
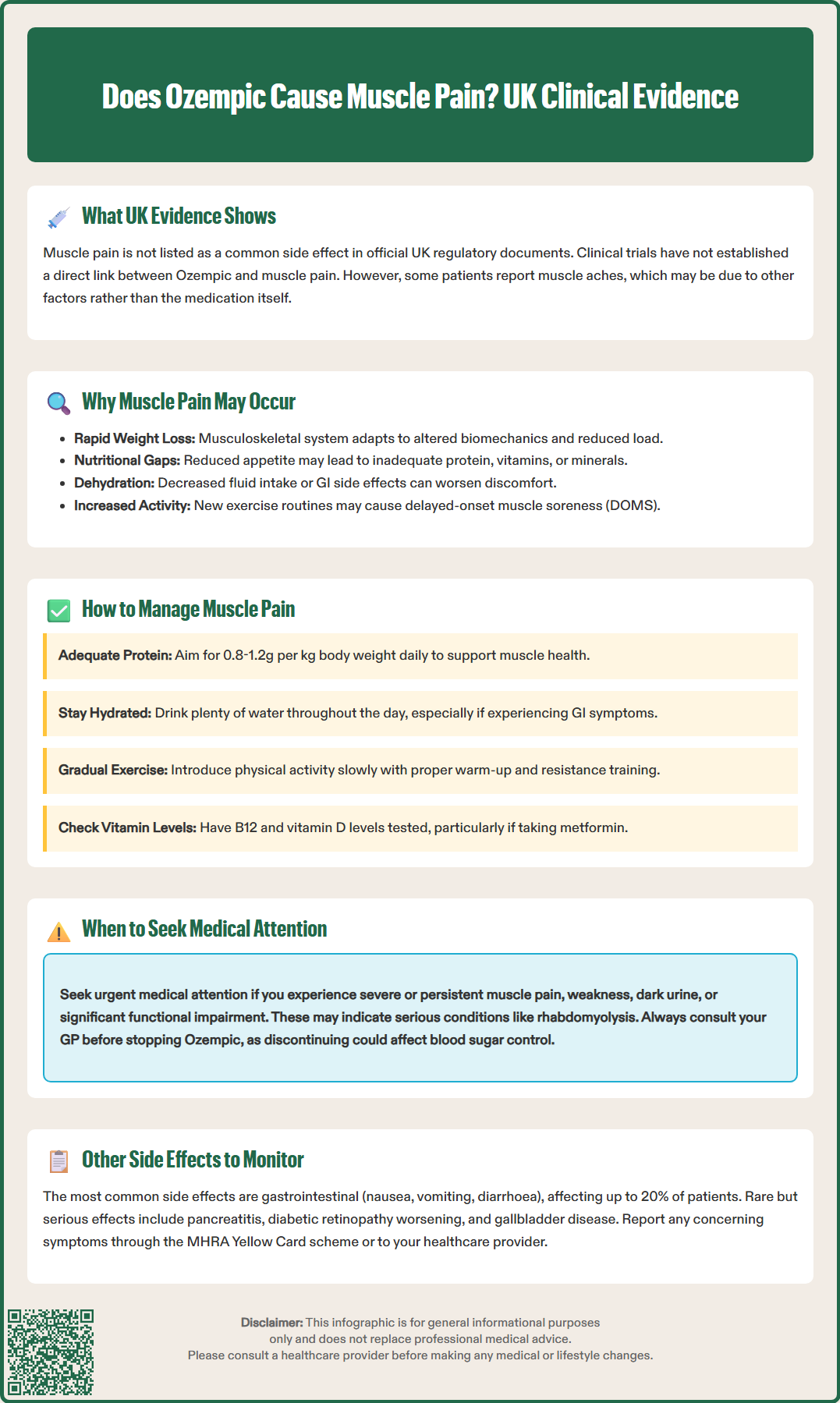
Does Ozempic cause muscle pain? Whilst muscle pain is not listed amongst the common adverse effects of Ozempic (semaglutide) in UK regulatory documentation, some patients do report musculoskeletal discomfort during treatment. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for type 2 diabetes mellitus management. Clinical trial data have not established a direct causal link between semaglutide and muscle pain, though symptoms may relate to rapid weight loss, changes in body composition, nutritional factors, or increased physical activity. If you experience persistent or severe muscle pain whilst taking Ozempic, consult your GP or diabetes specialist for proper assessment and guidance.
Quick Answer: Ozempic (semaglutide) is not directly linked to muscle pain in clinical trials, though some patients report musculoskeletal discomfort potentially related to weight loss, body composition changes, or increased activity.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A higher dose formulation of semaglutide (Wegovy) is licensed for weight management, but Ozempic itself is not approved for this purpose. Whilst muscle pain is not listed amongst the common adverse effects in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), some patients do report musculoskeletal discomfort during treatment.
According to the European Medicines Agency's European Public Assessment Report (EPAR) for Ozempic, clinical trial data and post-marketing surveillance have not established a direct causal link between semaglutide and muscle pain. Some individuals may experience muscle aches or joint discomfort whilst taking Ozempic, but these symptoms may be related to other factors, such as increased physical activity following weight loss, changes in body composition, or concurrent medical conditions.
The National Institute for Health and Care Excellence (NICE) guidelines for type 2 diabetes management (NG28) recommend monitoring for adverse effects when initiating GLP-1 receptor agonists. If you are experiencing persistent or severe muscle pain whilst taking Ozempic, it is essential to discuss this with your GP or diabetes specialist. They can assess whether the symptoms are related to the medication, require investigation for alternative causes, or necessitate a change in treatment strategy. Never discontinue prescribed medication without medical advice, as this may compromise glycaemic control.
Understanding the potential mechanisms behind muscle pain in patients taking Ozempic requires consideration of both the drug's pharmacological effects and the physiological changes that accompany its use. Semaglutide works by mimicking the action of endogenous GLP-1, enhancing glucose-dependent insulin secretion, suppressing glucagon release, and slowing gastric emptying. These effects contribute to improved glycaemic control and often significant weight loss.
One plausible explanation for musculoskeletal discomfort relates to rapid weight loss and changes in body composition. As patients lose weight—sometimes substantially—the musculoskeletal system must adapt to altered biomechanics and reduced load-bearing. This adjustment period may manifest as muscle aches, joint discomfort, or generalised fatigue. Data from the STEP and SUSTAIN clinical trial programmes have shown that weight loss with semaglutide includes some reduction in lean body mass alongside fat mass, which could potentially contribute to muscle symptoms.
Another consideration is nutritional status. GLP-1 receptor agonists reduce appetite and caloric intake, which may inadvertently lead to reduced protein, vitamin, or mineral consumption. Inadequate intake of certain nutrients may contribute to muscle symptoms, particularly in those already taking medications like metformin, which can affect vitamin B12 levels. Dehydration—which may occur due to reduced fluid intake or gastrointestinal side effects—can also exacerbate musculoskeletal symptoms.
It is also worth noting that increased physical activity following weight loss and improved energy levels may lead to delayed-onset muscle soreness (DOMS), particularly in individuals who were previously sedentary. This is a normal physiological response to unaccustomed exercise rather than a direct drug effect.
If you are experiencing muscle pain whilst taking Ozempic, several practical strategies may help alleviate symptoms whilst maintaining the therapeutic benefits of the medication. First and foremost, consult your healthcare provider to rule out other potential causes of muscle pain, such as statin-induced myopathy (if you are taking cholesterol-lowering medication), vitamin D deficiency, thyroid dysfunction, or inflammatory conditions.
Optimising nutrition is important. Ensure adequate protein intake (generally 0.8-1.2 g per kilogram of body weight daily, though this should be individualised, particularly if you have kidney disease). A registered dietitian can provide personalised guidance. Your GP may consider checking vitamin B12 levels, particularly if you also take metformin, and other tests based on your specific symptoms and clinical assessment.
Gradual introduction of physical activity is advisable. If you have recently increased your exercise levels, ensure you incorporate adequate warm-up and cool-down periods, and consider working with a physiotherapist or exercise specialist to develop a balanced programme that includes both cardiovascular and resistance training. This approach helps preserve muscle mass and reduces the risk of injury.
Hydration is often overlooked but essential. Aim for adequate fluid intake throughout the day, particularly if you are experiencing gastrointestinal side effects such as nausea or diarrhoea. Dehydration can exacerbate muscle cramping and discomfort.
Simple self-care measures may provide relief:
Gentle stretching exercises, particularly before bed
Warm baths or heat application to affected muscles
Paracetamol may help relieve pain (follow package instructions and do not exceed recommended doses)
Adequate rest and sleep to support muscle recovery
Non-steroidal anti-inflammatory drugs (NSAIDs) should be used with caution, particularly if you are dehydrated or have kidney problems.
If muscle pain is severe, persistent, or accompanied by weakness, dark urine, or significant functional impairment, seek urgent medical attention via NHS 111, your GP, or A&E as appropriate. These symptoms may indicate rhabdomyolysis or another serious condition requiring immediate investigation.
Whilst muscle pain is not amongst the most commonly reported adverse effects, Ozempic is associated with a well-characterised side effect profile that patients and healthcare professionals should be aware of. According to the MHRA-approved SmPC, gastrointestinal symptoms are the most frequently reported adverse effects, occurring in a significant proportion of patients, particularly during dose escalation. These include:
Nausea (affecting up to 20% of patients)
Vomiting
Diarrhoea
Constipation
Abdominal pain or discomfort
These symptoms are typically mild to moderate in severity and often improve over time as the body adjusts to the medication. Small, frequent meals, avoiding high-fat or spicy foods, and staying well-hydrated may help mitigate gastrointestinal discomfort.
Hypoglycaemia (low blood glucose) is uncommon when Ozempic is used as monotherapy, as its glucose-lowering effect is glucose-dependent. However, the risk increases when combined with insulin or sulfonylureas. NICE guidance (NG28) recommends considering a reduction in insulin or sulfonylurea doses when initiating or uptitrating GLP-1 receptor agonists. Patients should be educated about recognising hypoglycaemia symptoms (tremor, sweating, confusion, palpitations) and appropriate management strategies.
Injection site reactions—including redness, itching, or swelling—may occur but are generally mild and transient. Rotating injection sites (abdomen, thigh, or upper arm) can help minimise these reactions.
More serious but rare adverse effects include:
Pancreatitis: Seek immediate medical attention if you experience severe, persistent abdominal pain radiating to the back, particularly if accompanied by vomiting
Diabetic retinopathy complications: The SmPC notes that rapid improvement in glucose control has been associated with temporary worsening of diabetic retinopathy, particularly in patients with pre-existing retinopathy and those on insulin
Acute kidney injury: Particularly in the context of severe dehydration from gastrointestinal side effects
Gallbladder disease: Rapid weight loss may increase the risk of gallstones
Thyroid considerations: Semaglutide has been associated with thyroid C-cell tumours in rodent studies, though the relevance to humans remains uncertain. The UK SmPC advises discussing any thyroid symptoms with your healthcare provider.
If you experience any concerning symptoms whilst taking Ozempic, contact your GP or diabetes specialist team promptly. Suspected side effects can be reported via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or by searching 'MHRA Yellow Card' in the Google Play or Apple App Store.
Muscle pain is not listed amongst the common adverse effects in the UK Summary of Product Characteristics for Ozempic. Clinical trials have not established a direct causal link between semaglutide and muscle pain, though some patients report musculoskeletal discomfort.
Consult your GP or diabetes specialist to assess whether symptoms are medication-related or require investigation for alternative causes. Never discontinue prescribed medication without medical advice, as this may compromise glycaemic control.
Seek urgent medical attention via NHS 111, your GP, or A&E if muscle pain is severe, persistent, or accompanied by weakness, dark urine, or significant functional impairment, as these may indicate serious conditions like rhabdomyolysis.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.