
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Patients sometimes wonder whether Mounjaro causes high potassium levels, particularly when routine blood tests reveal elevated results. Understanding the relationship between this medication and potassium homeostasis is important for safe prescribing and patient reassurance. Current clinical evidence and regulatory guidance do not identify hyperkalaemia as a recognised adverse effect of tirzepatide. However, patients taking Mounjaro often have comorbidities and concurrent medications that genuinely affect potassium balance, making it essential to consider the broader clinical context when interpreting blood results.
Quick Answer: Mounjaro (tirzepatide) does not cause high potassium levels based on current clinical evidence and regulatory guidance.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. It has also received approval for weight management in adults with obesity or overweight with weight-related comorbidities, as per the MHRA authorisation. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. This dual mechanism distinguishes Mounjaro from other diabetes medications currently available.
The drug works by mimicking two naturally occurring incretin hormones that play crucial roles in glucose regulation and appetite control. When blood glucose levels rise after eating, Mounjaro stimulates insulin secretion from pancreatic beta cells whilst simultaneously suppressing glucagon release from alpha cells. This coordinated action helps lower blood sugar levels in a glucose-dependent manner, which reduces the risk of hypoglycaemia compared to some other diabetes treatments. Additionally, tirzepatide slows gastric emptying and acts on appetite centres in the brain, promoting satiety and reducing food intake.
Mounjaro is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg for 4 weeks, then increasing to 5 mg, with further stepwise increases based on individual response and tolerability. The medication has demonstrated significant efficacy in clinical trials (SURPASS for diabetes, SURMOUNT for weight management), with substantial reductions in HbA1c levels and body weight.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, particularly during dose escalation. Severe gastrointestinal symptoms may lead to dehydration and acute kidney injury in susceptible individuals. There is an increased risk of hypoglycaemia when used with insulin or sulfonylureas, which may require dose adjustment of these medications. Other important safety considerations include risks of pancreatitis and gallbladder disease. Patients should report any suspected side effects via the MHRA Yellow Card scheme.
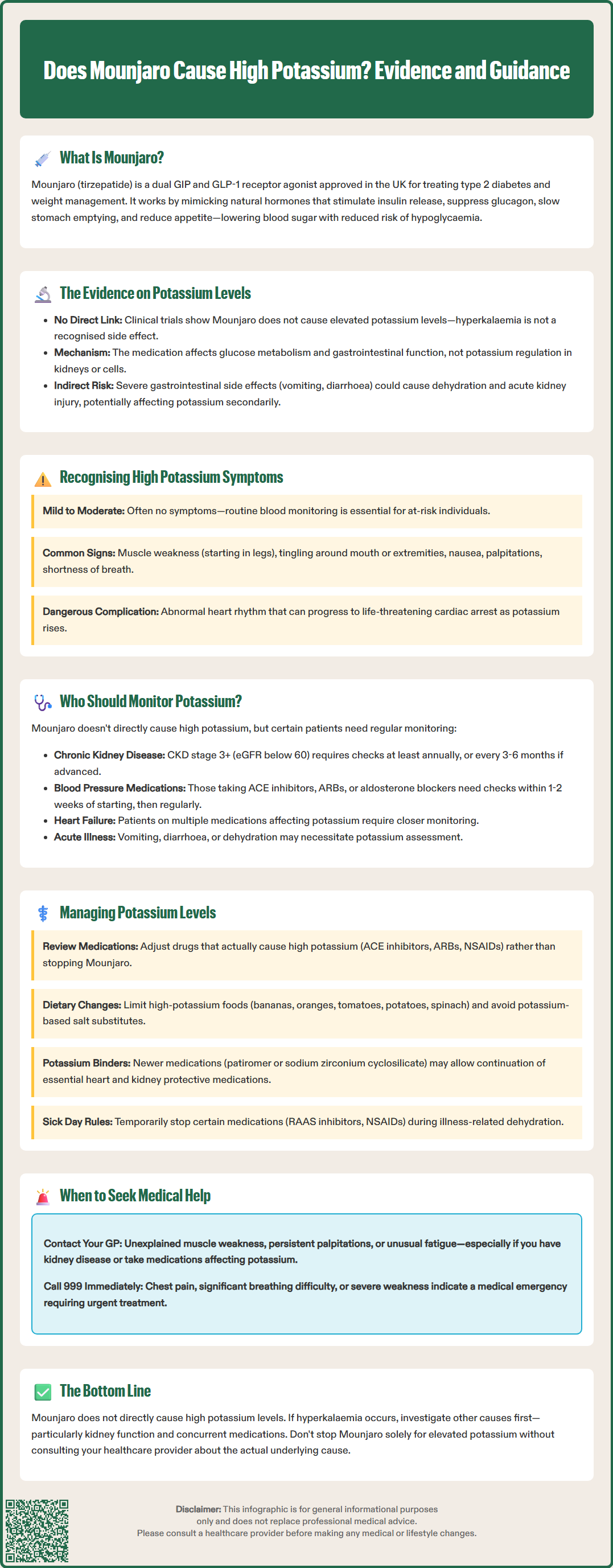
There is no established link between Mounjaro (tirzepatide) and elevated potassium levels (hyperkalaemia) based on current clinical evidence and regulatory guidance. According to the Mounjaro Summary of Product Characteristics (SmPC) and European Medicines Agency (EMA) assessment reports, hyperkalaemia is not listed as a recognised adverse effect of tirzepatide. Clinical trial data have not demonstrated a significant association between the medication and raised serum potassium concentrations.
The pharmacological action of GLP-1 receptor agonists, which forms part of Mounjaro's dual mechanism, primarily affects glucose metabolism, insulin secretion, and gastrointestinal function rather than directly influencing renal potassium handling or cellular potassium distribution. The most commonly reported adverse effects relate to the gastrointestinal system, with nausea, vomiting, and diarrhoea being particularly prevalent, especially during treatment initiation and dose escalation.
However, it is important to note that severe gastrointestinal symptoms can potentially lead to dehydration and acute kidney injury in susceptible patients, which could indirectly contribute to hyperkalaemia. This represents a secondary effect rather than a direct action of the medication itself.
It is also essential to consider the broader clinical context when evaluating potassium levels in patients taking Mounjaro. Individuals with type 2 diabetes often have multiple comorbidities and take several medications that can genuinely affect potassium homeostasis. Medications commonly prescribed alongside diabetes treatments include:
ACE inhibitors or angiotensin receptor blockers (ARBs) for blood pressure control
Potassium-sparing diuretics such as spironolactone or eplerenone
Mineralocorticoid receptor antagonists (MRAs)
Non-steroidal anti-inflammatory drugs (NSAIDs)
Trimethoprim-containing antibiotics
Potassium supplements
Calcineurin inhibitors (e.g., ciclosporin, tacrolimus)
Additionally, chronic kidney disease, which frequently coexists with diabetes, significantly impairs potassium excretion and represents the most important risk factor for hyperkalaemia. Therefore, whilst Mounjaro itself does not cause high potassium, patients taking this medication may develop elevated potassium levels due to other factors in their medical history or concurrent medication regimen.
Hyperkalaemia, defined as a serum potassium concentration above 5.5 mmol/L, can range from mild (5.5-5.9 mmol/L) to moderate (6.0-6.4 mmol/L) or severe (≥6.5 mmol/L). Recognising the symptoms of elevated potassium is crucial because severe hyperkalaemia constitutes a medical emergency requiring immediate intervention. However, many patients with mild to moderate elevations may experience no symptoms at all, which underscores the importance of routine blood monitoring in at-risk individuals.
When symptoms do occur, they typically include:
Muscle weakness or fatigue, often affecting the legs first
Paraesthesia (tingling or numbness), particularly around the mouth or in the extremities
Nausea and vomiting
Palpitations or awareness of irregular heartbeat
Chest discomfort or shortness of breath
The most serious concern with hyperkalaemia relates to its effects on cardiac conduction. Potassium plays a vital role in maintaining the electrical activity of the heart, and elevated levels can cause dangerous arrhythmias. Early ECG changes include tall, peaked T waves and prolongation of the PR interval. As potassium levels rise further, the QRS complex widens, and there is risk of ventricular fibrillation or asystole, both of which can be fatal without immediate treatment.
Patients should be advised to contact their GP promptly if they experience unexplained muscle weakness, persistent palpitations, or unusual fatigue, particularly if they have known risk factors for hyperkalaemia such as chronic kidney disease or are taking medications that affect potassium balance. For moderate hyperkalaemia (≥6.0 mmol/L), urgent same-day assessment is typically required.
In cases of severe symptoms such as chest pain, significant breathing difficulty, or profound weakness, patients should call 999 or go to A&E immediately. For urgent advice, patients can also contact NHS 111. It is worth noting that these symptoms are non-specific and can occur with various medical conditions, so proper clinical assessment, ECG evaluation, and blood testing are essential for accurate diagnosis and management.
Whilst Mounjaro itself does not directly cause hyperkalaemia, certain patient groups require regular potassium monitoring due to underlying conditions or concurrent medications. NICE guidance on chronic kidney disease (NG203), hypertension (NG136), and chronic heart failure (NG106) provides frameworks for identifying patients who need routine electrolyte surveillance.
Patients who should have regular potassium monitoring include those with:
Chronic kidney disease (CKD): Particularly those with an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73m². As renal function declines, the kidneys' ability to excrete potassium diminishes, increasing hyperkalaemia risk. According to NICE NG203, patients with CKD stage 3 or higher should typically have electrolytes checked at least annually, with more frequent monitoring (every 3–6 months) for advanced disease.
Concurrent use of renin-angiotensin-aldosterone system (RAAS) inhibitors: ACE inhibitors, ARBs, and mineralocorticoid receptor antagonists all reduce renal potassium excretion. When initiating or adjusting doses of these medications, potassium should be checked within 1–2 weeks. For MRAs specifically, NICE NG106 recommends checking potassium and renal function at 1 week, monthly for the first 3 months, then every 3-6 months thereafter.
Heart failure: Particularly those on multiple medications affecting potassium balance, including diuretics and RAAS inhibitors.
Acute illness: Patients experiencing significant vomiting, diarrhoea, or dehydration may develop electrolyte disturbances requiring assessment. While gastrointestinal fluid losses often cause hypokalaemia, in patients with CKD, the resulting dehydration and acute kidney injury may paradoxically raise potassium levels.
For patients starting Mounjaro without these risk factors, routine potassium monitoring is not specifically required solely due to the medication itself. However, baseline renal function and electrolytes are typically checked before initiating any diabetes medication as part of comprehensive diabetes care. The frequency of subsequent monitoring should be individualised based on the patient's overall clinical picture, comorbidities, and concurrent medications rather than the use of Mounjaro alone. Healthcare professionals should follow local protocols and NICE guidance when determining appropriate monitoring schedules for their patients.
Effective management of potassium levels in patients taking Mounjaro centres on addressing the actual causes of hyperkalaemia rather than the diabetes medication itself. A comprehensive approach involves medication review, dietary guidance, and appropriate monitoring tailored to individual risk factors.
Medication optimisation represents the first step when hyperkalaemia is detected. Healthcare professionals should review all medications that may contribute to elevated potassium, including RAAS inhibitors, potassium-sparing diuretics, NSAIDs, and potassium supplements. In many cases, dose adjustment or temporary discontinuation of the causative agent may be necessary. However, this must be balanced against the cardiovascular and renal protective benefits of medications such as ACE inhibitors and ARBs, particularly in patients with diabetes and CKD. Newer potassium binders such as patiromer (NICE TA599) or sodium zirconium cyclosilicate (NICE TA623) may allow continuation of essential cardioprotective medications whilst managing potassium levels, though these are typically initiated under specialist advice.
Dietary modification plays an important supportive role. Patients should receive education about potassium-rich foods and may benefit from referral to a dietitian, particularly those with CKD. High-potassium foods include bananas, oranges, tomatoes, potatoes, spinach, and many salt substitutes (which often contain potassium chloride). Patients should be specifically warned to avoid potassium-based salt substitutes. However, dietary restriction should be individualised and not overly restrictive, as many potassium-rich foods provide important nutritional benefits.
Addressing underlying renal function is crucial. Patients with declining kidney function require closer monitoring and may need nephrology referral, particularly if eGFR falls below 30 mL/min/1.73m² or if hyperkalaemia proves difficult to manage. Ensuring adequate hydration and avoiding nephrotoxic medications helps preserve renal function. Patients should be advised about 'sick day rules' – temporarily holding RAAS inhibitors, NSAIDs, and certain other medications during periods of dehydration due to acute illness, and seeking clinical advice.
In cases of acute or severe hyperkalaemia (≥6.5 mmol/L or with ECG changes), urgent management according to UK Kidney Association guidance is required, with immediate review of all medications and appropriate emergency treatment.
Importantly, Mounjaro should not be discontinued solely due to elevated potassium levels unless other causes have been thoroughly investigated and addressed. The medication provides significant benefits for glycaemic control and weight management, and there is no evidence linking it directly to hyperkalaemia. Patients should be reassured that with appropriate monitoring and management of contributing factors, they can safely continue their diabetes treatment whilst maintaining healthy potassium levels.
No, Mounjaro (tirzepatide) does not directly raise potassium levels. Clinical trial data and regulatory guidance do not identify hyperkalaemia as a recognised adverse effect of this medication.
Patients with chronic kidney disease (eGFR below 60 mL/min/1.73m²), those taking ACE inhibitors, ARBs, or potassium-sparing diuretics, and individuals with heart failure require regular potassium monitoring regardless of Mounjaro use.
Mounjaro should not be discontinued solely due to elevated potassium unless other causes have been thoroughly investigated. Healthcare professionals should review concurrent medications and underlying conditions that genuinely affect potassium balance.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.