
GLP-1 receptor agonists, such as semaglutide and liraglutide, have gained attention for their weight-loss effects, prompting many to ask: does GLP-1 get rid of belly fat? Whilst these medications produce significant overall weight reduction, they do not selectively target abdominal fat. Instead, they promote generalised fat loss throughout the body, including visceral adipose tissue—the metabolically active fat surrounding internal organs. Clinical trials demonstrate substantial reductions in waist circumference and visceral fat alongside total body weight loss. Understanding how these medications work, who can access them, and what realistic outcomes to expect is essential for anyone considering GLP-1 therapy for weight management.
Quick Answer: GLP-1 medications reduce belly fat as part of overall weight loss but do not selectively target abdominal fat.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management but increasingly prescribed for weight management. These injectable medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in regulating blood glucose and appetite.
The mechanism of action involves several physiological pathways. GLP-1 medications bind to GLP-1 receptors in the pancreas, stimulating glucose-dependent insulin secretion whilst simultaneously suppressing glucagon release in a glucose-dependent manner. This dual action helps maintain glycaemic control. Importantly for weight management, these medications also act on receptors in the brain—particularly in the hypothalamus—to reduce appetite and increase feelings of satiety. They additionally slow gastric emptying, which prolongs the sensation of fullness after eating and may affect the absorption of some oral medications.
Currently available GLP-1 medications in the UK include:
Semaglutide (Ozempic for diabetes; Wegovy specifically licensed for weight management)
Liraglutide (Victoza for diabetes; Saxenda specifically licensed for weight management)
Dulaglutide (Trulicity for diabetes only)
Exenatide (Byetta, Bydureon for diabetes only)
Oral semaglutide (Rybelsus for diabetes only)
These medications are administered via subcutaneous injection (except Rybelsus), with dosing frequencies ranging from daily to weekly depending on the specific formulation. The MHRA has approved these agents for specific indications, and NICE provides guidance on their use within the NHS. Whilst they were not specifically designed to target abdominal fat, their overall weight-loss effects naturally include reductions in visceral adipose tissue—the metabolically active fat stored around internal organs in the abdominal cavity.
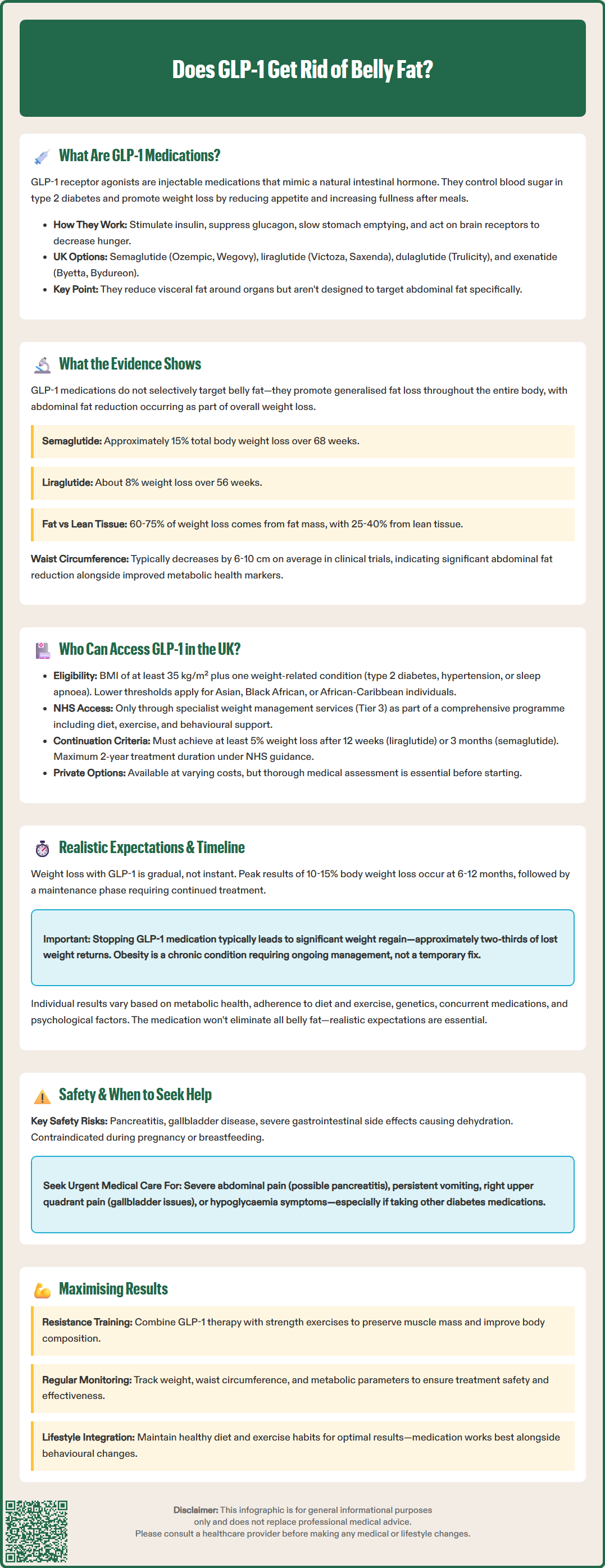
Clinical research demonstrates that GLP-1 receptor agonists produce significant overall weight loss, which includes reductions in abdominal and visceral fat. However, it is important to understand that these medications do not selectively target belly fat—they promote generalised fat loss throughout the body, with abdominal fat reduction occurring as part of this overall process.
The STEP (Semaglutide Treatment Effect in People with obesity) clinical trial programme provides robust evidence. In the STEP 1 trial published in the New England Journal of Medicine (2021), participants receiving semaglutide 2.4 mg weekly achieved an average weight loss of approximately 15% of body weight over 68 weeks, compared to 2.4% with placebo. Body composition substudies using imaging techniques confirmed that visceral adipose tissue decreased alongside total fat mass. Similarly, the SCALE (Satiety and Clinical Adiposity—Liraglutide Evidence) trials published in The Lancet (2015) demonstrated that liraglutide 3.0 mg daily resulted in approximately 8% weight loss over 56 weeks.
Key findings from body composition studies include:
Visceral fat (the deep abdominal fat surrounding organs) decreases alongside subcutaneous fat
Studies suggest that approximately 60-75% of weight loss comes from fat mass, with the remainder from lean tissue
Waist circumference—a proxy measure for abdominal obesity—typically reduces by 6-10 cm on average in clinical trials
Improvements in metabolic parameters often occur alongside reductions in visceral fat
It is worth noting that individual responses vary considerably. Some patients experience more pronounced abdominal fat loss, whilst others may see more uniform distribution of fat reduction. Genetic factors, baseline body composition, adherence to lifestyle modifications, and duration of treatment all influence outcomes. There is no official evidence that GLP-1 medications preferentially mobilise abdominal fat compared to fat in other body regions.
Access to GLP-1 medications for weight management in the UK is governed by specific NICE Technology Appraisals and NHS commissioning policies, which establish strict eligibility criteria. These medications are not available for cosmetic weight loss or for individuals seeking to reduce belly fat alone without meeting clinical thresholds.
NICE Technology Appraisal guidance (TA875 for semaglutide/Wegovy and TA664 for liraglutide/Saxenda) recommends these medications for weight management in adults with:
A body mass index (BMI) of at least 35 kg/m² and
At least one weight-related comorbidity (such as type 2 diabetes, hypertension, dyslipidaemia, obstructive sleep apnoea, or non-alcoholic fatty liver disease)
For liraglutide (Saxenda), NICE TA664 specifies additional criteria including prediabetes (HbA1c 42-47 mmol/mol or fasting plasma glucose 5.5-6.9 mmol/L) or high risk of cardiovascular disease.
For individuals of Asian, Black African, or African-Caribbean family origin, lower BMI thresholds apply (typically 2.5 kg/m² lower) due to increased metabolic risk at lower body weights. Treatment must be initiated within specialist weight management services (Tier 3) as part of a comprehensive programme that includes dietary modification, increased physical activity, and behavioural support. Treatment duration is limited to a maximum of 2 years under NHS guidance.
Treatment continuation requires demonstration of adequate response:
For liraglutide: at least 5% weight loss after 12 weeks at the maintenance dose of 3.0 mg
For semaglutide: assessment after approximately 3 months at the maintenance dose of 2.4 mg, with discontinuation if less than 5% weight loss achieved
Private prescribing is available but costs vary by provider and medication. Patients should be aware that key safety considerations include:
Hypersensitivity to the active substance or excipients
Pregnancy or breastfeeding
Risk of pancreatitis and gallbladder disease
Potential for dehydration with severe gastrointestinal side effects
A thorough medical assessment, including review of current medications and comorbidities, is essential before initiating treatment. Dulaglutide and exenatide are not licensed for weight management in the UK.
Understanding the realistic timeline and expected outcomes with GLP-1 therapy is crucial for patient satisfaction and adherence. Weight loss—including abdominal fat reduction—occurs gradually, and results vary significantly between individuals.
Typical timeline for GLP-1 treatment:
Weeks 0-4: Dose titration begins; appetite suppression starts; minimal weight loss (1-2 kg)
Months 2-3: Noticeable weight reduction (3-5% of body weight); early changes in waist circumference
Months 4-6: Continued steady weight loss; for semaglutide, titration to 2.4 mg maintenance dose typically takes 16 weeks
Months 6-12: Peak weight loss achieved (10-15% for semaglutide; 5-10% for liraglutide)
Beyond 12 months: Weight maintenance phase; continued treatment required to sustain losses
It is essential to recognise that GLP-1 medications are not a permanent solution. Clinical trials demonstrate that discontinuation typically results in weight regain. The STEP 1 extension study showed that patients regained approximately two-thirds of lost weight within one year of stopping treatment. This reflects the chronic nature of obesity as a disease requiring ongoing management.
Factors influencing individual results include:
Baseline metabolic health and insulin resistance
Adherence to dietary and physical activity recommendations
Genetic predisposition to weight loss
Concurrent medications that may affect weight
Psychological factors and eating behaviours
Patients should maintain realistic expectations: whilst significant abdominal fat reduction is achievable, GLP-1 therapy will not produce a flat stomach or eliminate all belly fat, particularly in those with substantial weight to lose. Combining medication with resistance training helps preserve lean muscle mass and may improve body composition outcomes.
When to seek medical attention:
Severe or persistent abdominal pain (stop medication and seek urgent care—potential pancreatitis)
Persistent nausea or vomiting affecting hydration or nutrition
Signs of gallbladder disease (right upper quadrant pain)
Symptoms of hypoglycaemia if taking other diabetes medications
No weight loss after 3 months at maintenance dose
Regular monitoring, including weight, waist circumference, blood pressure, and metabolic parameters, should be conducted throughout treatment to assess efficacy and safety. Doses of insulin or sulfonylureas may need adjustment when starting GLP-1 therapy to reduce hypoglycaemia risk. Patients should report suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Noticeable abdominal fat reduction typically occurs within 2–3 months of starting GLP-1 therapy, with peak weight loss and waist circumference reduction achieved at 6–12 months. Individual results vary based on adherence to lifestyle modifications and baseline metabolic health.
No, NHS access to GLP-1 medications for weight management requires meeting strict criteria: BMI ≥35 kg/m² with at least one weight-related comorbidity, referral to specialist weight management services, and participation in a comprehensive lifestyle programme. These medications are not available for cosmetic purposes or isolated abdominal fat reduction.
Clinical evidence shows that discontinuing GLP-1 therapy typically results in weight regain, with patients regaining approximately two-thirds of lost weight—including abdominal fat—within one year of stopping. Obesity is a chronic condition requiring ongoing management to maintain weight loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.