Does Ozempic affect memory? This question has emerged as semaglutide (Ozempic) becomes increasingly prescribed for type 2 diabetes in the UK. Whilst some patients report subjective cognitive symptoms such as 'brain fog' or difficulty concentrating, there is currently no established causal link between Ozempic and memory impairment. Memory problems are not listed as recognised adverse effects by the MHRA or in the Summary of Product Characteristics. However, ongoing pharmacovigilance continues to monitor for unexpected effects. This article examines the current evidence, explores alternative explanations for cognitive changes during treatment, and provides guidance on when to seek medical advice.
Quick Answer: There is currently no established causal link between Ozempic (semaglutide) and memory impairment based on clinical trial data or UK regulatory assessments.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. Since its introduction, Ozempic has become widely prescribed, and with increased use comes greater scrutiny of its potential side effects.
Concerns about memory and cognitive function have emerged in patient forums and anecdotal reports, prompting questions about whether Ozempic directly affects memory. Currently, there is no established causal link between Ozempic and memory impairment based on clinical trial data or regulatory assessments by the Medicines and Healthcare products Regulatory Agency (MHRA) or the European Medicines Agency (EMA). Memory problems are not listed among the recognised adverse effects in the Summary of Product Characteristics (SmPC) for semaglutide.
However, it is important to acknowledge that post-marketing surveillance continues to monitor for unexpected effects. Some patients have reported subjective experiences of "brain fog" or difficulty concentrating whilst taking GLP-1 receptor agonists, though these reports remain unverified and may be influenced by multiple confounding factors. The absence of evidence is not evidence of absence, and ongoing pharmacovigilance is essential to detect rare or delayed adverse effects that may not have been apparent in pre-licensing trials.
For healthcare professionals and patients alike, understanding the current evidence base is crucial. This article examines reported cognitive concerns, explores alternative explanations for memory changes during treatment, and provides guidance on when to seek medical advice.
If you experience any suspected side effects while taking Ozempic, you can report them via the MHRA Yellow Card scheme.
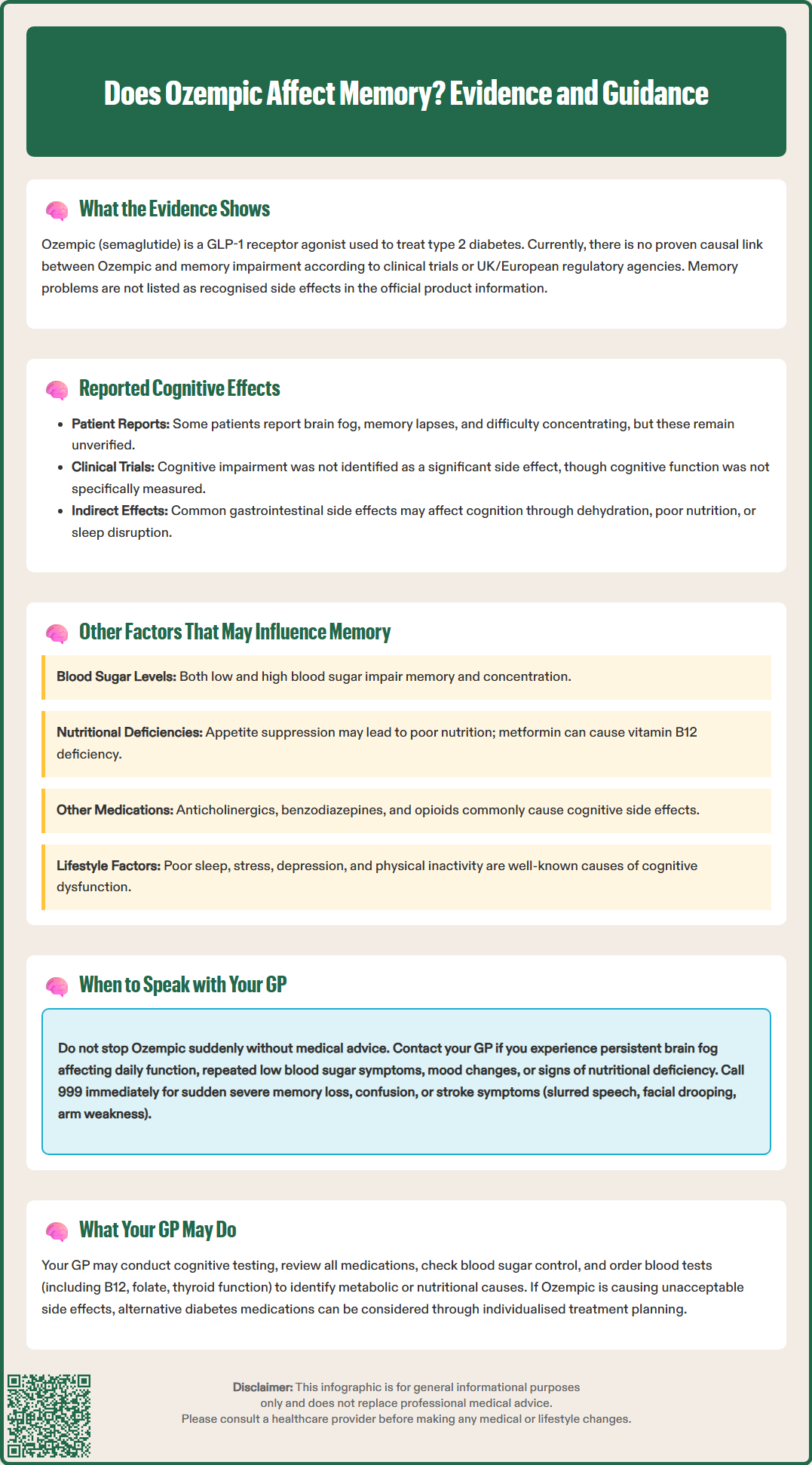
Anecdotal reports from patients taking Ozempic have included descriptions of memory lapses, difficulty concentrating, and a sensation often termed "brain fog". These subjective experiences are not unique to semaglutide and have been reported with other medications, particularly those affecting metabolic or hormonal pathways. It is essential to differentiate between verified adverse drug reactions and coincidental symptoms that may arise during treatment.
In clinical trials of semaglutide for type 2 diabetes, cognitive impairment or memory disturbance were not identified as significant adverse events, although it should be noted that specific cognitive assessments were not a primary focus of these studies. The most commonly reported side effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which occur in a substantial proportion of patients, particularly during dose escalation. These symptoms can be distressing and may indirectly affect cognitive performance through mechanisms such as dehydration, poor nutritional intake, or disrupted sleep.
Some early research has explored potential effects of GLP-1 receptor agonists on neuronal function. Preclinical studies suggest that GLP-1 analogues may influence neuroinflammation and synaptic plasticity, but these findings remain preliminary. Early-phase clinical trials are investigating semaglutide's potential role in neurodegenerative conditions such as Alzheimer's disease and Parkinson's disease, though no cognitive benefits have been established in humans at this stage.
It is important to note that patient-reported cognitive symptoms may reflect a nocebo effect, where negative expectations or heightened awareness of potential side effects lead to the perception of symptoms. Additionally, the psychological burden of managing a chronic condition like diabetes, combined with lifestyle changes and medication adjustments, can contribute to subjective cognitive complaints. Healthcare professionals should take these reports seriously whilst maintaining a balanced, evidence-based perspective.
When evaluating memory concerns in patients taking Ozempic, it is essential to consider alternative explanations that may account for cognitive changes. Type 2 diabetes itself is associated with an increased risk of cognitive impairment and dementia, mediated by mechanisms including chronic hyperglycaemia, vascular damage, and inflammation. Patients may attribute pre-existing or progressive cognitive decline to a newly initiated medication rather than the underlying disease process.
Glycaemic control plays a critical role in cognitive function. Both hypoglycaemia and hyperglycaemia can impair memory and concentration. Ozempic reduces blood glucose levels, and whilst it carries a low intrinsic risk of hypoglycaemia when used as monotherapy, the risk increases significantly when combined with insulin or sulphonylureas, as noted in the SmPC. Even mild, unrecognised hypoglycaemic episodes can cause transient cognitive symptoms, including confusion, difficulty concentrating, and memory lapses. Patients should be educated on recognising hypoglycaemia and advised to monitor blood glucose levels appropriately.
Nutritional factors may also contribute to cognitive symptoms. The appetite-suppressing effects of Ozempic can lead to reduced food intake, and inadequate nutrition may develop if dietary quality is poor. It's worth noting that metformin, commonly prescribed alongside GLP-1 receptor agonists, is associated with vitamin B12 deficiency, which can cause memory impairment and neurological symptoms. Patients on long-term diabetes therapy should have their nutritional status reviewed if they report cognitive concerns.
Certain medications may have cognitive side effects. Medicines with anticholinergic properties, benzodiazepines, sedating antihistamines, and opioids are well-established to affect memory and concentration in some patients. A comprehensive medication review is essential to identify potential drug interactions or cumulative effects. Additionally, lifestyle factors such as poor sleep quality, stress, depression, and lack of physical activity are well-established contributors to cognitive dysfunction and should be addressed as part of holistic patient care.
Patients experiencing memory problems or cognitive changes whilst taking Ozempic should not discontinue the medication abruptly without medical advice, as this may lead to worsening glycaemic control. Instead, it is important to arrange a consultation with your GP or diabetes specialist nurse to discuss your concerns in detail. A thorough clinical assessment can help determine whether the symptoms are related to the medication, the underlying condition, or other factors.
You should contact your GP promptly if you experience:
Persistent "brain fog" that does not improve with time or affects your ability to work or function safely
Symptoms of hypoglycaemia, including shakiness, sweating, palpitations, or difficulty concentrating, especially if recurrent
Mood changes, including low mood, anxiety, or loss of interest in activities, which may indicate depression
Signs of nutritional deficiency, such as fatigue, pallor, tingling in the hands or feet, or glossitis
Call 999 immediately if you experience:
Sudden or severe memory loss that interferes with daily activities
Confusion or disorientation
Slurred speech, facial drooping, arm weakness, or visual disturbances (FAST symptoms of stroke)
If your symptoms are concerning but not an emergency, and you cannot reach your GP, contact NHS 111 for advice.
During your consultation, your GP may perform a cognitive assessment, review your medication regimen, check your blood glucose control, and arrange blood tests to exclude metabolic or nutritional causes of cognitive symptoms. Tests may include full blood count, renal and liver function, thyroid function, vitamin B12, folate, and HbA1c. If necessary, referral to a neurologist or memory clinic may be considered, particularly if there are concerns about underlying neurodegenerative disease.
NICE guidance (NG28) on the management of type 2 diabetes emphasises individualised treatment and regular review of medication efficacy and tolerability. If Ozempic is thought to be contributing to unacceptable side effects, alternative glucose-lowering therapies can be considered. Open communication between patients and healthcare professionals is essential to optimise treatment outcomes whilst maintaining quality of life and cognitive health.
Currently, there is no established causal link between Ozempic and memory impairment based on clinical trial data or regulatory assessments. Memory problems are not listed as recognised adverse effects, though some patients report subjective cognitive symptoms that may have alternative explanations.
Do not stop taking Ozempic without medical advice. Arrange a consultation with your GP or diabetes specialist nurse to discuss your concerns, as they can assess whether symptoms relate to the medication, underlying diabetes, hypoglycaemia, nutritional factors, or other causes.
Yes, type 2 diabetes itself increases cognitive impairment risk, and hypoglycaemia can cause transient memory problems. Nutritional deficiencies (particularly vitamin B12), other medications, poor sleep, stress, and depression may also contribute to cognitive symptoms during treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.