These medications are administered either as once-daily, once-weekly, or twice-daily subcutaneous injections, with one oral formulation (semaglutide) also available. NICE guidelines (NG28) recommend GLP-1 receptor agonists for type 2 diabetes based on individual patient factors, including cardiovascular risk, and not strictly as second- or third-line therapy after metformin failure. For weight management, NICE (TA875) provides specific eligibility criteria.
As with all medications, GLP-1 receptor agonists carry potential adverse effects, most commonly gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation. Given their increasing use, understanding their broader metabolic effects—including potential impacts on bone health—has become an important area of clinical and research interest.
Suspected adverse reactions should be reported via the Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
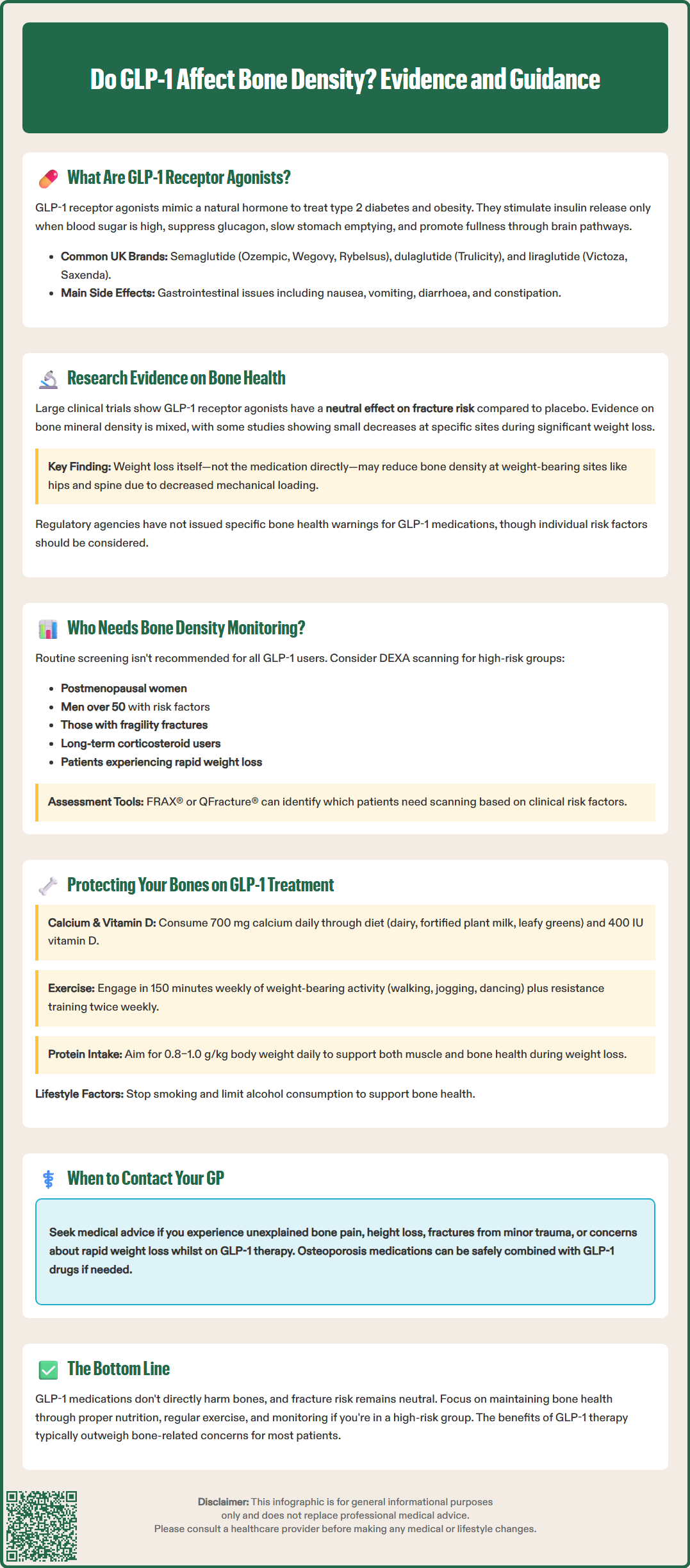
The relationship between GLP-1 receptor agonists and bone density remains an area of ongoing investigation. Current evidence suggests a neutral effect on fracture risk, though findings on bone mineral density (BMD) are mixed, with some studies reporting small site-specific decreases during substantial weight loss.
Preclinical and mechanistic studies have suggested potential interactions between GLP-1 signalling and bone metabolism. While animal studies indicate GLP-1 may influence bone formation and resorption, human data on direct GLP-1 receptor expression in bone cells are limited and findings are mixed. Effects on bone may be indirect, mediated through weight loss, changes in calcitonin, or other pathways rather than direct receptor activation in bone tissue.
Clinical trial data from large cardiovascular outcome studies—including LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide)—have not demonstrated increased fracture risk among patients taking GLP-1 receptor agonists compared with placebo. A meta-analysis published in Diabetes, Obesity and Metabolism found no significant increase in fracture risk associated with GLP-1 therapy.
However, weight loss itself may influence bone health. Substantial weight reduction, regardless of the method, can lead to decreased bone mineral density, particularly at weight-bearing sites such as the hip and spine. This occurs because reduced mechanical loading and changes in hormonal factors (including reduced leptin and oestrogen in adipose tissue) can affect bone remodelling. Patients experiencing rapid or significant weight loss on GLP-1 therapy may therefore face indirect effects on bone health.
Current evidence indicates that MHRA Summaries of Product Characteristics (SmPCs) and European Medicines Agency (EMA) European Public Assessment Reports (EPARs) for GLP-1 receptor agonists do not include specific warnings regarding bone health. Nevertheless, individual patient factors—including age, menopausal status, baseline bone health, and degree of weight loss—warrant consideration in clinical practice.
Routine bone density screening is not currently recommended for all patients taking GLP-1 receptor agonists, as there is insufficient evidence to support universal monitoring based solely on GLP-1 use. However, certain patient groups may benefit from assessment according to existing NICE and UK clinical guidelines for osteoporosis screening (CG146).
Patients who should be considered for bone density assessment include:
Postmenopausal women and men aged over 50 with additional risk factors
Individuals with a history of fragility fractures
Those taking long-term corticosteroids (≥7.5 mg prednisolone daily for ≥3 months)
Patients with conditions affecting bone health, such as rheumatoid arthritis, coeliac disease, or chronic kidney disease
Individuals experiencing rapid or substantial weight loss on GLP-1 therapy
Those with low body mass index (BMI <19 kg/m²)
In line with NICE guidance, fracture risk should not routinely be assessed in people aged under 50 unless they have major risk factors such as previous fragility fracture or prolonged glucocorticoid use.
Dual-energy X-ray absorptiometry (DEXA) scanning remains the gold standard for measuring bone mineral density. NICE recommends using fracture risk assessment tools such as FRAX® (Fracture Risk Assessment Tool) or QFracture® to identify patients who would benefit from DEXA scanning. These tools incorporate clinical risk factors including age, sex, BMI, previous fractures, family history, smoking status, and alcohol intake.
For patients initiating GLP-1 therapy who have pre-existing osteoporosis or osteopenia, baseline DEXA scanning may be appropriate. Rescan timing depends on baseline risk, treatment, and local protocols rather than a fixed interval. Healthcare professionals should document baseline fracture risk and discuss bone health as part of comprehensive diabetes or weight management care.
Patient counselling should include advice on maintaining bone health through adequate calcium and vitamin D intake, weight-bearing exercise, smoking cessation, and moderation of alcohol consumption. If concerns arise regarding bone health during GLP-1 treatment, patients should be advised to contact their GP or diabetes specialist nurse for assessment.
Proactive bone health management is essential for patients taking GLP-1 receptor agonists, particularly those with additional risk factors or experiencing significant weight loss. A multifaceted approach addresses both pharmacological and lifestyle interventions.
Nutritional support forms the foundation of bone health maintenance:
Calcium intake: Adults should aim for 700 mg daily (UK Reference Nutrient Intake) through dietary sources such as dairy products, fortified plant-based alternatives, green leafy vegetables, and tinned fish with bones. Supplementation should only be considered if dietary intake is inadequate.
Vitamin D: UK guidelines recommend 10 micrograms (400 IU) daily for all adults, particularly during autumn and winter months. Patients with deficiency, malabsorption, or limited sun exposure may require higher doses (typically 800–2,000 IU daily).
Protein intake: Adequate protein (0.8–1.0 g/kg body weight daily) supports both muscle and bone health, which is particularly important during weight loss.
Physical activity plays a crucial role in maintaining bone density:
Weight-bearing exercises such as walking, jogging, dancing, and stair climbing stimulate bone formation
Resistance training with weights or resistance bands helps maintain both muscle mass and bone strength
Balance exercises reduce fall risk, particularly important for older adults
In line with UK Chief Medical Officers' guidelines, patients should aim for at least 150 minutes of moderate-intensity activity weekly, plus muscle-strengthening activities on at least two days per week. Older adults should also incorporate balance exercises.
Pharmacological interventions may be necessary for patients with established osteoporosis or high fracture risk. Bisphosphonates (such as alendronic acid) remain first-line treatment for osteoporosis and can be safely co-prescribed with GLP-1 receptor agonists. For patients with severe osteoporosis or very high fracture risk, NICE-approved anabolic therapies may be appropriate, including teriparatide, abaloparatide, or romosozumab. Other options include denosumab, raloxifene, or hormone replacement therapy in appropriate candidates. GLP-1 receptor agonists have no known adverse interactions with osteoporosis medicines, though management of GI symptoms may be important for optimising adherence to oral bisphosphonates.
Regular clinical review should include:
Assessment of weight loss trajectory and nutritional status
Evaluation of fall risk, particularly in older adults
Review of concomitant medications affecting bone health
Monitoring for new fractures or bone pain
When to seek medical advice: Patients should contact their GP if they experience unexplained bone pain, height loss, new fractures from minimal trauma, or concerns about rapid weight loss. Healthcare professionals should maintain a low threshold for referring patients with complex bone health needs to endocrinology or metabolic bone disease specialists.
By integrating these strategies, clinicians can support patients in achieving the metabolic benefits of GLP-1 therapy whilst safeguarding long-term skeletal health.
Routine bone density scanning is not recommended based solely on GLP-1 use. However, you should follow NICE guidance for osteoporosis screening if you have additional risk factors such as being postmenopausal, having a history of fragility fractures, taking long-term corticosteroids, or experiencing rapid weight loss.
Yes, osteoporosis medications such as bisphosphonates can be safely co-prescribed with GLP-1 receptor agonists. There are no known adverse interactions between these drug classes, though managing gastrointestinal symptoms may help optimise adherence to oral bisphosphonates.
Maintain bone health through adequate calcium (700 mg daily) and vitamin D (10 micrograms daily) intake, regular weight-bearing and resistance exercise, smoking cessation, and moderate alcohol consumption. Ensure sufficient protein intake (0.8–1.0 g/kg body weight daily), particularly during weight loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.