Does Ozempic give you a yeast infection? This is a common concern amongst patients prescribed semaglutide for type 2 diabetes. Whilst Ozempic (semaglutide) is not directly linked to yeast infections in official UK guidance, people with diabetes face inherently higher infection risks due to elevated blood glucose levels. Understanding the relationship between diabetes medications, glycaemic control, and candidal infections is essential for effective management. This article examines the evidence, clarifies misconceptions, and provides practical guidance on reducing infection risk whilst taking Ozempic.
Quick Answer: Ozempic (semaglutide) does not directly cause yeast infections and is not listed as causing thrush in UK prescribing information.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
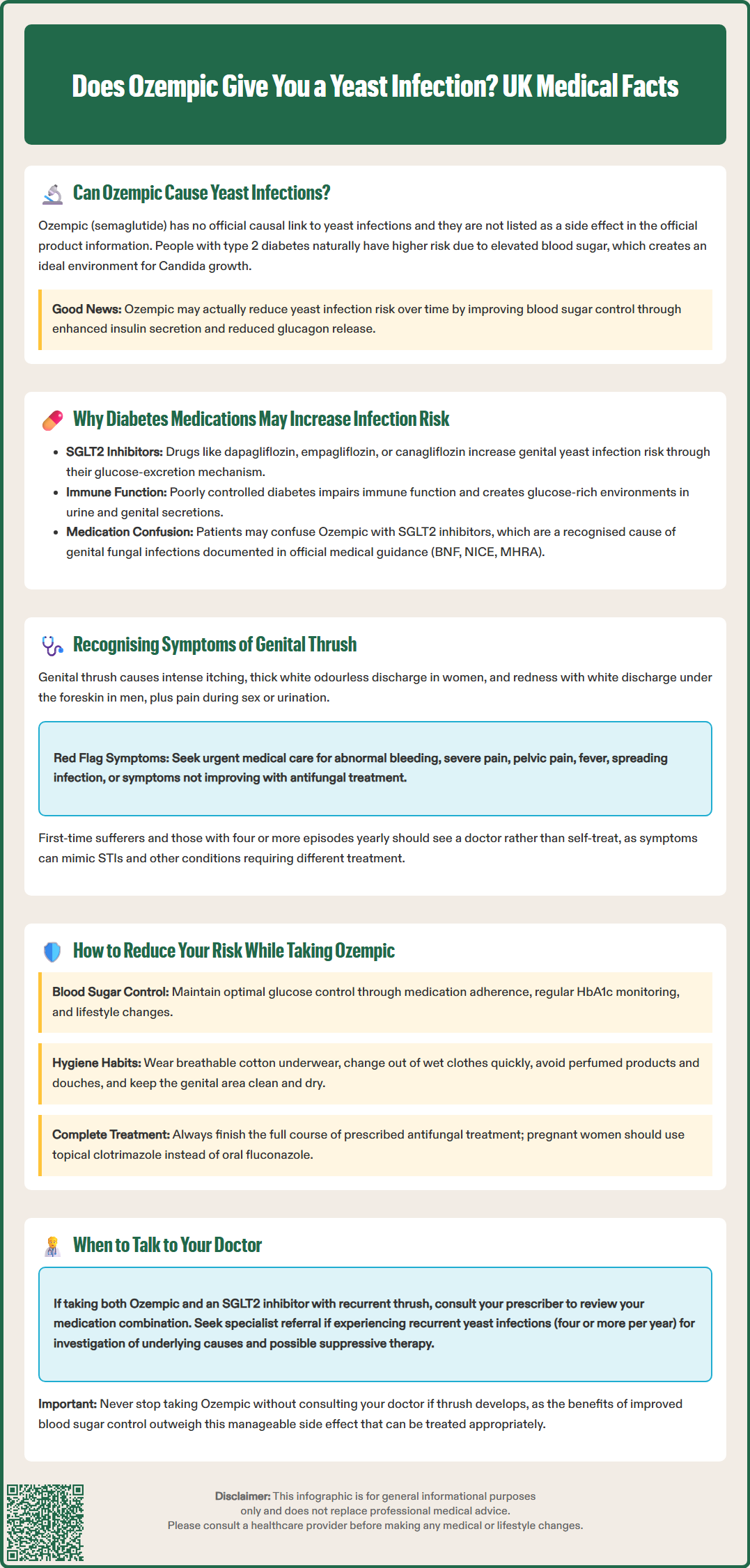
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst yeast infections—particularly genital thrush (vulvovaginal candidiasis in women and balanitis in men)—are not listed as an adverse effect of Ozempic in the Summary of Product Characteristics (SmPC), there is no official causal link established between semaglutide and increased yeast infection rates.
Patients with type 2 diabetes are inherently at higher risk of developing candidal infections due to elevated blood glucose levels, which create a favourable environment for Candida albicans growth. Because Ozempic improves glycaemic control by enhancing insulin secretion and reducing glucagon release, it may indirectly reduce infection risk over time by lowering blood sugar levels.
It is important to distinguish between a direct drug effect and the underlying condition. Patients taking Ozempic who develop symptoms of thrush should not automatically attribute this to the medication itself, but rather consider their overall diabetes control, hygiene practices, and other risk factors. If you are also taking an SGLT2 inhibitor (such as dapagliflozin, empagliflozin, or canagliflozin), be aware that these medications are known to increase the risk of genital yeast infections.
If recurrent or severe yeast infections occur, a review with a GP or diabetes specialist is advisable to assess glycaemic control and exclude other contributing factors such as immunosuppression or antibiotic use. Any suspected adverse reactions to Ozempic can be reported via the MHRA Yellow Card scheme.
The relationship between diabetes and infection susceptibility is well established in clinical practice. Hyperglycaemia impairs immune function, particularly neutrophil activity and cell-mediated immunity, making individuals with poorly controlled diabetes more prone to bacterial and fungal infections. Elevated glucose levels in urine and genital secretions provide an ideal substrate for Candida species, which thrive in glucose-rich environments.
Whilst Ozempic itself does not directly promote yeast overgrowth, the broader context of diabetes management is relevant. SGLT2 inhibitors (sodium-glucose co-transporter-2 inhibitors), another class of diabetes medication, are known to increase the risk of genital mycotic infections due to their mechanism of action—promoting urinary glucose excretion. This is a recognised adverse effect documented in the BNF, NICE guidance, and MHRA Drug Safety Updates. Patients sometimes confuse medication classes, attributing side effects of one drug to another within their diabetes regimen.
It is crucial for healthcare professionals to educate patients that infection risk is multifactorial, involving glycaemic control, medication effects, personal hygiene, and immune status. If you are taking both Ozempic and an SGLT2 inhibitor and experience recurrent thrush, discuss this with your prescriber to review your treatment plan.
Patients should be counselled that optimising blood glucose levels remains the cornerstone of reducing infection risk, and any new or recurrent symptoms warrant clinical assessment rather than self-diagnosis or treatment cessation.
Genital thrush is a common fungal infection caused predominantly by Candida albicans. In women, vulvovaginal candidiasis presents with characteristic symptoms including:
Intense itching and irritation of the vulva and vaginal area
Thick, white, cottage cheese-like discharge that is typically odourless
Soreness, redness, and swelling of the vulval tissues
Discomfort or pain during sexual intercourse (dyspareunia)
Stinging or burning sensation when urinating, particularly if urine contacts inflamed skin
In men, candidal balanitis affects the glans penis and foreskin, causing:
Redness, irritation, and swelling of the glans and foreskin
White, lumpy discharge beneath the foreskin
Itching or burning sensation
Difficulty retracting the foreskin in some cases
Unpleasant odour may occasionally be present
It is important to differentiate thrush from other genital conditions, such as bacterial vaginosis, sexually transmitted infections (STIs), or dermatological conditions like lichen sclerosus. Patients experiencing symptoms for the first time, or those with recurrent episodes (four or more per year), should seek medical assessment rather than relying solely on over-the-counter treatments. Microbiological confirmation (swabs) may be needed for persistent or recurrent cases.
Red flag symptoms requiring urgent GP consultation include abnormal vaginal bleeding, severe vulval pain or fissuring, pelvic pain, fever, spreading cellulitis, severe balanitis, difficulty retracting the foreskin with pain and swelling (possible paraphimosis), or symptoms that do not resolve with standard antifungal treatment. Pregnant women, immunocompromised individuals, and those with uncontrolled diabetes should always consult a healthcare professional before self-treating. Accurate diagnosis ensures appropriate management and excludes more serious underlying conditions.
Optimising glycaemic control remains the most effective strategy for reducing yeast infection risk in patients with type 2 diabetes. Regular monitoring of HbA1c levels, adherence to prescribed medications including Ozempic, and lifestyle modifications (diet and physical activity) all contribute to maintaining blood glucose within individualised target ranges. NICE guidance (NG28) typically recommends HbA1c targets of 48–58 mmol/mol for most people with type 2 diabetes, though these should be agreed with your healthcare provider based on your specific circumstances.
Practical hygiene measures can significantly reduce candidal colonisation:
Wear loose-fitting, breathable cotton underwear and avoid synthetic fabrics that trap moisture
Change out of wet clothing promptly, particularly after exercise or swimming
Avoid perfumed soaps, bubble baths, and vaginal douches, which disrupt natural flora
Maintain good genital hygiene without over-washing, which can remove protective bacteria
Ensure the genital area is thoroughly dried after bathing
A balanced diet supporting good glycaemic control may help reduce infection risk. While some patients report that reducing refined sugar intake helps prevent recurrent thrush, this is primarily beneficial through improving overall diabetes control rather than having a direct effect on candidal growth.
Patients should be advised to complete the full course of any prescribed antifungal treatment (topical or oral). If you are pregnant, avoid oral fluconazole and use topical clotrimazole instead, following medical advice. Be aware that oral azole antifungals may interact with other medications, so always check with your pharmacist or doctor before starting treatment.
Recurrent vulvovaginal candidiasis (four or more episodes annually) warrants referral to gynaecology, sexual health/GUM, or dermatology services for investigation of underlying causes, including assessment of diabetes control, screening for immunodeficiency, and consideration of suppressive antifungal therapy.
It is essential not to discontinue Ozempic without medical advice if thrush develops, as the benefits of improved glycaemic control typically outweigh manageable side effects. Open communication with healthcare providers ensures that any concerns are addressed appropriately, and alternative management strategies can be explored if necessary.
No, Ozempic (semaglutide) is not listed as causing yeast infections in UK prescribing information. Diabetes itself increases thrush risk due to elevated blood glucose, whilst Ozempic may indirectly reduce infection risk by improving glycaemic control.
SGLT2 inhibitors (such as dapagliflozin, empagliflozin, and canagliflozin) are recognised in UK guidance as increasing genital mycotic infection risk due to their mechanism of promoting urinary glucose excretion.
Consult your GP if you experience recurrent episodes (four or more yearly), severe symptoms, first-time symptoms, or if over-the-counter treatments fail. Never discontinue Ozempic without medical advice.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.