
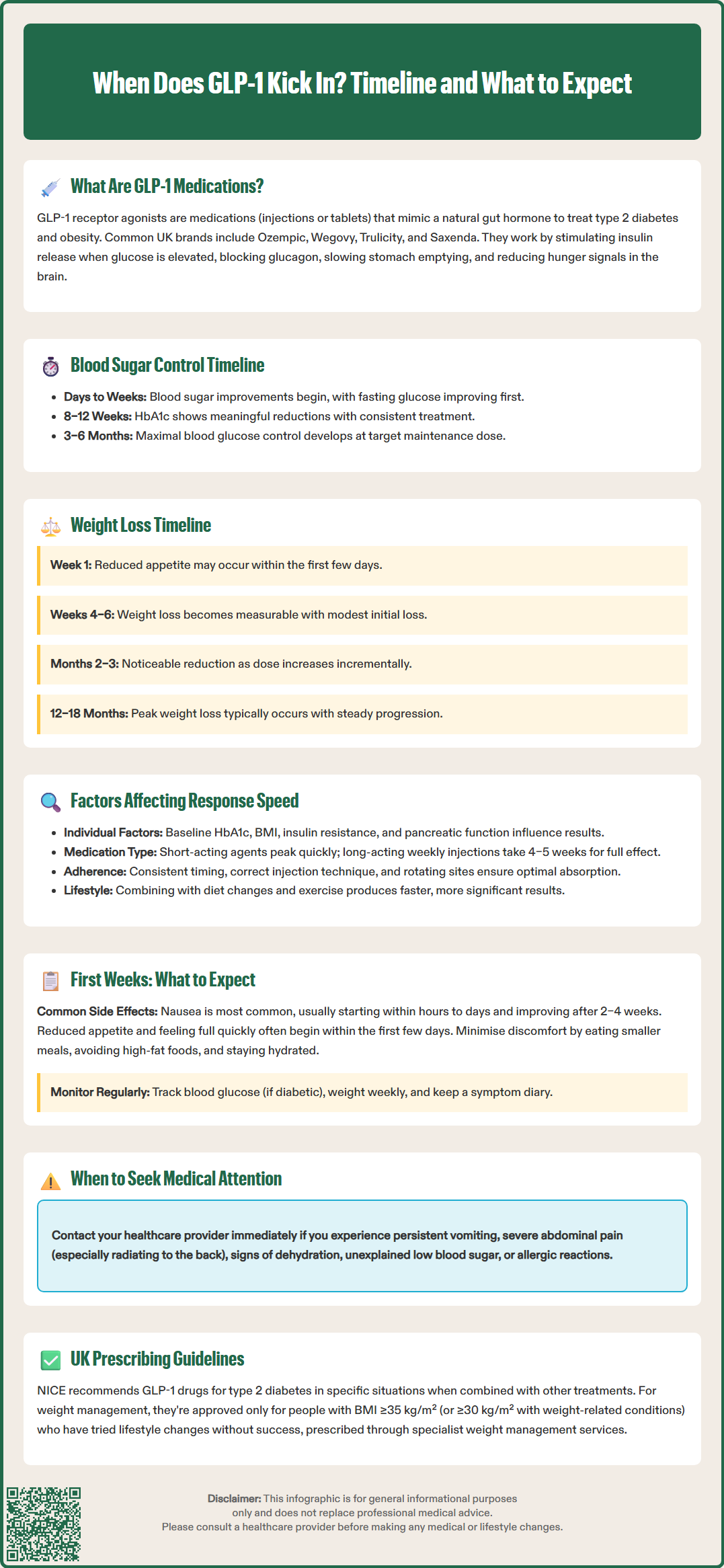
GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda) are increasingly prescribed for type 2 diabetes and weight management in the UK. Understanding when GLP-1 medications begin to work helps set realistic expectations for treatment outcomes. Blood glucose improvements typically emerge within days to weeks, whilst weight loss becomes noticeable after 4–6 weeks. The timeline varies depending on the specific medication, dose escalation schedule, individual metabolic factors, and adherence to lifestyle modifications. This article examines the mechanisms behind GLP-1 therapy and provides evidence-based guidance on what to expect during treatment initiation.
Quick Answer: GLP-1 medications typically improve blood glucose within days to weeks, with full HbA1c reductions after 8–12 weeks, whilst noticeable weight loss usually begins after 4–6 weeks of treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These medicines are available as injections and, in the case of semaglutide (Rybelsus), as an oral tablet. They mimic the action of naturally occurring GLP-1, a hormone produced in the intestines in response to food intake. In the UK, commonly prescribed GLP-1 medications include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide formulations.
The mechanism of action involves several complementary pathways. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they only promote insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications, though the risk increases when combined with insulin or sulfonylureas. Simultaneously, these agents suppress glucagon secretion, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver.
Beyond glycaemic control, GLP-1 medications significantly affect appetite regulation. They slow gastric emptying, prolonging the sensation of fullness after meals, and act on appetite centres in the brain to reduce hunger and food intake. This dual action on metabolism and appetite explains their effectiveness for both diabetes management and weight reduction.
The MHRA has approved various GLP-1 formulations with different dosing schedules—some require daily injections whilst others are administered weekly or taken orally. NICE guidelines (NG28) recommend GLP-1 receptor agonists for type 2 diabetes in specific circumstances, typically in combination with other treatments when certain criteria are met, including BMI thresholds. For weight management, NICE technology appraisals (TA875 for Wegovy, TA664 for Saxenda) specify use within specialist weight management services for people with a BMI of at least 35 kg/m² (or 30 kg/m² with weight-related comorbidities) and following unsuccessful lifestyle interventions.
Understanding when GLP-1 medications begin to work requires distinguishing between their effects on blood glucose control and weight loss, as these occur on different timescales.
Blood sugar improvements typically manifest relatively quickly. Many patients notice measurable reductions in blood glucose levels within days to weeks of starting treatment, with fasting glucose often improving first. However, the full glycaemic benefit develops more gradually. HbA1c—the three-month average blood glucose marker—shows meaningful reductions after approximately 8–12 weeks of consistent treatment. Clinical trials demonstrate that maximal HbA1c reduction usually occurs after 3–6 months of therapy at the target maintenance dose.
Weight loss follows a more gradual trajectory. Patients may notice reduced appetite and smaller portion sizes within the first week, but measurable weight reduction typically becomes apparent after 4–6 weeks. The rate and extent of weight loss varies considerably between individuals and depends on the specific GLP-1 medication and dose. Clinical trials such as the STEP programme (semaglutide) and SUSTAIN studies show that:
Initial weeks: Modest weight loss primarily from reduced caloric intake
Months 2–3: More noticeable reduction becomes evident
Months 3–6: Continued steady weight loss as dose escalates
Months 6–12: Peak weight loss approaches, with most studies showing maximal effect by 12–18 months
It is important to recognise that GLP-1 medications require dose titration—starting at a low dose and gradually increasing over several weeks according to the specific product's SmPC. This staged approach minimises gastrointestinal side effects but means the full therapeutic effect is not immediate. For instance, semaglutide for diabetes (Ozempic) typically starts at 0.25 mg weekly, increasing monthly until reaching the maintenance dose of 1 mg or 2 mg weekly. For weight management (Wegovy), the titration reaches 2.4 mg weekly over several steps.
The speed and magnitude of response to GLP-1 therapy varies significantly between individuals due to multiple physiological and practical factors.
Individual metabolic characteristics play a substantial role. Patients with higher baseline HbA1c levels often experience more dramatic initial improvements in blood glucose control, whilst those with more modest elevations may see smaller absolute changes. Body mass index (BMI) influences weight loss response—individuals with higher BMIs may lose more absolute weight but similar percentages of body weight compared to those with lower BMIs. Insulin resistance severity and pancreatic beta-cell function contribute to individual variability in response.
Medication-specific factors significantly impact onset of action. Different GLP-1 formulations have varying pharmacokinetic profiles as described in their SmPCs:
Short-acting agents reach peak concentrations more quickly
Long-acting weekly injections (semaglutide, dulaglutide) take 4–5 weeks to achieve stable blood levels
Dose escalation schedules deliberately delay full therapeutic effect to improve tolerability
Renal function affects clearance of some agents (particularly exenatide), potentially altering response time
Adherence and administration technique critically affect outcomes. Consistent injection timing, proper subcutaneous technique, and rotating injection sites ensure optimal absorption. Missing doses or irregular administration patterns delay therapeutic benefits and may increase side effects when restarting.
Concurrent lifestyle modifications substantially influence results. Patients who combine GLP-1 therapy with dietary changes and increased physical activity typically experience faster and more pronounced weight loss. The medication enhances the effectiveness of lifestyle interventions rather than replacing them. Conversely, unchanged eating patterns or sedentary behaviour may blunt the weight loss response, though glycaemic benefits generally persist.
Concomitant medications may interact with GLP-1 agents. Drugs affecting gastric emptying or those requiring specific timing relative to meals may need adjustment. Importantly, when GLP-1 medications are added to insulin or sulfonylureas, doses of these medications may need reduction to prevent hypoglycaemia. Your GP or diabetes specialist nurse should review your complete medication regimen when initiating GLP-1 therapy.
Starting GLP-1 therapy represents a significant step in managing diabetes or obesity, and understanding what to anticipate helps ensure realistic expectations and optimal outcomes.
Common early experiences include gastrointestinal symptoms, which affect the majority of patients to some degree. Nausea is the most frequent side effect, typically emerging within hours to days of the first injection and often improving after 2–4 weeks as your body adjusts. Other digestive symptoms may include mild abdominal discomfort, occasional vomiting, or changes in bowel habits (either constipation or loose stools). These effects are generally mild to moderate and can be minimised by:
Eating smaller, more frequent meals
Avoiding high-fat or heavily spiced foods initially
Staying well hydrated
Taking the injection at a consistent time as recommended in the product information
Appetite changes often occur remarkably quickly—many patients report feeling satisfied with smaller portions within the first few days. This is a therapeutic effect rather than a side effect, but the sensation can feel unusual initially. Some describe early satiety (feeling full quickly) or reduced interest in food, particularly high-fat or sweet items.
Monitoring requirements during the initial period include regular blood glucose checks if you have diabetes, particularly if you take insulin or sulfonylureas, as doses may need adjustment to prevent hypoglycaemia. Your healthcare team will provide specific guidance on testing frequency. Weight should be monitored weekly or fortnightly to track progress. Keep a symptom diary noting any side effects, their severity, and duration—this information helps your prescriber optimise your treatment plan.
When to contact your GP or diabetes team:
Persistent vomiting preventing fluid intake
Severe abdominal pain, especially if radiating to the back (possible pancreatitis)
Right upper abdominal pain, fever or jaundice (possible gallbladder problems)
Signs of dehydration (dark urine, dizziness, reduced urination)
Unexplained hypoglycaemia if on combination therapy
New or worsening visual symptoms (especially if you have diabetic retinopathy)
Allergic reactions (rash, swelling, breathing difficulties)
Most patients tolerate GLP-1 medications well once past the initial adjustment period. The gradual dose escalation schedule specifically aims to minimise side effects whilst building towards the therapeutic dose. Patience during these first weeks typically yields substantial long-term benefits for both metabolic control and weight management.
If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk) to help monitor medication safety.
Many patients report reduced appetite and feeling satisfied with smaller portions within the first few days of starting GLP-1 therapy. This early satiety effect is a therapeutic benefit of the medication's action on appetite centres in the brain and gastric emptying.
GLP-1 medications use gradual dose titration over several weeks to minimise gastrointestinal side effects such as nausea whilst allowing your body to adjust. This staged approach improves tolerability and adherence, though it means the full therapeutic effect develops more gradually.
Contact your GP immediately if you experience persistent vomiting preventing fluid intake, severe abdominal pain (especially radiating to the back), signs of dehydration, unexplained hypoglycaemia, new visual symptoms, or allergic reactions. Most side effects are mild and improve within 2–4 weeks.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.