Does Mounjaro cause low iron? This question concerns many patients prescribed tirzepatide for type 2 diabetes or weight management. Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist that effectively regulates blood glucose and promotes weight loss through appetite suppression and delayed gastric emptying. Whilst iron deficiency is not listed as a direct side effect in UK regulatory guidance, the medication's gastrointestinal effects and impact on dietary intake may indirectly influence nutritional status. Understanding the relationship between Mounjaro and iron levels helps patients recognise when medical assessment is needed and how to maintain adequate nutrition during treatment.
Quick Answer: Mounjaro (tirzepatide) does not directly cause low iron levels according to clinical trial data and UK regulatory assessments.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By mimicking these naturally occurring hormones, Mounjaro helps regulate blood glucose levels, reduces appetite, and slows gastric emptying.
The mechanism of action involves binding to both GIP and GLP-1 receptors, which stimulates insulin secretion when blood glucose is elevated, suppresses glucagon release, and promotes satiety. This dual action makes tirzepatide particularly effective for glycaemic control and weight reduction. Mounjaro is administered once weekly via subcutaneous injection, typically starting at a low dose (2.5 mg) and gradually increasing to minimise side effects.
Common adverse effects reported with Mounjaro predominantly affect the gastrointestinal system. According to the MHRA Summary of Product Characteristics (SmPC), these include:
Nausea (very common, affecting more than 1 in 10 patients)
Diarrhoea and vomiting (very common)
Constipation (common)
Abdominal pain and dyspepsia (common)
Decreased appetite (very common)
Most gastrointestinal side effects are mild to moderate in severity and tend to diminish over time as the body adjusts to treatment. Other reported effects include injection site reactions, fatigue, and hypoglycaemia (particularly when used alongside other glucose-lowering medications such as sulphonylureas or insulin). The SmPC also notes that rodent studies showed thyroid C-cell tumours, though the human relevance of this finding is unknown and not established as a human risk.
Understanding these common side effects helps patients and healthcare professionals distinguish between expected medication responses and potentially concerning symptoms requiring further investigation. If you experience any suspected adverse reactions to Mounjaro, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
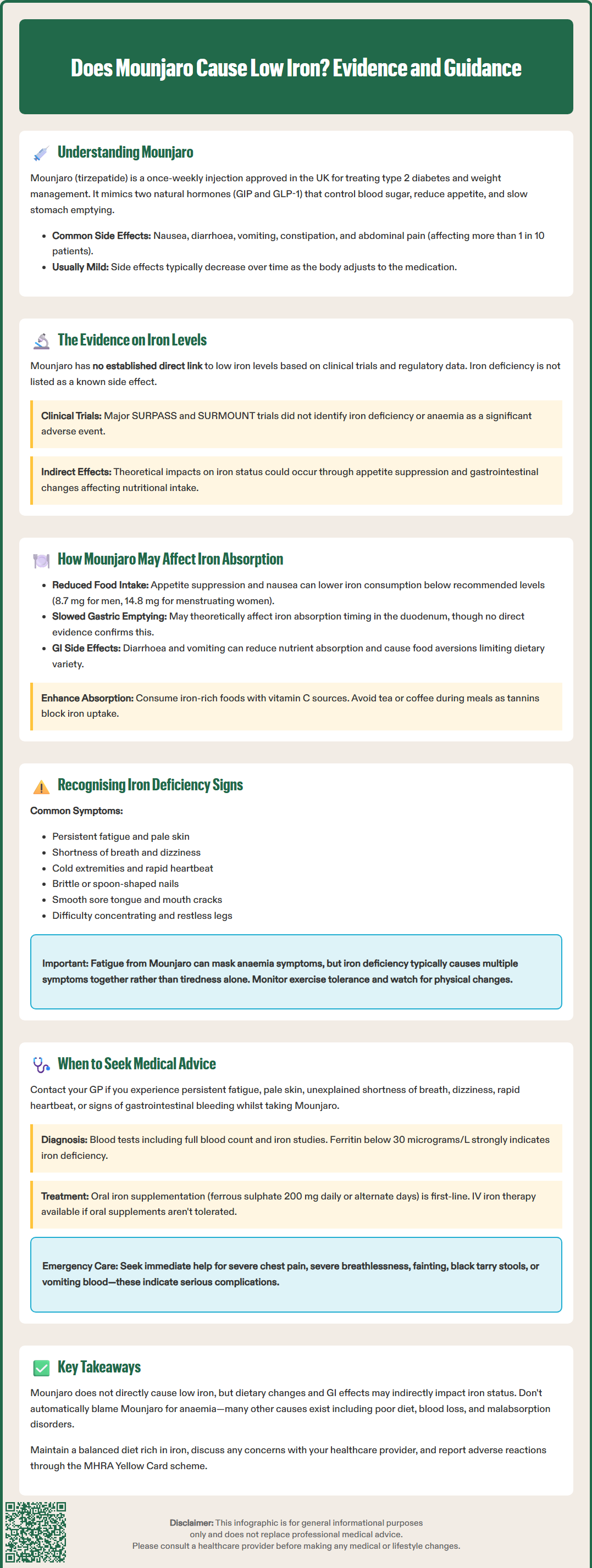
There is currently no established direct link between Mounjaro (tirzepatide) and low iron levels (iron deficiency anaemia) based on clinical trial data and post-marketing surveillance. Iron deficiency is not listed among the known adverse effects in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA) or in prescribing information from the European Medicines Agency (EMA).
The major clinical trials evaluating tirzepatide's safety profile, including the SURPASS programme for diabetes management and the SURMOUNT trials for weight management, did not identify iron deficiency or anaemia as a significant adverse event directly attributable to the medication. No specific signal for iron deficiency has been reported in the regulatory assessments of tirzepatide.
However, it is important to recognise that indirect mechanisms related to Mounjaro's effects on the gastrointestinal system and dietary intake could theoretically influence iron status in certain individuals. The medication's impact on appetite, food intake, and gastrointestinal function may create circumstances where nutritional deficiencies, including iron deficiency, could develop or worsen—though this would be an indirect consequence rather than a direct drug effect.
Patients taking Mounjaro who develop symptoms suggestive of anaemia should not automatically attribute these to the medication itself. Iron deficiency has multiple potential causes, including inadequate dietary intake, chronic blood loss (gastrointestinal or menstrual), malabsorption disorders, and chronic diseases. A thorough clinical assessment is essential to identify the underlying cause. Healthcare professionals should maintain awareness that whilst Mounjaro does not directly cause low iron, the broader context of treatment—including dietary changes and gastrointestinal symptoms—warrants consideration when evaluating a patient's nutritional status.
The gastrointestinal side effects associated with Mounjaro may indirectly influence iron status through several mechanisms. Understanding these potential pathways helps patients and clinicians monitor nutritional health during treatment.
Reduced dietary intake is perhaps the most significant indirect factor. Mounjaro's appetite-suppressing effects and associated nausea can lead to substantially decreased food consumption, which is indeed the primary mechanism behind its weight loss efficacy. However, if patients significantly restrict their diet—particularly foods rich in haem iron (red meat, poultry, fish) and non-haem iron (legumes, fortified cereals, dark leafy vegetables)—they may inadvertently reduce their iron intake below recommended levels. The NHS recommends 8.7 mg of iron daily for adult men and postmenopausal women, and 14.8 mg for women of reproductive age.
Altered gastric emptying is another consideration. GLP-1 receptor agonists slow gastric emptying, which is therapeutic for glucose control but may theoretically affect nutrient absorption. Iron absorption occurs primarily in the duodenum and proximal jejunum, where an acidic environment facilitates the conversion of ferric iron (Fe³⁺) to the more readily absorbed ferrous form (Fe²⁺). While there is no direct evidence that tirzepatide impairs iron absorption, delayed gastric emptying could potentially influence the timing and efficiency of nutrient absorption.
Gastrointestinal symptoms such as diarrhoea and vomiting may contribute to nutrient losses and reduced absorption. Persistent diarrhoea can decrease intestinal transit time, potentially limiting the contact time necessary for optimal iron absorption. Additionally, patients experiencing significant nausea may develop food aversions, further restricting dietary variety and nutritional adequacy.
For patients concerned about maintaining adequate iron levels whilst taking Mounjaro, dietary strategies include consuming iron-rich foods alongside vitamin C sources (which enhance non-haem iron absorption), avoiding excessive tea or coffee with meals (tannins inhibit absorption), and considering iron supplementation if dietary intake proves insufficient—though this should be discussed with a healthcare professional first. The NHS website provides detailed guidance on dietary sources of iron and factors affecting absorption.
Iron deficiency anaemia develops gradually, and early recognition of symptoms enables timely intervention. Patients taking Mounjaro should be aware of the following signs and symptoms:
Common symptoms of iron deficiency include:
Persistent fatigue and weakness that seems disproportionate to activity levels
Pallor (pale skin, conjunctiva, or nail beds)
Shortness of breath, particularly with exertion
Dizziness or lightheadedness
Cold hands and feet
Headaches
Rapid or irregular heartbeat (palpitations)
More specific signs that may develop with established iron deficiency include:
Brittle nails or koilonychia (spoon-shaped nails)
Angular cheilitis (cracks at the corners of the mouth)
Glossitis (sore, smooth tongue)
Restless legs syndrome
Unusual cravings for non-food items (pica), such as ice, clay, or starch
Difficulty concentrating or cognitive impairment
It is important to note that fatigue is also a recognised side effect of Mounjaro itself, particularly during the initial weeks of treatment. This can make it challenging to distinguish between medication-related tiredness and anaemia-related fatigue. However, iron deficiency anaemia typically presents with a constellation of symptoms rather than fatigue alone.
Patients should also be aware that some symptoms—such as dizziness and palpitations—could indicate hypoglycaemia (low blood sugar) rather than anaemia, particularly in those taking Mounjaro alongside other diabetes medications. Monitoring blood glucose levels can help differentiate between these possibilities.
Self-monitoring strategies include paying attention to changes in exercise tolerance, noting any progressive worsening of fatigue despite adequate rest, and observing physical signs such as increased pallor or brittle nails. Keeping a symptom diary can be helpful when discussing concerns with healthcare professionals.
Seek urgent medical attention (call 999) if you experience severe chest pain, severe breathlessness, or fainting. Attend A&E or urgent care if you notice black, tarry stools or vomit blood, as these may indicate gastrointestinal bleeding requiring immediate assessment.
Prompt medical consultation is important if you experience symptoms suggestive of iron deficiency whilst taking Mounjaro. Your GP can arrange appropriate investigations to determine whether low iron is present and identify the underlying cause.
You should contact your GP if you experience:
Persistent or worsening fatigue that interferes with daily activities
Noticeable pallor or comments from others about looking pale
Unexplained shortness of breath or chest discomfort
Persistent dizziness or fainting episodes
Rapid heartbeat or palpitations at rest
Any signs of gastrointestinal bleeding, such as black, tarry stools or blood in vomit
Diagnostic evaluation typically includes a full blood count (FBC) to assess haemoglobin levels, mean corpuscular volume (MCV), and red blood cell indices. If anaemia is confirmed, further tests to evaluate iron status include serum ferritin (a sensitive marker of iron stores), serum iron, total iron-binding capacity (TIBC), and transferrin saturation. According to NICE Clinical Knowledge Summary and British Society of Gastroenterology (BSG) guidelines, serum ferritin below 30 micrograms/L is strongly suggestive of iron deficiency anaemia in adults. However, in the presence of chronic inflammation, iron deficiency may occur with ferritin levels up to 100 micrograms/L, and transferrin saturation below 20% can help support the diagnosis.
Your healthcare provider will also investigate potential causes of iron deficiency, which may include:
Dietary inadequacy (particularly relevant with significant appetite suppression)
Gastrointestinal blood loss (requiring investigation if no obvious cause)
Menstrual blood loss in premenopausal women
Malabsorption disorders such as coeliac disease
Chronic inflammation or other underlying conditions
NICE guidance (NG12) recommends urgent suspected cancer referral (two-week wait) for adults aged 60 and over with iron deficiency anaemia. Additionally, BSG guidelines recommend screening all adults with iron deficiency anaemia for coeliac disease.
Management depends on the severity and cause. Oral iron supplementation (typically ferrous sulphate 200 mg once daily or on alternate days) is first-line treatment for uncomplicated iron deficiency. Current evidence suggests that alternate-day dosing may actually improve absorption and tolerability by reducing hepcidin levels. Iron supplements can cause gastrointestinal side effects (nausea, constipation, dark stools) that may overlap with or exacerbate Mounjaro's gastrointestinal effects. Your doctor may recommend taking iron with food to improve tolerance, though this may reduce absorption.
For patients unable to tolerate or absorb oral iron, or those with ongoing significant losses or malabsorption, intravenous iron therapy may be considered. Regular monitoring of iron levels and haemoglobin is essential to assess treatment response, typically with repeat blood tests after 2-3 months of supplementation. If you have concerns about your iron levels or nutritional status whilst taking Mounjaro, do not hesitate to discuss these with your healthcare team, who can provide personalised advice and appropriate monitoring.
No, there is no established direct link between Mounjaro (tirzepatide) and iron deficiency anaemia based on clinical trials and regulatory data. Iron deficiency is not listed as a known adverse effect in UK prescribing information.
Mounjaro's gastrointestinal effects—including appetite suppression, nausea, and altered gastric emptying—may lead to reduced dietary iron intake or affect absorption. These are indirect mechanisms rather than direct drug effects on iron metabolism.
Contact your GP if you experience persistent fatigue, noticeable pallor, unexplained shortness of breath, dizziness, rapid heartbeat, or signs of gastrointestinal bleeding. Your doctor can arrange blood tests to assess iron status and identify any underlying causes.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.