Does Ozempic boost metabolism? This is a common question among people considering semaglutide for type 2 diabetes or weight management. Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst it produces significant weight loss and improves glucose control, it does not directly increase basal metabolic rate or thermogenesis. Instead, Ozempic works primarily by suppressing appetite, slowing gastric emptying, and enhancing insulin secretion. Understanding how this medication truly affects your body's energy balance helps set realistic expectations and supports informed treatment decisions.
Quick Answer: Ozempic does not directly boost metabolism or increase basal metabolic rate; it produces weight loss primarily through appetite suppression and improved glucose control.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It mimics the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. By binding to GLP-1 receptors in multiple tissues, Ozempic influences several physiological processes that affect glucose regulation and appetite control.
The primary mechanism of action involves enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications, though this risk increases when combined with insulin or sulfonylureas. Simultaneously, Ozempic suppresses glucagon release from pancreatic alpha cells, thereby reducing hepatic glucose production. These combined effects help maintain more stable blood glucose levels throughout the day.
Crucially, Ozempic also acts on receptors in the brain, particularly in areas that regulate appetite and satiety. This leads to reduced hunger and increased feelings of fullness, which contributes significantly to its weight loss effects. Additionally, the medication slows gastric emptying, meaning food remains in the stomach longer, further promoting satiety and reducing overall caloric intake. This gastric emptying effect is most pronounced early in treatment and may diminish with ongoing therapy.
Whilst Ozempic profoundly affects energy balance and body weight, it does not directly 'boost metabolism' in the traditional sense of increasing basal metabolic rate or thermogenesis. Rather, its effects on weight and energy use are mediated through appetite suppression, improved glucose handling, and subsequent changes in body composition. Any improvements in insulin sensitivity are largely secondary to weight loss and better glycaemic control. Understanding this distinction is important for setting realistic expectations about how the medication works.
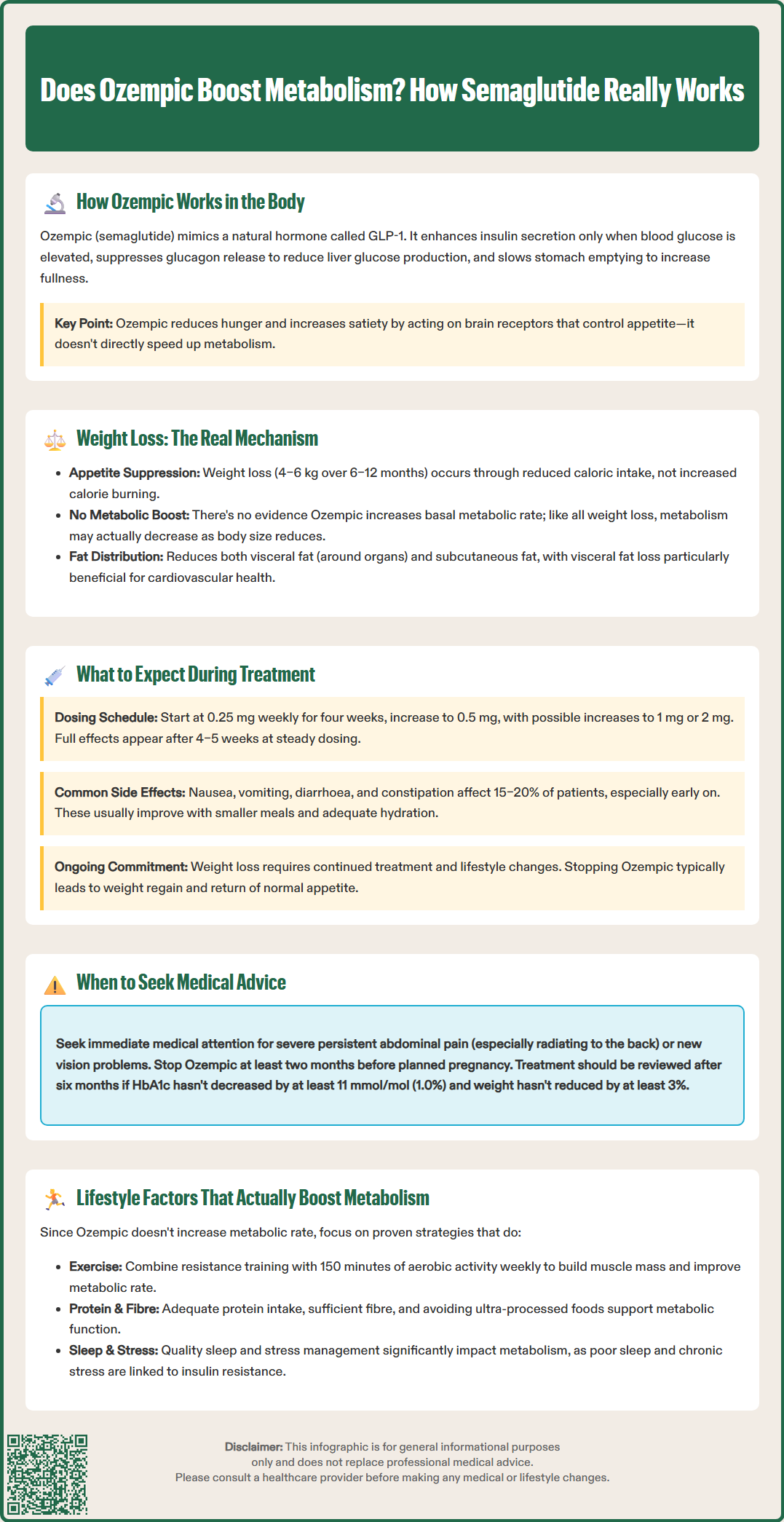
Clinical trials have consistently demonstrated that Ozempic produces significant weight loss in people with type 2 diabetes, with average reductions of 4–6 kg observed over 6–12 months at therapeutic doses. This weight loss occurs primarily through reduced caloric intake rather than through direct metabolic acceleration. The appetite-suppressing effects lead patients to consume fewer calories naturally, creating an energy deficit that results in fat mass reduction.
Regarding metabolic rate specifically, there is no official evidence that Ozempic directly increases basal metabolic rate (BMR) or resting energy expenditure. Research shows that substantial weight loss typically leads to a reduction in metabolic rate, as smaller bodies require less energy to maintain basic functions. Like with other weight loss methods, maintaining adequate protein intake and resistance training can help minimise loss of lean muscle mass during weight reduction.
The medication does influence energy partitioning and substrate utilisation. By improving insulin sensitivity and glucose uptake in peripheral tissues (largely as a consequence of weight loss and improved glycaemic control), Ozempic helps the body use glucose more efficiently. This improved metabolic efficiency, combined with reduced hepatic glucose production, contributes to better overall energy balance and glycaemic control.
Studies show that Ozempic treatment reduces both visceral adipose tissue (fat around internal organs) and subcutaneous fat. Visceral fat reduction is particularly beneficial as this fat type is associated with increased cardiovascular and metabolic risk. Patients should understand that whilst Ozempic facilitates weight loss through appetite regulation, maintaining results requires ongoing treatment and lifestyle modifications. The STEP 4 trial demonstrated that discontinuation typically leads to weight regain and return of appetite to baseline levels.
Ozempic is administered as a once-weekly subcutaneous injection, typically starting at 0.25 mg for the first four weeks as a dose escalation phase (not a maintenance dose), then increasing to 0.5 mg weekly. Some patients may be titrated to 1 mg weekly, and a 2 mg once-weekly dose is also licensed in the UK for patients requiring additional glycaemic control. The medication reaches steady-state concentrations after approximately 4–5 weeks of regular dosing, meaning full therapeutic effects may not be apparent immediately.
Common adverse effects include gastrointestinal symptoms, particularly during dose escalation. Nausea affects approximately 15–20% of patients and is usually most pronounced in the first few weeks of treatment or after dose increases. Other frequent side effects include vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms typically diminish over time as the body adjusts to the medication. Eating smaller, more frequent meals and avoiding high-fat foods may help manage these effects. Maintaining adequate hydration is important, especially if experiencing gastrointestinal side effects, particularly for those with kidney problems.
Important safety considerations include the risk of hypoglycaemia when Ozempic is used with insulin or sulfonylureas (dose reductions of these medications may be needed). Ozempic carries warnings regarding pancreatitis, gallbladder disease, and diabetic retinopathy complications (particularly with rapid improvement in blood glucose control). Contact your GP immediately if you experience severe, persistent abdominal pain, particularly if radiating to the back, as this may indicate pancreatitis. Similarly, report any new or worsening visual symptoms promptly. Ozempic is contraindicated in pregnancy and should be discontinued at least two months before a planned pregnancy. Women of childbearing potential should use effective contraception during treatment.
Monitoring requirements include regular HbA1c measurements to assess glycaemic control, typically every 3–6 months. Weight and blood pressure should be monitored at routine appointments. NICE guidance recommends reviewing the continued need for GLP-1 receptor agonists if HbA1c has not reduced by at least 11 mmol/mol (1.0%) and weight loss of at least 3% of initial body weight has not been achieved within six months of reaching the maximum tolerated dose. Patients should maintain regular contact with their diabetes care team to optimise treatment outcomes and address any concerns promptly. Suspected side effects can be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
For individuals seeking metabolic improvements, lifestyle modifications remain the cornerstone of effective management. Regular physical activity, particularly resistance training combined with aerobic exercise, can increase muscle mass and improve metabolic rate more directly than any medication. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly for adults, alongside muscle-strengthening activities on two or more days per week.
Dietary approaches that support metabolic health include adequate protein intake (which has a higher thermic effect than carbohydrates or fats), sufficient fibre consumption, and avoiding ultra-processed foods. Whilst no specific diet universally 'boosts metabolism', maintaining regular meal patterns and avoiding prolonged caloric restriction can help prevent metabolic adaptation. Sleep quality and stress management also significantly influence metabolic function, with poor sleep and chronic stress associated with insulin resistance and weight gain.
Alternative medications for type 2 diabetes include other GLP-1 receptor agonists such as dulaglutide (Trulicity) and liraglutide (Victoza), which work through similar mechanisms. According to NICE guidance (NG28), metformin remains the first-line pharmacological treatment for many people with type 2 diabetes in the UK, though SGLT2 inhibitors may be considered first-line in those with established cardiovascular disease, chronic kidney disease, or at high cardiovascular risk. SGLT2 inhibitors (such as dapagliflozin or empagliflozin) offer cardiovascular and renal benefits alongside glucose-lowering effects and typically produce modest weight loss through urinary glucose excretion.
For weight management specifically, higher-dose semaglutide (Wegovy, 2.4 mg weekly) is licensed for obesity treatment in the UK. NICE (TA875) recommends its use within specialist weight management services for people with a BMI of at least 35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) and at least one weight-related condition. Orlistat, which reduces dietary fat absorption, represents a non-systemic alternative available through the NHS for eligible patients. However, all pharmacological approaches work best when combined with comprehensive lifestyle interventions. Patients should discuss with their healthcare team which treatment approach best suits their individual circumstances, comorbidities, and treatment goals, recognising that sustainable metabolic health requires a multifaceted, long-term commitment rather than reliance on any single intervention.
No, Ozempic does not directly increase basal metabolic rate or resting energy expenditure. It produces weight loss primarily through appetite suppression and reduced caloric intake, not by accelerating metabolism.
Ozempic reaches steady-state concentrations after approximately 4–5 weeks of regular dosing. Full therapeutic effects on glucose control and appetite may not be apparent immediately, particularly during the initial dose escalation phase.
Clinical trials show that discontinuing Ozempic typically leads to weight regain and return of appetite to baseline levels. Maintaining results requires ongoing treatment combined with sustained lifestyle modifications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.