
Visceral fat—the deep abdominal fat surrounding vital organs—poses serious metabolic risks, including type 2 diabetes, cardiovascular disease, and non-alcoholic fatty liver disease. Does GLP-1 help with visceral fat? Emerging evidence suggests GLP-1 receptor agonists, a class of medications that mimic a natural gut hormone, may reduce visceral adipose tissue alongside overall body weight. These agents work by enhancing insulin secretion, suppressing appetite, and slowing gastric emptying. Whilst licensed in the UK for type 2 diabetes and weight management, their effects on visceral fat specifically remain an area of ongoing research. This article examines the mechanisms, available medications, expected outcomes, and safety considerations for GLP-1 therapy in visceral fat reduction.
Quick Answer: GLP-1 receptor agonists may reduce visceral fat alongside overall weight loss, though preferential visceral fat reduction is not a licensed indication in the UK.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereVisceral fat refers to adipose tissue stored deep within the abdominal cavity, surrounding vital organs including the liver, pancreas, and intestines. Unlike subcutaneous fat that sits just beneath the skin, visceral fat is metabolically active and produces inflammatory substances called adipokines. This type of fat cannot be pinched or easily seen, with accurate measurement requiring imaging techniques such as CT or MRI scans, though waist circumference provides a useful proxy measurement.
The accumulation of visceral fat poses significant health risks that extend far beyond cosmetic concerns. Excess visceral adiposity is strongly associated with:
Type 2 diabetes mellitus and insulin resistance
Cardiovascular disease and hypertension
Non-alcoholic fatty liver disease (NAFLD)
Certain cancers, including colorectal and breast cancer
Metabolic syndrome
According to NHS guidance, waist circumference measurements exceeding 94 cm in men and 80 cm in women (for white European populations) indicate increased metabolic risk, largely driven by visceral fat accumulation. For individuals of South Asian, Chinese, and Japanese origin, these thresholds are lower at 90 cm for men and 80 cm for women, reflecting different body composition patterns and associated health risks.
Visceral fat produces hormones and inflammatory markers that interfere with normal metabolic processes, contributing to insulin resistance and systemic inflammation. UK clinical evidence demonstrates that reducing overall body weight—even modest reductions of 5–10%—can significantly improve metabolic health markers including HbA1c, blood pressure, and lipid profiles. This makes visceral fat reduction a key therapeutic target in managing obesity-related conditions, which is where newer pharmacological interventions such as GLP-1 receptor agonists have shown promise.
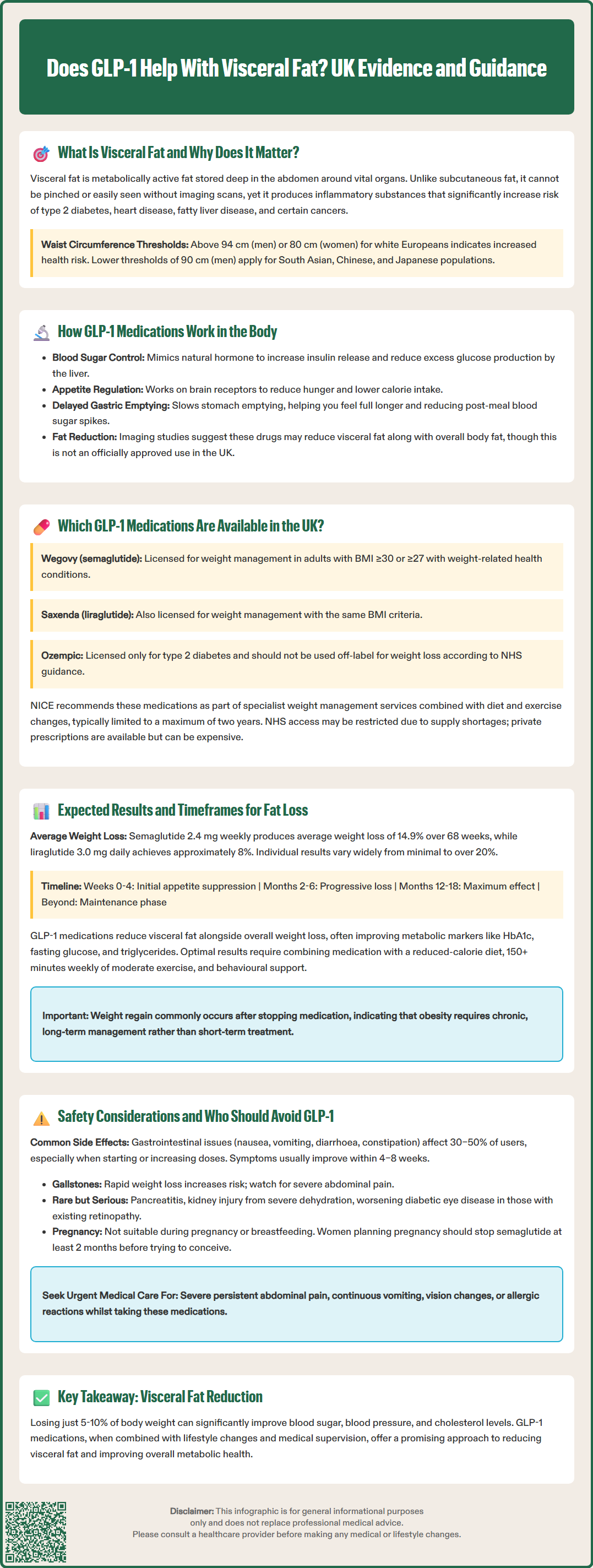
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of naturally occurring GLP-1, an incretin hormone produced by intestinal L-cells in response to food intake. These medications work through multiple complementary mechanisms that collectively promote weight loss and metabolic improvement.
The primary mechanisms of action include:
Enhanced insulin secretion: GLP-1 receptor agonists stimulate glucose-dependent insulin release from pancreatic beta cells, improving glycaemic control without causing hypoglycaemia when glucose levels are normal
Suppressed glucagon secretion: These agents inhibit inappropriate glucagon release from pancreatic alpha cells, reducing hepatic glucose production
Delayed gastric emptying: By slowing the rate at which food leaves the stomach, GLP-1 medications prolong satiety and reduce postprandial glucose excursions
Central appetite regulation: GLP-1 receptors in the hypothalamus and brainstem mediate reduced appetite and food intake, leading to decreased caloric consumption
Regarding visceral fat specifically, some imaging substudies suggest GLP-1 receptor agonists may reduce visceral adipose tissue alongside subcutaneous fat. These findings come from smaller imaging cohorts using computed tomography (CT) and magnetic resonance imaging (MRI), though it's important to note that preferential visceral fat reduction is not a licensed indication for these medications in the UK.
Some research also suggests these medications may have effects on ectopic fat deposition in the liver and pancreas, which could contribute to improved metabolic function. However, these effects are considered investigational and are not licensed indications in the UK. It's worth noting that when GLP-1 receptor agonists are used alongside insulin or sulfonylureas, there is an increased risk of hypoglycaemia, and dose adjustments of these medications may be required.
Several GLP-1 receptor agonists are currently licensed and available through the NHS and private prescribers in the UK, approved by the Medicines and Healthcare products Regulatory Agency (MHRA) for specific indications. These medications differ in their formulation, dosing frequency, and licensed indications.
Currently available GLP-1 receptor agonists include:
Semaglutide (Ozempic®, Wegovy®): Available as once-weekly subcutaneous injection. Ozempic is licensed for type 2 diabetes, whilst Wegovy is specifically licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities. Oral semaglutide (Rybelsus®) is also available for diabetes management.
Dulaglutide (Trulicity®): Once-weekly subcutaneous injection licensed for type 2 diabetes management
Liraglutide (Victoza®, Saxenda®): Daily subcutaneous injection. Victoza is indicated for diabetes, whilst Saxenda is licensed for weight management under similar criteria to Wegovy
Exenatide (Byetta®, Bydureon®): Available as twice-daily or once-weekly formulations for type 2 diabetes
Lixisenatide (Lyxumia®): Once-daily injection for type 2 diabetes
NICE guidance (NG28) recommends GLP-1 receptor agonists for type 2 diabetes management when certain glycaemic and weight criteria are met. For weight management specifically, NICE technology appraisals TA875 (semaglutide 2.4 mg/Wegovy) and TA664 (liraglutide 3 mg/Saxenda) support their use as part of specialist weight management services, alongside dietary modification and increased physical activity. Treatment is typically limited to a maximum of two years.
It is important to note that Ozempic is not licensed for weight management and should not be used off-label for this purpose, in line with NHS supply guidance. Access through the NHS may be limited due to commissioning decisions and ongoing supply constraints. Patients should be assessed by appropriately qualified healthcare professionals, with consideration of contraindications, potential drug interactions, and individual suitability. Private prescription is an alternative route, though costs can be substantial, and patients should discuss availability and costs with their prescriber or pharmacist.
Clinical trial data and real-world evidence provide insight into the magnitude and timeline of weight loss achievable with GLP-1 receptor agonists. Results vary considerably between individuals based on baseline characteristics, adherence, lifestyle modifications, and the specific medication used.
Weight loss expectations:
In landmark trials such as STEP 1 (Semaglutide Treatment Effect in People with obesity) and SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence), participants achieved average weight reductions of 14.9% of initial body weight over 68 weeks with semaglutide 2.4 mg weekly, and approximately 8% with liraglutide 3.0 mg daily. However, individual responses ranged widely, with some participants losing over 20% whilst others experienced minimal benefit.
Some imaging substudies have examined changes in visceral fat during GLP-1 receptor agonist treatment. These smaller studies suggest reductions in visceral adipose tissue alongside overall weight loss, though the magnitude varies between individuals. These changes often correlate with improvements in metabolic markers including HbA1c, fasting glucose, and triglycerides.
Typical timeline:
Weeks 0–4: Initial appetite suppression and modest weight loss, primarily fluid and glycogen
Months 2–6: Progressive weight loss with measurable reductions in waist circumference
Months 6–12: Continued but often slower weight loss, with maximum effect typically achieved by 12–18 months
Beyond 12 months: Weight maintenance phase; continued treatment generally required to sustain losses
It is essential to emphasise that GLP-1 medications are not a standalone solution. Optimal results require:
Adherence to a reduced-calorie diet
Regular physical activity (150+ minutes weekly of moderate intensity)
Behavioural support and lifestyle modification
Ongoing medical supervision
Weight regain commonly occurs following medication discontinuation, highlighting the chronic nature of obesity management.
Whilst GLP-1 receptor agonists demonstrate favourable efficacy for weight loss, they are not suitable for everyone and carry potential adverse effects that require careful consideration and monitoring.
Common adverse effects include:
Gastrointestinal symptoms: Nausea, vomiting, diarrhoea, constipation, and abdominal discomfort affect 30–50% of users, particularly during dose escalation. These typically improve over 4–8 weeks but may necessitate slower titration or discontinuation
Injection site reactions: Erythema, pruritus, or discomfort at injection sites
Fatigue and dizziness: Reported by some patients, particularly initially
Gallbladder disease: Rapid weight loss increases cholelithiasis risk; patients should be counselled about symptoms of biliary colic
Serious but rare adverse effects:
Pancreatitis (discontinue immediately if suspected)
Diabetic retinopathy complications (particularly in patients with pre-existing retinopathy and rapid glycaemic improvement)
Acute kidney injury (usually in context of severe dehydration from vomiting/diarrhoea)
Hypoglycaemia (particularly when used with insulin or sulfonylureas, which may require dose adjustment)
Contraindications include:
Known hypersensitivity to the medication
Pregnancy and breastfeeding (for semaglutide, discontinue at least 2 months before planned conception; check specific SmPC guidance for other agents)
Cautions and special considerations:
Severe gastroparesis or gastrointestinal disease
History of pancreatitis
Renal impairment (specific guidance varies by agent; exenatide is contraindicated if eGFR <30 mL/min/1.73m², while others may be used with caution)
Diabetic retinopathy requiring active treatment
Patients should contact their GP or seek urgent medical attention if they experience:
Severe, persistent abdominal pain (possible pancreatitis)
Persistent vomiting preventing oral fluid intake
Visual changes
Signs of allergic reaction
Regular monitoring should include weight, blood pressure, renal function, and glycaemic parameters in diabetic patients. Healthcare professionals and patients are encouraged to report suspected adverse reactions to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
Semaglutide 2.4 mg (Wegovy) and liraglutide 3.0 mg (Saxenda) are licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities. Treatment should be part of specialist weight management services alongside dietary modification and increased physical activity.
Initial appetite suppression and modest weight loss typically occur within the first 4 weeks. Progressive weight loss with measurable reductions in waist circumference develops over 2–6 months, with maximum effect usually achieved by 12–18 months of treatment.
Gastrointestinal symptoms including nausea, vomiting, diarrhoea, and abdominal discomfort affect 30–50% of users, particularly during dose escalation. These typically improve over 4–8 weeks but may require slower dose titration or, in some cases, discontinuation of treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.