Ozempic (semaglutide) is a once-weekly injectable GLP-1 receptor agonist licensed in the UK for managing type 2 diabetes mellitus in adults. Many patients wonder how fast does Ozempic work when starting treatment. Whilst some early improvements in blood glucose may be noticed within the first week, the medication reaches steady-state concentrations after approximately 4 to 5 weeks of consistent dosing. Full therapeutic benefits—including measurable HbA1c reductions and potential weight loss—typically develop over 12 to 16 weeks. Understanding this timeline helps set realistic expectations and supports adherence to treatment under healthcare professional supervision.
Quick Answer: Ozempic begins affecting blood glucose within the first week, but reaches steady-state concentrations after 4 to 5 weeks, with full therapeutic benefits typically evident after 12 to 16 weeks of consistent use.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is indicated as monotherapy when metformin is not tolerated or contraindicated, or as add-on therapy with other glucose-lowering medicines. It belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and is typically used alongside diet and exercise to improve glycaemic control.
The mechanism of action of Ozempic centres on mimicking the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation. When administered, semaglutide binds to GLP-1 receptors in the pancreas, stimulating insulin secretion in a glucose-dependent manner. This means insulin is released only when blood glucose levels are elevated, reducing the risk of hypoglycaemia compared to some other diabetes medications.
Additionally, Ozempic suppresses glucagon secretion, a hormone that raises blood glucose levels, and slows gastric emptying, which helps moderate the rise in blood sugar after meals. It also acts on the brain to reduce appetite. These combined effects contribute to improved HbA1c levels and better overall glucose control. Many patients also experience weight loss, which occurs as a secondary effect due to reduced appetite and delayed gastric emptying.
It is important to note that Ozempic is not insulin and is not indicated for type 1 diabetes or diabetic ketoacidosis. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic specifically for type 2 diabetes management, and it should only be used under the supervision of a healthcare professional. Patients should be aware that while weight loss may occur, Ozempic is not licensed in the UK as a standalone weight management treatment—this indication applies to a higher-dose formulation called Wegovy.
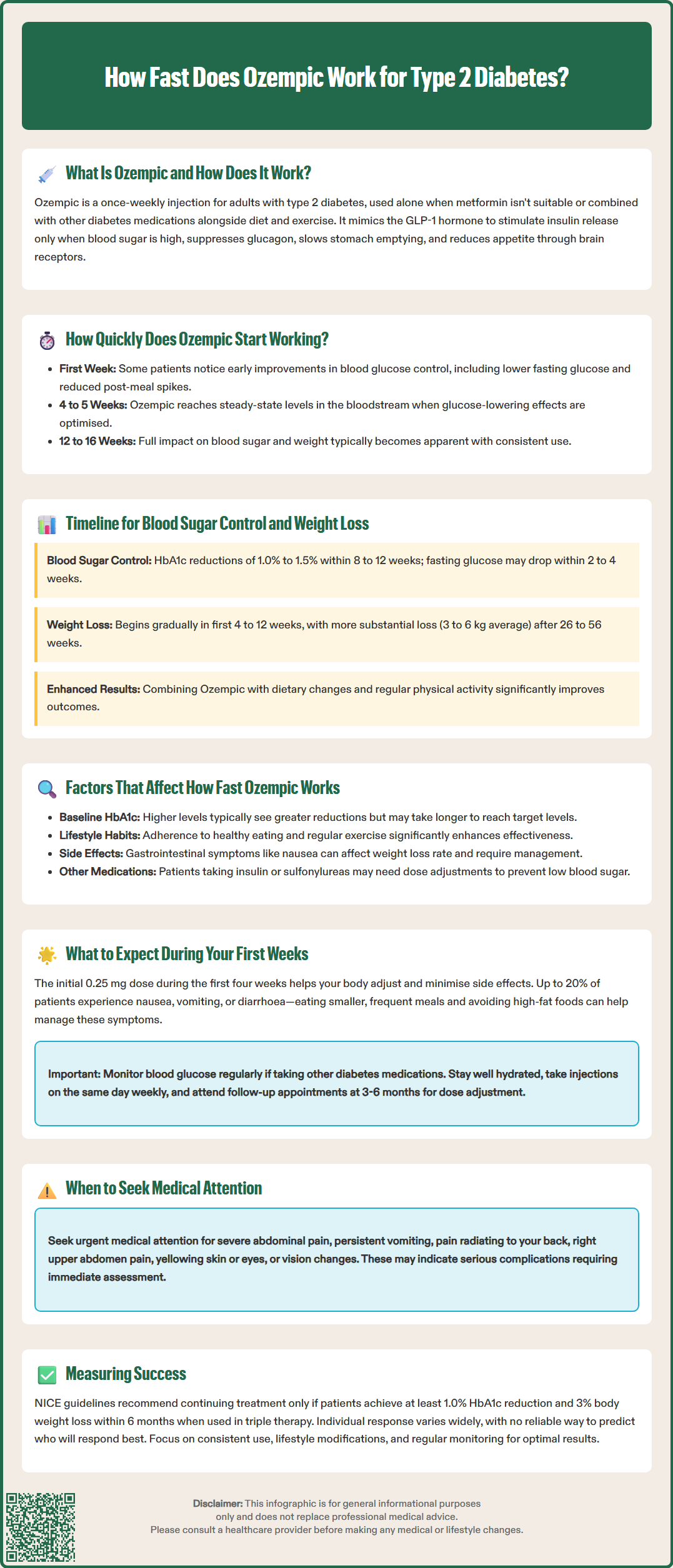
Ozempic begins to exert its pharmacological effects relatively quickly after the first injection, though the full therapeutic benefit develops gradually over several weeks. From a pharmacokinetic perspective, semaglutide has a half-life of approximately one week and reaches steady-state concentrations in the bloodstream after approximately 4 to 5 weeks of once-weekly dosing. This means the medication accumulates to consistent levels that optimise its glucose-lowering effects.
However, patients may notice some early improvements in blood glucose control within the first week of treatment. This initial response occurs because Ozempic starts influencing insulin and glucagon secretion soon after administration. Many individuals observe lower fasting blood glucose readings and reduced post-meal glucose spikes during the first few days, though these changes may be modest initially.
According to the UK Summary of Product Characteristics (SmPC), Ozempic is initiated at a low dose (0.25 mg once weekly) for the first four weeks. This starting dose is primarily intended to improve gastrointestinal tolerability rather than to achieve maximum glycaemic control. After this initial period, the dose is typically increased to 0.5 mg weekly, with the option to escalate to 1 mg weekly after at least 4 weeks if additional glucose control is needed. For patients requiring further glycaemic control, the maintenance dose may be increased to 2 mg once weekly after at least 4 weeks on the 1 mg dose.
If a dose is missed, it should be administered as soon as possible within 5 days after the missed dose. If more than 5 days have passed, the missed dose should be skipped, and the next dose administered on the regularly scheduled day.
It is essential for patients to understand that the timeline for experiencing benefits varies between individuals. Factors such as baseline HbA1c, body weight, diet, physical activity, and concurrent medications all influence how quickly Ozempic produces noticeable effects. Patience and adherence to the prescribed regimen are crucial, as the medication's full impact on both blood sugar and weight typically becomes apparent over 12 to 16 weeks of consistent use.
The timeline for achieving blood sugar control and weight loss with Ozempic follows a generally consistent pattern, though individual responses vary considerably. For glycaemic control, measurable improvements in HbA1c—a marker reflecting average blood glucose over the preceding 2 to 3 months—are typically observed after 8 to 12 weeks of treatment. In pivotal trials, patients achieved HbA1c reductions of approximately 1.0% to 1.5% (11-16 mmol/mol) from baseline when using the 0.5 mg or 1 mg weekly doses.
Fasting plasma glucose levels often improve more rapidly, with many patients noticing lower morning readings within 2 to 4 weeks. Post-prandial (after-meal) glucose control also improves progressively as the medication reaches steady-state levels. Healthcare professionals typically assess treatment response through blood tests at 3-month intervals, allowing sufficient time for Ozempic to demonstrate its effect on HbA1c.
Weight loss, while not the primary indication for Ozempic in diabetes management, occurs as a beneficial secondary outcome for many patients. Clinical studies show that weight reduction begins gradually, with most patients experiencing modest weight loss in the first 4 to 12 weeks. More substantial weight loss—typically ranging from 3 to 6 kg on average—becomes evident after approximately 26 to 56 weeks of treatment, though individual results vary considerably.
The weight loss effect is thought to result from reduced appetite, increased satiety, and delayed gastric emptying. Patients often report feeling fuller for longer periods and experiencing fewer cravings. It is important to emphasise that weight loss outcomes are enhanced when Ozempic is combined with dietary modifications and regular physical activity, as recommended in NICE guidance for type 2 diabetes management. Not all patients will experience significant weight loss, and this should not be considered a treatment failure if glycaemic control improves.
According to NICE guideline NG28, when GLP-1 receptor agonists like Ozempic are used in triple therapy regimens, treatment should only continue if there is a beneficial metabolic response (a reduction of at least 11 mmol/mol [1.0%] in HbA1c and weight loss of at least 3% of initial body weight in 6 months).
Several patient-specific and clinical factors influence the speed and extent of Ozempic's therapeutic effects. Understanding these variables helps set realistic expectations and optimise treatment outcomes.
Baseline HbA1c and disease duration: Patients with higher initial HbA1c levels often experience more pronounced reductions, though it may take longer to reach target levels. Those with longstanding type 2 diabetes or significant beta-cell dysfunction may respond more slowly than newly diagnosed individuals. Importantly, rapid improvements in HbA1c can sometimes temporarily worsen diabetic retinopathy in patients with pre-existing eye disease; any new or worsening visual symptoms should be reported promptly to a healthcare professional.
Body weight and composition: Higher body weight may influence the pharmacokinetics of semaglutide, though the once-weekly dosing is designed to accommodate a range of body sizes. Patients with obesity may experience different weight loss trajectories compared to those with lower BMI.
Adherence to lifestyle modifications: Diet and exercise significantly impact how quickly Ozempic produces results. Patients who implement healthy eating patterns with appropriate carbohydrate intake (as advised by NHS or Diabetes UK guidance) and engage in regular physical activity typically achieve better glycaemic control and more substantial weight loss. Conversely, poor dietary habits may limit the medication's effectiveness.
Concurrent medications: Other diabetes medications, particularly insulin or sulfonylureas, may interact with Ozempic's effects. Dose adjustments of these agents may be necessary to prevent hypoglycaemia and optimise overall glucose control.
Gastrointestinal tolerability: Nausea, vomiting, or diarrhoea—common side effects, particularly during dose escalation—may affect dietary intake and, consequently, the rate of weight loss. These symptoms can also lead to dehydration and potential acute kidney injury, especially in older people or those with existing renal impairment. Patients experiencing significant gastrointestinal symptoms should stay well-hydrated and discuss management strategies with their healthcare provider.
Individual variability: Response to GLP-1 receptor agonists varies widely between individuals. While there are no validated pharmacogenetic markers to predict response to semaglutide, clinical observation confirms considerable differences in both efficacy and side effect profiles among patients.
Starting Ozempic requires preparation and realistic expectations to ensure safe and effective treatment. During the first four weeks, patients receive the 0.25 mg starter dose, which is primarily intended to help the body adjust to the medication and minimise gastrointestinal side effects.
Common early experiences include:
Nausea, vomiting and diarrhoea: These are common side effects, with nausea affecting up to 20% of patients. They are typically mild-to-moderate and often improve with time. Nausea usually occurs within hours of injection and often diminishes over several days. Eating smaller, more frequent meals and avoiding high-fat foods may help.
Reduced appetite: Many patients notice decreased hunger and earlier satiety during meals. This effect usually becomes more pronounced as treatment continues.
Injection site reactions: Mild redness, itching, or discomfort at the injection site may occur but typically resolves quickly. Rotating injection sites is recommended.
Modest blood glucose improvements: While dramatic changes are uncommon in the first week, many patients observe gradual reductions in fasting and post-meal glucose levels.
Practical advice for the initial period:
Monitor blood glucose regularly if advised by your healthcare team, particularly if taking other diabetes medications that may cause hypoglycaemia (such as insulin or sulfonylureas). Discuss potential dose adjustments of these medications with your healthcare provider.
Stay well hydrated, especially if experiencing nausea, vomiting or diarrhoea. Be alert for signs of dehydration (excessive thirst, dark urine, dizziness), particularly if you have kidney problems or are taking medications like diuretics.
Report concerning symptoms to your GP or diabetes specialist nurse. Severe or persistent abdominal pain, persistent vomiting, signs of pancreatitis (severe upper abdominal pain radiating to the back), gallbladder problems (pain in the right upper abdomen, yellowing of skin/eyes), or changes in vision require urgent medical attention.
Administer on the same day each week. If you miss a dose, take it as soon as possible within 5 days. If more than 5 days have passed, skip the missed dose and take your next dose on the regularly scheduled day.
Attend follow-up appointments as scheduled, typically at 3-6 months, to assess HbA1c response and determine whether dose escalation is appropriate.
Use effective contraception if you are a woman of childbearing potential. Ozempic is not recommended during pregnancy and should be discontinued at least 2 months before a planned pregnancy.
Patients should understand that the first weeks represent an adjustment phase. The full benefits of Ozempic—both for glucose control and potential weight loss—develop gradually, and consistency with weekly injections is essential for optimal outcomes.
If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Some patients notice early improvements in blood glucose within the first week, though full therapeutic benefits develop over 12 to 16 weeks. Measurable HbA1c reductions are typically observed after 8 to 12 weeks of consistent treatment.
The initial 0.25 mg dose for the first 4 weeks is primarily intended to improve gastrointestinal tolerability and help your body adjust to the medication, rather than to achieve maximum glycaemic control.
Common side effects like nausea often improve with time and can be managed by eating smaller meals and staying hydrated. However, severe abdominal pain, persistent vomiting, visual changes, or signs of dehydration require urgent medical attention.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.