
Does Ozempic affect serotonin? Many patients taking Ozempic (semaglutide) for type 2 diabetes wonder whether this medication influences serotonin levels, particularly if they also take antidepressants. Based on current evidence, Ozempic does not directly alter serotonin production, release, or reuptake in the brain. This GLP-1 receptor agonist works through distinct pathways to improve blood glucose control and does not interact with serotonergic systems in the way psychiatric medications do. However, understanding the relationship between metabolic medications and mood regulation remains important for comprehensive patient care.
Quick Answer: Ozempic does not directly affect serotonin production, release, or reuptake in the brain.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and has been approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and recommended by the National Institute for Health and Care Excellence (NICE) for specific patient groups.
The primary mechanism of action involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. Ozempic works through several pathways:
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it stimulates insulin release only when blood glucose levels are elevated
Suppressing glucagon secretion, which reduces glucose production by the liver
Slowing gastric emptying, which helps control post-meal blood sugar spikes
Reducing appetite through effects on satiety centres in the brain, particularly the hypothalamus
These combined actions help improve glycaemic control in people with type 2 diabetes. Although many patients experience weight loss as a secondary benefit, it is important to note that Ozempic is not licensed for weight management in the UK. A different semaglutide product (Wegovy) is specifically licensed for weight management in eligible patients.
Ozempic does not work in the same way as insulin and carries a lower risk of hypoglycaemia when used alone. However, the risk increases when combined with insulin or sulfonylureas. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, particularly during the initial titration period. These gastrointestinal symptoms typically improve over time as the body adjusts to the medication.
Patients should be aware of important safety warnings, including the risk of acute pancreatitis (seek urgent medical attention for severe, persistent abdominal pain, especially if radiating to the back), gallbladder disease, potential worsening of diabetic retinopathy in patients with pre-existing retinopathy, and risk of dehydration and acute kidney injury with prolonged vomiting or diarrhoea.
According to NICE guidance (NG28), patients on GLP-1 receptor agonists should be reviewed regularly, with continuation based on specific HbA1c reduction and weight loss targets at around 6 months of treatment.
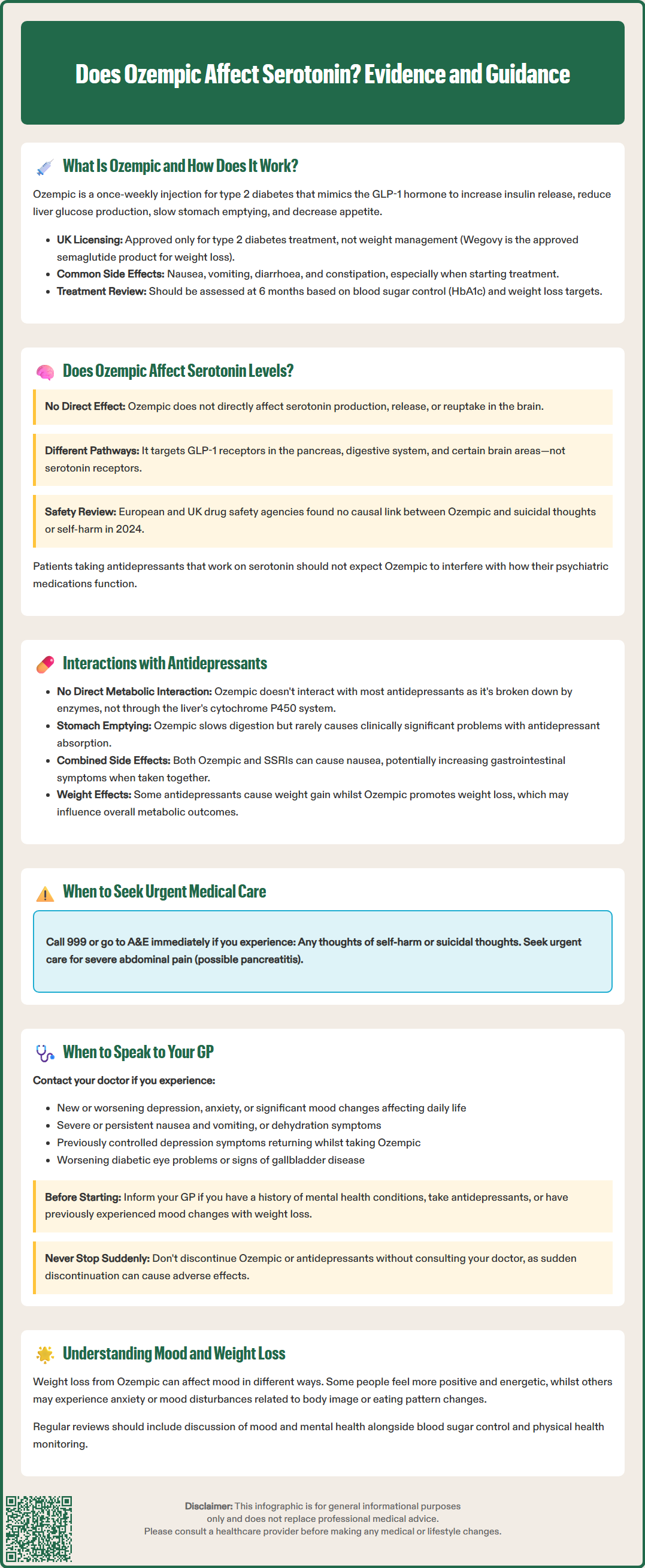
A common question among patients and healthcare professionals is whether Ozempic directly affects serotonin levels or serotonergic pathways in the brain. Based on current evidence, there is no established direct mechanism by which Ozempic alters serotonin production, release, or reuptake in the central nervous system.
Ozempic's primary target is the GLP-1 receptor, which is distinct from serotonin receptors (5-HT receptors). GLP-1 receptors are found throughout the body, including in the pancreas, gastrointestinal tract, and certain brain regions involved in appetite regulation and glucose homeostasis. Whilst GLP-1 receptors are present in the brain, their activation does not directly modulate serotonergic neurotransmission in the way that selective serotonin reuptake inhibitors (SSRIs) or other psychiatric medications do.
However, it is important to recognise that mood, appetite, and metabolic regulation are interconnected through complex neural networks. Some preclinical and emerging research suggests that GLP-1 may have indirect effects on mood and behaviour through potential influence on:
Hypothalamic circuits that regulate both feeding behaviour and emotional responses
Reward pathways in the brain, potentially affecting dopaminergic systems
Inflammatory markers and metabolic health, which may influence mental wellbeing
These potential indirect pathways are still being investigated, and their clinical relevance in humans remains unclear. They do not constitute a direct serotonergic effect. Patients taking antidepressants that work on serotonin systems should not expect Ozempic to interfere with the primary mechanism of their psychiatric medication.
It is also worth noting that in 2024, the European Medicines Agency's Pharmacovigilance Risk Assessment Committee (PRAC) and the MHRA reviewed available evidence and concluded that there is no causal link between GLP-1 receptor agonists like semaglutide and suicidal thoughts or self-harm. Nevertheless, any medication that affects appetite, weight, and metabolic function may have secondary effects on mood and overall mental health, which is why monitoring remains important.
Many patients with type 2 diabetes also take antidepressants for conditions such as depression or anxiety. Understanding potential interactions between Ozempic and these medications is essential for safe prescribing and patient counselling.
Pharmacokinetic interactions (how drugs affect each other's absorption, distribution, metabolism, or elimination) between Ozempic and most antidepressants are generally considered minimal. According to the MHRA/EMC Summary of Product Characteristics (SmPC), Ozempic is a peptide that is degraded by proteolytic enzymes and does not undergo hepatic metabolism via cytochrome P450 enzymes, which are responsible for metabolising many antidepressants. This means direct drug-drug interactions at the metabolic level are unlikely.
However, indirect considerations are important:
Delayed gastric emptying: Ozempic slows the rate at which the stomach empties, which could theoretically affect the absorption of oral medications, including antidepressants. The SmPC notes that injectable semaglutide has not shown clinically relevant effects on the absorption of tested oral medicines, and routine dose adjustments are not required. In practice, this rarely causes clinically significant problems, but patients should be advised to take their antidepressants consistently.
Gastrointestinal side effects: Both Ozempic and certain antidepressants (particularly SSRIs) can cause nausea. When used together, these effects may be additive, potentially affecting medication adherence.
Weight changes: Some antidepressants are associated with weight gain (e.g., mirtazapine, certain tricyclics), whilst Ozempic typically promotes weight loss. These opposing effects may influence overall metabolic outcomes.
Mood and behavioural changes: Whilst there is no pharmacodynamic serotonergic interaction (such as serotonin syndrome) expected between Ozempic and antidepressants, any significant changes in weight, eating patterns, or physical health can affect mood and mental wellbeing.
Patients taking both medications should be monitored regularly by their GP or specialist. If persistent vomiting or poor oral intake occurs, this may affect the effectiveness of oral antidepressants, and patients should seek medical review. It is important to report any new or worsening symptoms, particularly changes in mood, anxiety levels, or the effectiveness of antidepressant therapy.
Whilst Ozempic does not directly affect serotonin systems, patients may experience mood changes for various reasons when starting or taking this medication. It is important to know when to seek medical advice.
Contact your GP or healthcare professional if you experience:
New or worsening depression or anxiety that persists beyond the initial adjustment period (typically the first few weeks)
Significant changes in mood that affect your daily functioning, relationships, or quality of life
Thoughts of self-harm or suicide — this requires urgent medical attention
Severe or persistent nausea and vomiting that prevents you from eating, drinking, or taking other medications
Symptoms of dehydration, such as dizziness, reduced urination, or extreme thirst
Changes in the effectiveness of your antidepressant, such as return of depressive symptoms that were previously well-controlled
For urgent mental health concerns:
If you are in immediate danger or have suicidal intent, call 999 or go to A&E immediately
For urgent advice, call NHS 111
For emotional support, contact Samaritans on 116 123 (available 24/7)
Important warning signs requiring urgent medical attention:
Severe, persistent abdominal pain (especially if radiating to the back) which could indicate pancreatitis
Sudden visual changes, particularly if you have pre-existing diabetic retinopathy
Signs of severe dehydration or reduced kidney function
It is worth noting that weight loss itself can affect mood in complex ways. Some patients feel more positive and energetic as they lose weight and improve their metabolic health, whilst others may experience anxiety or mood disturbances related to changes in body image, eating patterns, or nutritional status.
According to NICE guidance on type 2 diabetes management (NG28), regular review of patients on GLP-1 receptor agonists should include assessment of tolerability, effectiveness, and overall wellbeing. This provides an opportunity to discuss any concerns about mood or mental health.
Before starting Ozempic, inform your GP if you:
Have a history of depression, anxiety, or other mental health conditions
Are currently taking antidepressants or other psychiatric medications
Have previously experienced mood changes with weight loss or dietary changes
Your healthcare team can then provide appropriate monitoring and support, ensuring that both your diabetes management and mental health needs are addressed comprehensively. Never stop taking Ozempic or antidepressants without consulting your doctor, as abrupt discontinuation can lead to adverse effects.
If you suspect you are experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Yes, Ozempic can generally be taken safely with antidepressants as there are minimal pharmacokinetic interactions. However, both medications may cause nausea, and patients should be monitored regularly by their GP for any changes in mood or medication effectiveness.
Ozempic does not interfere with the serotonergic mechanism of SSRIs. The medications work through different pathways, though delayed gastric emptying from Ozempic could theoretically affect oral medication absorption, which is rarely clinically significant.
Yes, you should contact your GP if you experience new or worsening depression, anxiety, significant mood changes affecting daily life, or any thoughts of self-harm. Regular monitoring ensures both diabetes management and mental health needs are addressed comprehensively.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.