Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have transformed obesity management in the UK, offering significant weight reduction for eligible patients. As GLP-1 receptor agonists become more widely prescribed, questions about potential adverse effects naturally arise. One concern that patients and clinicians encounter is whether these medications increase the risk of kidney stone formation. Whilst no direct causal link has been established by regulatory bodies, understanding the theoretical mechanisms, recognising symptoms, and implementing protective strategies remain essential components of safe treatment. This article examines the current evidence, risk factors, and practical guidance for maintaining kidney health during weight loss therapy.
Quick Answer: Weight loss injections do not have a confirmed direct causal link to kidney stones, though dehydration from gastrointestinal side effects may theoretically increase risk.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections have become increasingly prominent in obesity management across the UK, with medications such as semaglutide (Wegovy) and liraglutide (Saxenda) now available through NHS specialist weight management services and private prescriptions. These medications belong to a class called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management but have demonstrated significant efficacy in weight reduction.
The mechanism of action centres on mimicking the natural hormone GLP-1, which is released by the intestine after eating. These injections work through several pathways: they slow gastric emptying, meaning food remains in the stomach longer, creating prolonged feelings of fullness. They also act on appetite centres in the brain, reducing hunger signals and food cravings. Additionally, GLP-1 receptor agonists improve insulin secretion and reduce glucagon release, helping to regulate blood sugar levels.
Patients typically self-administer these subcutaneous injections once weekly (semaglutide) or once daily (liraglutide), with doses gradually increased over several weeks to minimise gastrointestinal side effects. Clinical trials have shown weight loss of approximately 12-15% of body weight with semaglutide and 5-8% with liraglutide over 12-18 months when combined with lifestyle modifications. According to NICE guidance, semaglutide 2.4 mg (Wegovy) is recommended for adults with a BMI ≥35 kg/m² and at least one weight-related comorbidity, while liraglutide 3 mg (Saxenda) is recommended for adults with a BMI ≥35 kg/m² who have non-diabetic hyperglycaemia and high cardiovascular risk. Lower BMI thresholds apply for certain ethnic groups. Both treatments are typically prescribed within specialist services for up to 2 years.
These medications represent a significant advancement in obesity pharmacotherapy, offering an evidence-based option for individuals who have not achieved adequate weight loss through diet and exercise alone. However, as with all medications, understanding potential adverse effects and monitoring requirements is essential for safe and effective use.
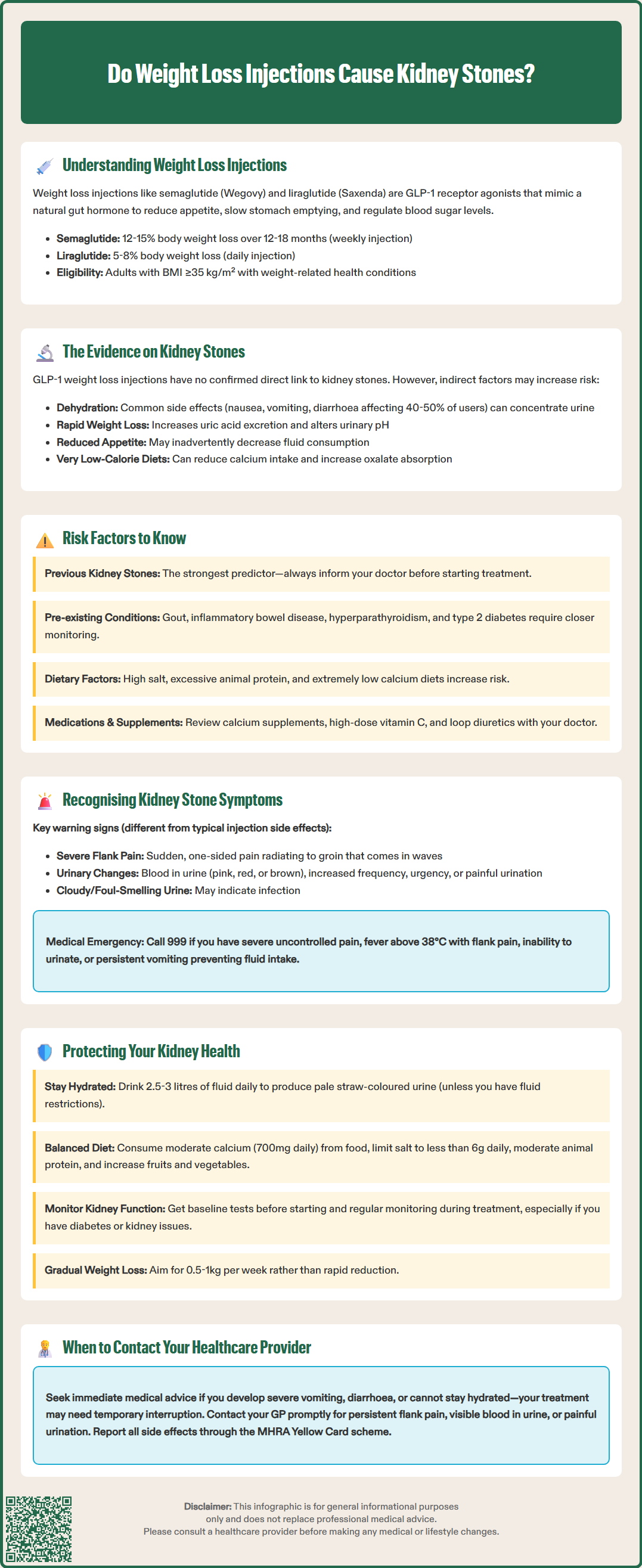
The relationship between GLP-1 receptor agonist weight loss injections and kidney stone formation is not definitively established in current medical literature. There is no official direct causal link confirmed by regulatory bodies such as the MHRA or EMA. However, several mechanisms associated with these medications and rapid weight loss warrant careful consideration.
The primary concern relates to dehydration risk rather than a direct pharmacological effect. GLP-1 receptor agonists commonly cause gastrointestinal side effects, particularly during the initial titration phase. Nausea, vomiting, and diarrhoea affect a substantial proportion of patients—up to 40-50% experience some degree of nausea. These symptoms can lead to reduced fluid intake and increased fluid loss, both of which concentrate the urine and may increase the risk of crystal formation and kidney stone development. Importantly, the Summary of Product Characteristics for both Wegovy and Saxenda warn that acute kidney injury has been reported in association with dehydration from these gastrointestinal adverse events.
Rapid weight loss itself, regardless of the method, has been associated with increased kidney stone risk in some studies. When the body metabolises fat stores quickly, there can be changes in urinary composition, including increased uric acid excretion and alterations in urinary pH. Additionally, some patients may adopt very low-calorie diets alongside these injections, potentially reducing calcium intake and increasing oxalate absorption—both factors that can contribute to calcium oxalate stone formation, the most common type of kidney stone.
Post-marketing surveillance data and ongoing pharmacovigilance have not identified kidney stones as a common adverse effect of GLP-1 receptor agonists. The Summary of Product Characteristics for these medications does not list nephrolithiasis (kidney stones) as a recognised side effect. However, individual case reports exist, and the theoretical mechanisms suggest that maintaining adequate hydration and monitoring kidney function during treatment is prudent clinical practice.
If you experience severe vomiting or diarrhoea while using these medications, contact your healthcare provider promptly, as treatment may need to be temporarily interrupted. You can report any suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Understanding your personal risk factors for kidney stone formation is crucial when considering or using weight loss injections. Previous kidney stone history is the strongest predictor—individuals who have had one kidney stone have a high risk of recurrence. If you have a history of nephrolithiasis, inform your prescribing clinician before starting weight loss therapy.
Several pre-existing medical conditions increase kidney stone risk during weight loss treatment. These include specific kidney conditions such as distal renal tubular acidosis and medullary sponge kidney, gout, hyperparathyroidism, inflammatory bowel disease (particularly Crohn's disease), and recurrent urinary tract infections. Patients with type 2 diabetes—a common indication for GLP-1 therapy—may already have compromised kidney function, making adequate hydration and monitoring even more important.
Dietary factors play a significant role. Low fluid intake is the most modifiable risk factor; individuals with low urine output have substantially higher stone risk. High salt intake increases calcium excretion in urine, whilst excessive animal protein consumption raises uric acid levels. Paradoxically, very low calcium diets can increase oxalate absorption and stone formation. Some patients using weight loss injections may inadvertently adopt extreme dietary restrictions that compound these risks.
Medications and supplements can also contribute. Loop diuretics can increase urinary calcium, whilst thiazide diuretics may actually reduce calcium stone risk. Calcium supplements (especially when taken without food), high-dose vitamin C (which converts to oxalate), and topiramate (not licensed for weight loss in the UK) all increase stone risk. Environmental and lifestyle factors include living in hot climates, occupations involving heat exposure or limited access to fluids, and sedentary behaviour.
Genetic predisposition matters too—family history of kidney stones increases individual risk. Certain ethnic groups and anatomical abnormalities of the urinary tract can also predispose to stone formation. A comprehensive assessment of these factors should inform the decision to proceed with weight loss injections and guide monitoring strategies.
Early recognition of kidney stone symptoms is essential for patients using weight loss injections, as prompt treatment can prevent complications. The classic presentation involves sudden-onset, severe pain in the loin (flank) area, typically on one side, which may radiate to the groin or lower abdomen. This pain, known as renal colic, is often described as one of the most intense pains experienced and typically comes in waves as the stone moves through the urinary tract.
However, distinguishing kidney stone symptoms from the common gastrointestinal side effects of GLP-1 receptor agonists can be challenging. Both conditions may cause nausea and vomiting, but kidney stones typically produce pain that is more severe, localised to the back or side, and associated with urinary symptoms. The pain from kidney stones is usually not relieved by changing position or passing wind, unlike gastrointestinal discomfort.
Urinary symptoms provide important diagnostic clues. These include haematuria (blood in the urine, which may be visible as pink, red, or brown discolouration, or detected only on urine testing), increased urinary frequency, urgency, or painful urination (dysuria). Some patients experience difficulty passing urine or notice cloudy or foul-smelling urine. Fever and chills accompanying these symptoms may indicate infection (pyelonephritis), which requires urgent medical attention. Fever with loin pain and rigors suggests a possible obstructed infected urinary system, which is a urological emergency.
When to seek medical help: Contact your GP promptly if you experience persistent loin pain, visible blood in urine, or pain during urination. Your GP may arrange urine testing, blood tests, analgesia, and urgent imaging such as a non-contrast CT scan when indicated. Seek immediate medical attention (call 999 or attend A&E) if you have severe pain uncontrolled by over-the-counter analgesia, high fever (above 38°C) with loin pain, inability to pass urine, or persistent vomiting preventing fluid intake. Patients with a single functioning kidney or known kidney disease should have a lower threshold for seeking medical review. Keep your healthcare team informed about your weight loss injection therapy, as this context may influence investigation and management decisions.
Maintaining kidney health whilst using weight loss injections requires a proactive, multifaceted approach centred on adequate hydration. For most people, aim for a urine output of more than 2-2.5 litres daily, which typically requires consuming 2.5-3 litres of fluid daily, primarily as water. This dilutes urine and reduces the concentration of stone-forming substances. If you have heart failure, advanced kidney disease, or other conditions requiring fluid restriction, seek personalised advice from your healthcare provider. Spread fluid intake throughout the day rather than consuming large volumes at once. If you experience nausea from your weight loss injection, try small, frequent sips of water, or consider oral rehydration solutions. Urine colour provides a useful guide—aim for pale straw-coloured urine rather than dark yellow.
Dietary modifications support kidney health during weight loss. Maintain moderate calcium intake (approximately 700mg daily) through dietary sources such as dairy products, as adequate calcium binds oxalate in the gut, reducing absorption. Limit salt to less than 6g daily (approximately one teaspoon), as excess salt increases calcium excretion. Moderate animal protein intake and increase consumption of fruits and vegetables, which alkalinise urine and may reduce stone risk. Avoid excessive vitamin C supplements and limit foods high in oxalate (spinach, rhubarb, nuts) if you have a history of calcium oxalate stones.
Medical monitoring is essential. Before starting weight loss injections, baseline kidney function tests (serum creatinine, eGFR) should be performed, particularly if you have diabetes or other risk factors. According to product information, renal function should be monitored if symptoms or signs of dehydration occur, or in those with pre-existing renal impairment, particularly during dose escalation. If you experience severe vomiting or diarrhoea or are unable to maintain adequate hydration, seek clinical advice promptly; your treatment may need to be temporarily interrupted.
Lifestyle measures include maintaining gradual, steady weight loss (0.5-1kg per week is ideal) rather than rapid reduction, which may increase stone risk. Regular physical activity supports overall metabolic health. Avoid prolonged heat exposure without adequate fluid replacement. Keep a symptom diary to distinguish medication side effects from potential kidney problems, and maintain open communication with your healthcare team. If you develop recurrent stones, referral to a urologist or nephrologist for specialist assessment and metabolic stone prevention strategies (including 24-hour urine testing) may be warranted.
No direct causal link has been established by regulatory bodies such as the MHRA or EMA. However, dehydration from common gastrointestinal side effects (nausea, vomiting, diarrhoea) may theoretically increase kidney stone risk by concentrating urine.
Sudden severe loin or flank pain radiating to the groin, blood in urine (pink, red, or brown), increased urinary frequency, and painful urination are key symptoms. Seek immediate medical attention if you experience high fever with loin pain or inability to pass urine.
Maintain adequate hydration (2.5-3 litres daily), ensure moderate dietary calcium intake, limit salt to less than 6g daily, and attend regular kidney function monitoring. Contact your healthcare provider promptly if you experience severe vomiting, diarrhoea, or signs of dehydration.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.