
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide and liraglutide, are increasingly prescribed in the UK for type 2 diabetes and weight management. Emerging research suggests these medications may offer unexpected mental health benefits, with observational studies indicating potential reductions in depression symptoms among users. Whilst GLP-1 agonists are not licensed for treating depression and evidence remains preliminary, their effects on brain regions involved in mood regulation have sparked considerable scientific interest. This article examines the current evidence linking GLP-1 medications to depression, explores potential mechanisms, and provides guidance on when to discuss mental health concerns with your GP.
Quick Answer: Emerging observational evidence suggests GLP-1 receptor agonists may be associated with reduced depression symptoms, though they are not licensed for mental health treatment and require further research.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for managing type 2 diabetes mellitus and, more recently, some have been approved for weight management. In the UK, commonly prescribed GLP-1 agonists include semaglutide (Ozempic for diabetes; Wegovy for weight management), liraglutide (Victoza for diabetes; Saxenda for weight management), and dulaglutide (Trulicity for diabetes only). These medications are administered via subcutaneous injection, typically weekly or daily depending on the specific formulation.
GLP-1 is a naturally occurring incretin hormone released by the intestine in response to food intake. GLP-1 receptor agonists mimic this hormone's action by binding to GLP-1 receptors throughout the body. Their primary mechanisms include:
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner
Suppressing glucagon release, which reduces hepatic glucose production
Slowing gastric emptying, promoting satiety and reducing appetite
Acting on central nervous system pathways involved in appetite regulation
These combined effects lead to improved glycaemic control in people with type 2 diabetes and significant weight reduction in those with obesity. NICE guideline NG28 recommends GLP-1 agonists for type 2 diabetes when metformin and other oral agents prove insufficient, particularly in people with a BMI ≥30 kg/m² (or ≥27.5 kg/m² in certain ethnic groups).
For weight management, NICE technology appraisals TA875 (semaglutide/Wegovy) and TA664 (liraglutide/Saxenda) recommend these medications only within specialist weight management services for adults with a BMI ≥35 kg/m² (or ≥32.5 kg/m² in certain ethnic groups) with weight-related comorbidities, and under specific time-limited conditions.
Interestingly, GLP-1 receptors are not confined to the pancreas and gastrointestinal tract. They are also present in various brain regions, including areas involved in mood regulation, reward processing, and emotional behaviour. This widespread distribution has prompted researchers to investigate whether GLP-1 agonists might influence mental health conditions such as depression.
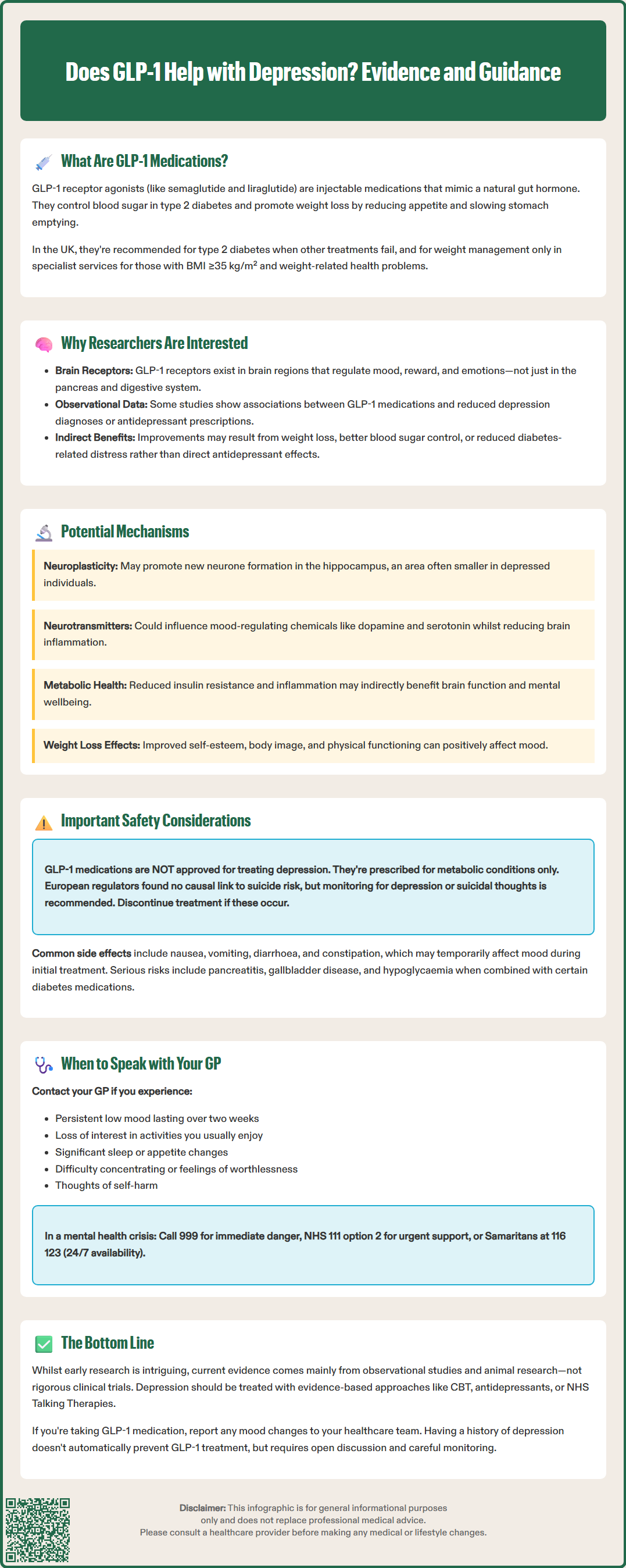
The relationship between GLP-1 medications and depression is an emerging area of clinical research, with accumulating evidence suggesting potential mental health benefits. Several observational studies and database analyses have examined whether people taking GLP-1 agonists experience changes in depressive symptoms compared to those on alternative treatments.
Recent epidemiological research, including studies analysing electronic health records, has identified associations between GLP-1 agonist use and reduced incidence of depression diagnoses or antidepressant prescriptions. Some observational studies suggest a lower risk of new depression diagnoses among GLP-1 users compared to those taking other diabetes or weight-loss medications. However, it is crucial to note that these are observational findings showing correlation rather than causation.
The picture is complicated by several confounding factors:
Weight loss itself is associated with improved mood and reduced depressive symptoms in many individuals
Better glycaemic control may enhance overall wellbeing and reduce diabetes-related distress
Selection bias may exist, as patients with severe mental health conditions might be less likely to be prescribed these medications initially
Currently, there is no official indication for GLP-1 agonists in treating depression, and the MHRA has not licensed these medications for mental health conditions. NICE guideline NG222 for depression in adults does not include GLP-1 receptor agonists among recommended treatments. The evidence base consists primarily of secondary analyses and observational data rather than randomised controlled trials specifically designed to assess antidepressant effects. Nonetheless, the consistency of findings across multiple studies has generated considerable scientific interest and ongoing clinical trials are investigating this potential therapeutic application more rigorously.
Understanding how GLP-1 receptor agonists might influence mood requires examining their effects on brain function and neurochemistry. Several plausible biological mechanisms have been proposed, though research remains at a relatively early stage.
Central nervous system GLP-1 receptors are distributed throughout brain regions implicated in depression, including the hippocampus, prefrontal cortex, and nucleus accumbens. Preclinical studies in animal models suggest that GLP-1 receptor activation may:
Promote neuroplasticity and neurogenesis (formation of new neurons) in the hippocampus, a region often showing reduced volume in depression
Modulate neurotransmitter systems, particularly dopamine and serotonin pathways involved in mood regulation and reward processing
Reduce neuroinflammation, which is increasingly recognised as contributing to depressive disorders
Enhance brain-derived neurotrophic factor (BDNF) expression, a protein crucial for neuronal health and resilience
Metabolic improvements associated with GLP-1 therapy may also contribute indirectly to mood benefits. Obesity, insulin resistance, and chronic hyperglycaemia are all associated with increased inflammation and oxidative stress, which can negatively impact brain function. By addressing these metabolic disturbances, GLP-1 agonists may create a more favourable environment for mental wellbeing.
Additionally, the weight loss achieved with these medications often leads to improved self-esteem, body image, and physical functioning, all of which can positively influence mood. The relationship between physical and mental health is bidirectional and complex.
It is important to emphasise that these mechanisms remain theoretical in humans, derived largely from animal research and indirect evidence. Well-designed clinical trials with depression as a primary outcome measure are needed to establish whether GLP-1 agonists have genuine antidepressant properties independent of their metabolic effects.
Whilst emerging evidence suggests potential mood benefits, GLP-1 agonists are not without adverse effects, and mental health monitoring remains important during treatment. The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, and constipation, which typically diminish over time but can affect quality of life and potentially mood during the initial treatment period.
Several important safety considerations from UK SmPCs include:
Pancreatitis risk: Seek immediate medical attention for severe, persistent abdominal pain
Gallbladder disease: Including cholelithiasis and cholecystitis
Diabetic retinopathy complications: Particularly with semaglutide in those with pre-existing retinopathy
Dehydration and acute kidney injury: Possible with severe gastrointestinal side effects
Hypoglycaemia: Increased risk when used with insulin or sulfonylureas (dose adjustment of these medications may be needed)
Pregnancy/breastfeeding: Weight management GLP-1 agonists (Wegovy, Saxenda) are contraindicated in pregnancy and should be avoided during breastfeeding
Regarding mental health specifically, regulatory agencies have scrutinised GLP-1 medications for potential psychiatric adverse effects. The European Medicines Agency's Pharmacovigilance Risk Assessment Committee (PRAC) reviewed the evidence in 2024 and concluded there is no causal link between GLP-1 receptor agonists and increased suicide risk, though continued monitoring is advised. The SmPCs for weight management products (Wegovy, Saxenda) recommend monitoring for depression or suicidal thoughts and discontinuing treatment if these occur.
Patients starting GLP-1 therapy should be aware of:
Potential mood changes during the adjustment period, particularly if experiencing significant gastrointestinal side effects
The importance of continuing existing mental health treatments unless advised otherwise by their healthcare team
Realistic expectations regarding weight loss and metabolic improvements, as unrealistic goals can lead to disappointment
Healthcare professionals prescribing GLP-1 agonists should:
Screen for depression and anxiety at baseline and during follow-up appointments
Monitor for mood changes, particularly in patients with pre-existing mental health conditions
Ensure coordinated care between diabetes/obesity services and mental health teams when appropriate
It is essential to recognise that GLP-1 agonists are not a substitute for evidence-based depression treatments, including psychological therapies and antidepressant medications when indicated. Any potential mood benefits should be considered an additional effect rather than a primary therapeutic goal.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
If you are experiencing depression or have concerns about your mental health, it is important to discuss these with your GP, regardless of whether you are taking or considering GLP-1 medication. Depression is a common and treatable condition, and effective interventions are available through the NHS.
You should contact your GP if you experience:
Persistent low mood, sadness, or emptiness lasting more than two weeks
Loss of interest or pleasure in activities you previously enjoyed
Significant changes in sleep, appetite, or energy levels
Difficulty concentrating or making decisions
Feelings of worthlessness, excessive guilt, or hopelessness
Thoughts of self-harm or suicide
For immediate mental health crisis:
Call 999 or go to A&E if you or someone else is in immediate danger
Contact NHS 111 and select option 2 for urgent mental health support
Call the Samaritans free on 116 123 (available 24/7)
If you are already taking a GLP-1 agonist and notice mood improvements, this is worth mentioning to your healthcare team, as it may inform your overall treatment plan. Conversely, if you experience mood deterioration after starting these medications, your GP can assess whether this is related to the medication, side effects, or other factors.
For those considering GLP-1 therapy who have a history of depression, discuss this openly with your prescriber. Having depression is not necessarily a contraindication to GLP-1 treatment, but it requires careful consideration and monitoring. Your GP or specialist can help weigh the potential metabolic benefits against any mental health considerations specific to your situation.
NICE guideline NG222 recommends a holistic approach to managing depression, considering both physical and mental health. If you have both metabolic conditions (diabetes or obesity) and depression, integrated care addressing both aspects is ideal. This might involve collaboration between your GP, practice nurse, diabetes specialist, and mental health services to optimise your overall wellbeing.
Many areas offer self-referral to NHS Talking Therapies (formerly IAPT) for evidence-based psychological treatments. Your GP can also provide information about local mental health support services.
Remember that whilst research into GLP-1 and depression is promising, these medications are currently prescribed for metabolic indications. Evidence-based treatments for depression, including cognitive behavioural therapy (CBT), antidepressants, and other psychological interventions, remain the first-line approaches recommended by NICE for managing depressive disorders.
No, GLP-1 receptor agonists are not licensed by the MHRA for treating depression and are not included in NICE guidance for managing depressive disorders. They are approved only for type 2 diabetes and weight management.
Having depression is not necessarily a contraindication to GLP-1 treatment, but it requires careful discussion with your GP or specialist. Mental health monitoring is recommended during therapy, and you should continue any existing depression treatments unless advised otherwise.
Contact your GP if you experience mood deterioration, persistent low mood, or thoughts of self-harm whilst taking GLP-1 medication. For immediate mental health crisis, call 999, contact NHS 111 (option 2), or call Samaritans on 116 123.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.