GLP-1 receptor agonists such as semaglutide, liraglutide and dulaglutide are increasingly prescribed for type 2 diabetes and weight management in the UK. As their use expands, questions naturally arise about potential side effects, including whether GLP-1 drugs cause blood clots. Current evidence from large-scale clinical trials and regulatory surveillance does not establish a causal link between GLP-1 receptor agonists and increased risk of venous thromboembolism (deep vein thrombosis or pulmonary embolism). This article examines the cardiovascular effects of these medications, the underlying clotting risks in diabetes and obesity, and when to seek medical advice whilst taking GLP-1 therapy.
Quick Answer: Current evidence does not show that GLP-1 receptor agonists cause blood clots or increase the risk of venous thromboembolism.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGLP-1 receptor agonists are a class of medications that mimic the action of glucagon-like peptide-1, a naturally occurring hormone in the body. These medicines are primarily prescribed for the management of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities.
The mechanism of action involves binding to GLP-1 receptors found throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. When activated, these receptors trigger several beneficial effects:
Enhanced insulin secretion in response to elevated blood glucose levels
Suppression of glucagon release, reducing hepatic glucose production
Delayed gastric emptying, which promotes satiety and reduces appetite
Direct effects on appetite centres in the hypothalamus, leading to reduced food intake
Commonly prescribed GLP-1 receptor agonists available in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta, Bydureon). These medications are administered either as subcutaneous injections (weekly or daily, depending on the formulation) or as oral tablets in the case of oral semaglutide (Rybelsus).
According to NICE guidelines (NG28), GLP-1 receptor agonists are typically considered when triple therapy is not effective, not tolerated or contraindicated for type 2 diabetes. Treatment should continue only if there is a clinically meaningful response (for example, HbA1c reduction ≥11 mmol/mol and weight loss ≥3% at around 6 months).
For weight management, NICE (TA664) recommends these medications within specialist weight management services for people with a BMI of at least 35 kg/m² (or 32.5 kg/m² in people from minority ethnic backgrounds) with non-diabetic hyperglycaemia and a high risk of cardiovascular disease, or a BMI of at least 30 kg/m² with type 2 diabetes.
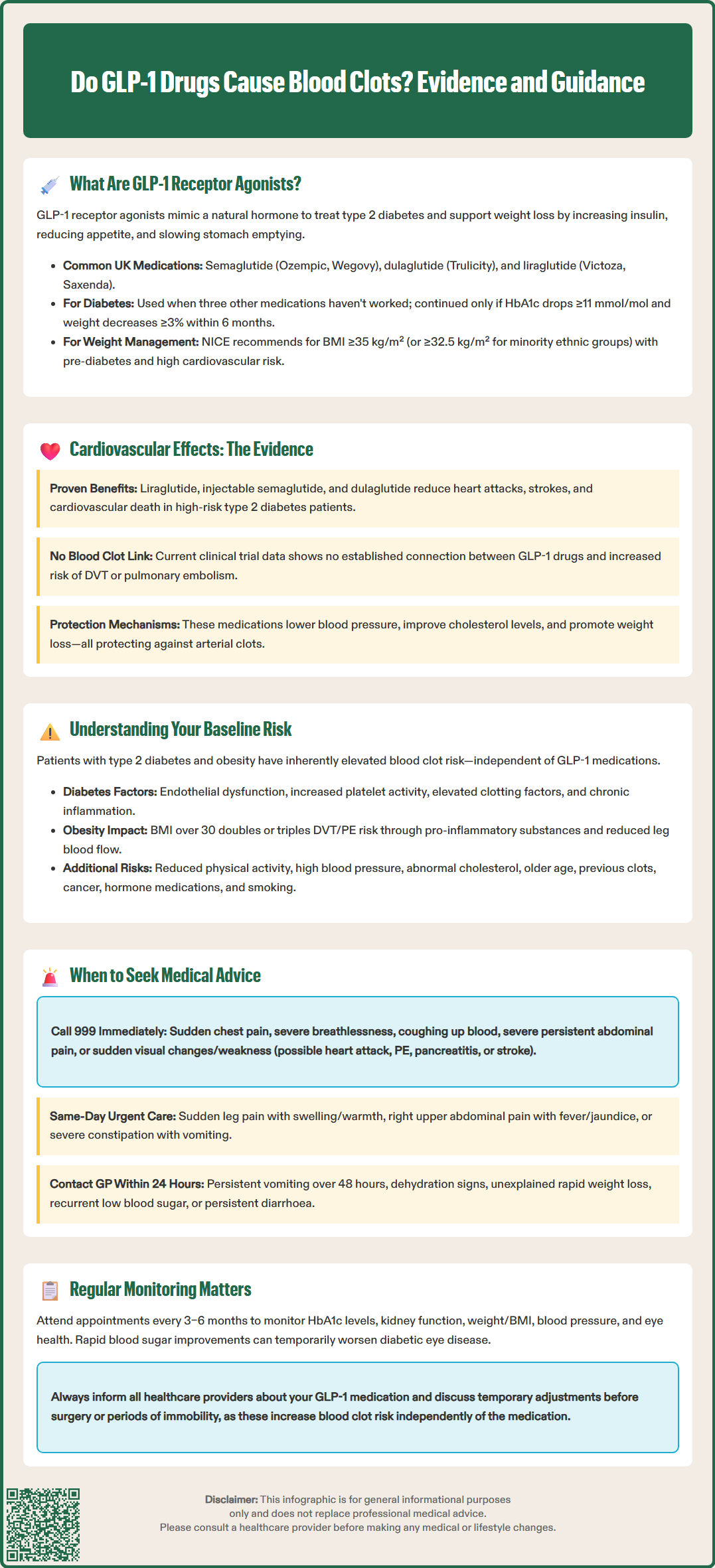
Extensive cardiovascular outcome trials have demonstrated that certain GLP-1 receptor agonists can reduce cardiovascular risk. Major studies including LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide) have shown significant reductions in major adverse cardiovascular events (MACE) in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors. It's important to note that cardiovascular risk reduction is not a class-wide effect; liraglutide (Victoza), injectable semaglutide (Ozempic) and dulaglutide (Trulicity) have specific cardiovascular risk-reduction indications, while exenatide and oral semaglutide (Rybelsus) do not.
Regarding the specific concern about blood clots (venous thromboembolism), there is no established causal link between GLP-1 receptor agonists and increased thrombotic risk. Current evidence from large-scale clinical trials and post-marketing surveillance has not shown an increased risk of deep vein thrombosis (DVT) or pulmonary embolism (PE) with these medications. The MHRA and EMA have not issued warnings regarding thrombotic events as a class effect of GLP-1 receptor agonists.
The cardiovascular benefits observed with these medications include:
Reduction in non-fatal myocardial infarction and stroke
Decreased cardiovascular mortality in high-risk populations (demonstrated with liraglutide)
Improvements in blood pressure and lipid profiles
Weight reduction, which independently lowers cardiovascular risk
It is important to distinguish between arterial thrombotic events (such as heart attacks and strokes, which some GLP-1 agonists help prevent) and venous thromboembolism (DVT and PE). The mechanisms and risk factors for these two types of clotting disorders differ substantially. While evidence suggests GLP-1 receptor agonists have protective effects against arterial disease, the evidence specifically examining venous thrombosis risk is more limited, though no safety signals have emerged.
Patients with type 2 diabetes and obesity—the primary conditions for which GLP-1 receptor agonists are prescribed—have inherently elevated baseline risk for both arterial and venous thrombotic events. Understanding this underlying risk is crucial when evaluating any perceived association between these medications and blood clots.
Diabetes-related thrombotic risk factors include:
Hyperglycaemia-induced endothelial dysfunction, promoting a prothrombotic state
Increased platelet reactivity and aggregation
Elevated levels of clotting factors including fibrinogen and von Willebrand factor
Chronic inflammation with raised inflammatory markers
Impaired fibrinolysis, reducing the body's ability to break down clots
Obesity independently increases thrombotic risk through multiple mechanisms. Adipose tissue produces pro-inflammatory cytokines and adipokines that promote coagulation. Excess weight is associated with venous stasis, particularly in the lower limbs, and obesity is a well-established risk factor for venous thromboembolism. Studies indicate that individuals with a BMI over 30 kg/m² have approximately two to three times higher risk of developing DVT or PE compared to those with normal weight.
Additional risk factors commonly present in patients prescribed GLP-1 receptor agonists include:
Reduced physical activity and prolonged immobility
Hypertension and other cardiovascular comorbidities
Dyslipidaemia contributing to atherosclerosis
Advanced age, as thrombotic risk increases with ageing
Other important VTE risk factors include:
Previous VTE or family history of clotting disorders
Thrombophilia (inherited or acquired clotting disorders)
Active cancer or cancer treatment
Oestrogen-containing medications (HRT, combined oral contraceptives)
Pregnancy and postpartum period
Recent surgery, trauma or hospitalisation
Long-haul travel with prolonged immobility
Smoking
When patients taking GLP-1 receptor agonists experience thrombotic events, it is important to consider these pre-existing risk factors as they often contribute significantly to clotting risk in this population.
Whilst GLP-1 receptor agonists are generally well-tolerated, patients should be aware of warning signs that require prompt medical attention. Understanding when to contact your GP or seek emergency care ensures appropriate management of potential complications, whether related to the medication or underlying conditions.
Seek immediate medical attention (call 999 or attend A&E) if you experience:
Sudden chest pain or pressure, particularly if radiating to the arm, jaw, or back
Severe breathlessness or difficulty breathing at rest
Coughing up blood or experiencing sharp chest pain when breathing (possible PE)
Severe, persistent abdominal pain, particularly if radiating to the back (potential pancreatitis)
Visual changes or sudden weakness on one side of the body (possible stroke)
Seek urgent same-day assessment (contact GP, NHS 111 or local DVT clinic) for:
Sudden leg pain, swelling, warmth, or redness, especially if unilateral (signs of possible DVT)
Right upper abdominal pain with fever or yellowing of skin/eyes (possible gallbladder disease)
Severe constipation with abdominal distension and vomiting (possible ileus)
Contact your GP or diabetes specialist nurse within 24 hours for:
Persistent nausea or vomiting lasting more than 48 hours
Signs of dehydration including reduced urination, dizziness, or extreme thirst
Unexplained rapid weight loss or inability to maintain adequate nutrition
Recurrent hypoglycaemia (blood glucose below 4 mmol/L), especially if taking insulin or sulfonylureas
Persistent diarrhoea affecting daily activities
Routine monitoring whilst taking GLP-1 receptor agonists should include regular review of:
HbA1c levels (typically every 3–6 months)
Renal function (note: exenatide is contraindicated if eGFR <30 mL/min/1.73 m²; other GLP-1 RAs generally require no dose adjustment in renal impairment)
Weight and BMI to assess treatment response
Blood pressure and cardiovascular risk factors
Eye examinations, particularly if you have pre-existing diabetic retinopathy, as rapid improvements in blood glucose can temporarily worsen retinopathy
Patients should inform healthcare providers about all medications they are taking, as drug interactions can occur. If planning surgery or facing prolonged immobility, discuss with your doctor whether temporary medication adjustments or thromboprophylaxis measures are appropriate, as these situations increase clotting risk independently of GLP-1 therapy.
If you suspect you are experiencing side effects from your medication, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
No established evidence shows that GLP-1 receptor agonists increase the risk of blood clots. Large clinical trials and post-marketing surveillance have not identified increased venous thromboembolism risk, and regulatory bodies have not issued warnings regarding thrombotic events as a class effect.
Yes, certain GLP-1 receptor agonists (liraglutide, injectable semaglutide and dulaglutide) have demonstrated cardiovascular benefits in major trials, including reduced risk of heart attack, stroke and cardiovascular death in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors.
Seek immediate medical attention for sudden chest pain, severe breathlessness, coughing up blood, sudden leg pain with swelling or warmth, severe persistent abdominal pain, or visual changes and weakness. Contact your GP urgently for unilateral leg swelling, persistent vomiting, or signs of dehydration.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.