Can you take weight loss injections with kidney disease? This is a crucial question for patients with chronic kidney disease (CKD) considering GLP-1 receptor agonists such as semaglutide (Wegovy), liraglutide (Saxenda), or tirzepatide (Zepbound). Whilst obesity accelerates kidney disease progression and weight loss can benefit renal function, the safety of these medications depends on your stage of CKD. Most GLP-1 agonists require no dose adjustment in mild to severe renal impairment but are not recommended in end-stage renal disease. This article explores which weight loss injections may be suitable, essential medical assessments, monitoring requirements, and alternative weight management strategies for kidney disease patients.
Quick Answer: Most GLP-1 receptor agonist weight loss injections can be used without dose adjustment in mild to severe chronic kidney disease but are not recommended in end-stage renal disease due to limited clinical data.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound), have become increasingly popular for managing obesity. However, patients with kidney disease face unique considerations when contemplating these treatments. The kidneys play a crucial role in drug metabolism and elimination, and impaired renal function can significantly affect how medications behave in the body.
For individuals with chronic kidney disease (CKD), the decision to use weight loss injections requires careful medical evaluation. Whilst obesity itself is a risk factor for kidney disease progression, and weight loss can potentially benefit renal function, the medications used must be appropriate for the patient's level of kidney impairment. The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) provide specific guidance on the use of these medications in patients with varying degrees of renal impairment.
It is essential to understand that kidney disease exists on a spectrum, from mild impairment (stage 1-2 CKD) to end-stage renal disease requiring dialysis (stage 5 CKD), as defined in NICE guideline NG203. The safety and efficacy of weight loss injections can vary considerably depending on the stage of kidney disease. According to their Summary of Product Characteristics (SmPCs), semaglutide and liraglutide do not require dose adjustment in mild to severe renal impairment, though they are not recommended in end-stage renal disease due to limited clinical experience in this population.
Key considerations include:
The stage and severity of your kidney disease
Current kidney function measurements (eGFR and urine albumin-to-creatinine ratio)
Presence of other conditions such as diabetes or cardiovascular disease
Potential drug interactions with existing medications
Patients should never initiate weight loss injections without thorough discussion with their nephrologist or GP, particularly when kidney disease is present.
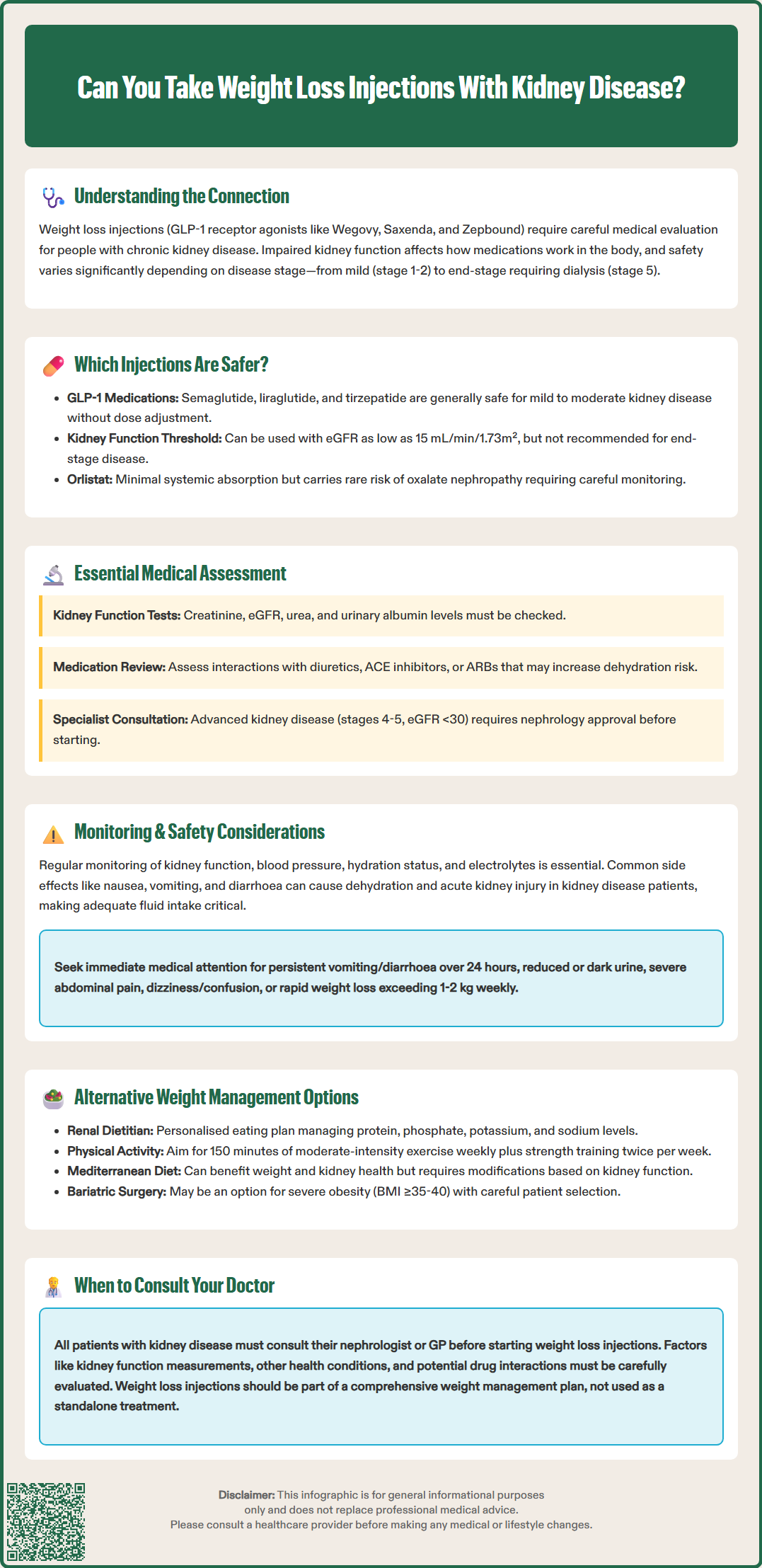
The safety profile of weight loss injections varies significantly depending on the specific medication and the degree of kidney impairment. GLP-1 receptor agonists are the most commonly prescribed weight loss injections and include semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound). These medications work by mimicking the action of naturally occurring hormones that regulate appetite, slow gastric emptying, and enhance insulin secretion.
For patients with mild to moderate kidney disease (eGFR 30-89 mL/min/1.73m²), the licensed weight loss injections are generally considered safer options, as they are primarily metabolised through protein degradation rather than renal excretion. According to their SmPCs, semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Zepbound) can be used without dose adjustment in patients with mild to severe renal impairment (eGFR ≥15 mL/min/1.73m²). However, they are not recommended in end-stage renal disease (eGFR <15 mL/min/1.73m²) due to limited clinical experience in this population.
Liraglutide (Saxenda) has been studied more extensively in patients with renal impairment. The SmPC indicates that no dose adjustment is required for mild to severe renal impairment, though experience in patients with end-stage renal disease is limited. Similarly, semaglutide (Wegovy) does not require dose adjustment in mild to severe CKD, but clinical experience in end-stage kidney disease remains restricted.
Tirzepatide (Zepbound), a newer GLP-1/GIP receptor agonist approved for weight management in the UK, also requires no dose adjustment in renal impairment, though data in end-stage renal disease are limited.
Other weight loss medications, such as orlistat (a lipase inhibitor), work through a different mechanism by reducing fat absorption in the gut. Whilst orlistat has minimal systemic absorption and is not contraindicated in kidney disease, the SmPC notes a risk of rare cases of oxalate nephropathy, particularly in patients with existing kidney problems. This risk necessitates careful consideration and monitoring.
Patients with end-stage renal disease or those on dialysis should generally avoid most weight loss injections unless specifically recommended by their nephrologist, as there is insufficient safety data in this population.
Before initiating any weight loss injection therapy, patients with kidney disease must undergo comprehensive medical assessment. This evaluation ensures that the treatment is appropriate, safe, and likely to provide benefit without exacerbating existing renal impairment. Your healthcare provider will conduct a thorough review of your medical history, current medications, and kidney function status.
Essential baseline investigations include:
Renal function tests: Serum creatinine, estimated glomerular filtration rate (eGFR), and urea levels to determine the stage of kidney disease
Urinary albumin-to-creatinine ratio (uACR): To assess for kidney damage, as recommended in NICE guideline NG203
Electrolyte panel: Sodium, potassium, and bicarbonate levels, as kidney disease affects electrolyte balance
HbA1c and glucose levels: Particularly important if diabetes is present, as this influences treatment choice
Blood pressure monitoring: Hypertension commonly coexists with kidney disease and affects treatment decisions
Cardiovascular assessment: Based on clinical judgement and individual cardiovascular risk factors
Your clinician will also review your medication list to identify potential risks. Certain drugs commonly used in kidney disease, such as diuretics, ACE inhibitors, or angiotensin receptor blockers (ARBs), do not have direct pharmacokinetic interactions with GLP-1 receptor agonists but may increase the risk of dehydration and acute kidney injury if severe gastrointestinal side effects occur.
NICE guidance emphasises the importance of individualised risk-benefit assessment. According to NICE Technology Appraisals TA875 (semaglutide) and TA664 (liraglutide), these medications may be offered to adults with a BMI of at least 35 kg/m² and at least one weight-related comorbidity, or with a BMI of at least 30 kg/m² and at least one weight-related comorbidity for people from certain ethnic backgrounds. For patients with CKD stages 4-5 (eGFR <30 mL/min/1.73m²), specialist nephrology input is essential before considering weight loss injections.
Patients should be prepared to discuss their weight loss goals, previous weight management attempts, dietary habits, and physical activity levels. This holistic assessment ensures that pharmacological treatment is part of a comprehensive weight management strategy rather than a standalone intervention.
Once weight loss injections are initiated in patients with kidney disease, rigorous monitoring is essential to ensure safety and detect any deterioration in renal function early. The frequency and intensity of monitoring should be tailored to the individual's baseline kidney function, with more frequent assessments for those with moderate to severe impairment, guided by NICE guideline NG203 recommendations.
Recommended monitoring includes:
Renal function tests (eGFR and uACR) should be checked at baseline and then at intervals determined by the clinician based on CKD stage, stability, and risk factors
Body weight and BMI tracked regularly to assess treatment efficacy
Blood pressure monitoring at each clinical visit, as weight loss and GLP-1 agonists can affect blood pressure
Hydration status assessment, particularly during the initial weeks when gastrointestinal side effects are most common
Electrolyte monitoring to detect imbalances that may arise from reduced food intake or gastrointestinal symptoms
Common adverse effects of GLP-1 receptor agonists include nausea, vomiting, diarrhoea, and constipation. Whilst these are generally mild and transient, they pose particular risks for kidney disease patients. According to the SmPCs for these medications, severe vomiting or diarrhoea can lead to dehydration and acute kidney injury (AKI), especially in patients with pre-existing renal impairment. Patients should be educated about maintaining adequate fluid intake and recognising warning signs of dehydration.
Additional safety considerations include the risk of pancreatitis and gallbladder disease (including cholelithiasis and cholecystitis), which are noted in the SmPCs. For patients with diabetes, rapid improvement in glycaemic control may be associated with temporary worsening of diabetic retinopathy; appropriate ophthalmological monitoring should be considered.
Red flag symptoms requiring immediate medical attention:
Persistent vomiting or diarrhoea lasting more than 24 hours
Reduced urine output or dark-coloured urine
Severe abdominal pain (potential pancreatitis)
Dizziness, confusion, or extreme fatigue
Rapid weight loss (>1-2 kg per week)
Patients should inform all healthcare providers about their weight loss injection use, especially before procedures requiring fasting or contrast imaging studies, as these can further stress kidney function. Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Dose adjustments or treatment discontinuation may be necessary if kidney function deteriorates significantly during therapy. Regular communication between the prescribing clinician and the patient's nephrologist ensures coordinated care and optimal safety.
For patients with kidney disease who are not suitable candidates for weight loss injections, or who prefer non-pharmacological approaches, several alternative weight management strategies can be effective and safe. NICE guidelines emphasise a multimodal approach to obesity management, with lifestyle modification forming the foundation of treatment.
Dietary interventions are particularly important for kidney disease patients, though they require specialist input. A renal dietitian can develop an individualised eating plan that promotes weight loss whilst adhering to kidney-specific dietary restrictions. This typically involves:
Controlled protein intake (to reduce kidney workload whilst maintaining adequate nutrition)
Phosphate and potassium restriction (depending on CKD stage)
Sodium reduction (to manage blood pressure and fluid retention)
Calorie deficit achieved through portion control and nutrient-dense food choices
The Mediterranean diet has shown benefits for both weight management and kidney health, emphasising plant-based foods, healthy fats, and lean proteins. However, modifications are typically needed based on individual kidney function parameters, and should be implemented under renal dietitian guidance.
Physical activity is crucial for weight management and has additional benefits for kidney disease patients, including improved cardiovascular health, better blood pressure control, and enhanced quality of life. The UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity per week for adults, plus strength activities on at least two days per week. Patients should start gradually, particularly if they have been sedentary, and choose activities appropriate for their fitness level and any mobility limitations. Walking, swimming, and cycling are generally well-tolerated options.
Behavioural interventions such as cognitive behavioural therapy (CBT) for weight management can address psychological factors contributing to obesity. NHS-funded weight management programmes, including group-based interventions and digital platforms, provide structured support and accountability.
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not responded to conservative measures, bariatric surgery may be considered. According to NICE guideline CG189, patients should first be assessed in a Tier 3 specialist weight management service before referral to Tier 4 surgical services. Whilst kidney disease was historically considered a relative contraindication, evidence now suggests that bariatric surgery can be safe and effective in selected CKD patients, potentially even improving renal function. However, this requires careful patient selection and specialist multidisciplinary team assessment.
When to contact your GP or specialist:
If you experience unexplained weight gain or loss
Before starting any new diet or exercise programme
If you develop new symptoms or your existing kidney disease symptoms worsen
To discuss referral to specialist weight management services
Ultimately, the most effective weight management approach for kidney disease patients is one that is sustainable, medically appropriate, and tailored to individual circumstances. Regular follow-up with your healthcare team ensures that your weight management strategy evolves with your changing health needs.
GLP-1 receptor agonists such as semaglutide and liraglutide are generally safe for patients with mild to severe chronic kidney disease (eGFR ≥15 mL/min/1.73m²) without dose adjustment. However, they are not recommended for end-stage renal disease due to limited clinical experience, and specialist nephrology input is essential for advanced CKD.
Patients require regular monitoring of renal function (eGFR and uACR), electrolytes, blood pressure, hydration status, and body weight. Frequency depends on CKD stage, with more intensive monitoring for moderate to severe impairment, as gastrointestinal side effects can cause dehydration and acute kidney injury.
Alternatives include renal dietitian-guided dietary modification (with appropriate protein, phosphate, potassium, and sodium restrictions), regular physical activity (at least 150 minutes weekly), behavioural interventions such as CBT, NHS weight management programmes, and bariatric surgery for selected patients with severe obesity under specialist multidisciplinary assessment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.