
Wegovy (semaglutide 2.4 mg) is a once-weekly GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Many patients wonder how to get Wegovy out of your system fast after discontinuing treatment, whether due to side effects, pregnancy planning, or other reasons. Understanding Wegovy's elimination process is essential for managing expectations during the discontinuation period. This article explains how long Wegovy remains in your body, why rapid elimination is not possible, and how to manage the transition safely under medical guidance.
Quick Answer: Wegovy cannot be rapidly eliminated from your system; it takes approximately 5 weeks (35 days) for semaglutide to be naturally metabolised and cleared from the body after your last injection.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. It works by mimicking the natural hormone GLP-1, which regulates appetite and food intake by acting on areas of the brain involved in appetite control. Wegovy also slows gastric emptying and enhances insulin secretion in response to meals, contributing to its weight loss effects.
The medication is administered as a once-weekly subcutaneous injection, with doses gradually increased over 16–20 weeks to reach the maintenance dose of 2.4 mg. This slow titration schedule helps minimise gastrointestinal side effects. Once injected, semaglutide binds extensively to plasma proteins (more than 99%) and is distributed throughout the body.
Elimination occurs primarily through proteolytic degradation of the peptide backbone, similar to how the body breaks down naturally occurring proteins. According to the Summary of Product Characteristics (SmPC), semaglutide undergoes metabolism in the liver with metabolites excreted via urine and faeces in roughly equal proportions, with minimal unchanged renal excretion.
It is important to understand that Wegovy currently cannot be rapidly removed from the body through any intervention. The medication's elimination follows predictable pharmacokinetic principles based on its chemical structure and how it binds to tissues. Unlike some substances that can be filtered or dialysed out, semaglutide must be naturally metabolised over time.
Wegovy is contraindicated in pregnancy, breastfeeding, and in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Caution is advised in severe renal or hepatic impairment. Patients considering stopping Wegovy should discuss their decision with their prescribing clinician to ensure appropriate monitoring and support during the discontinuation period.
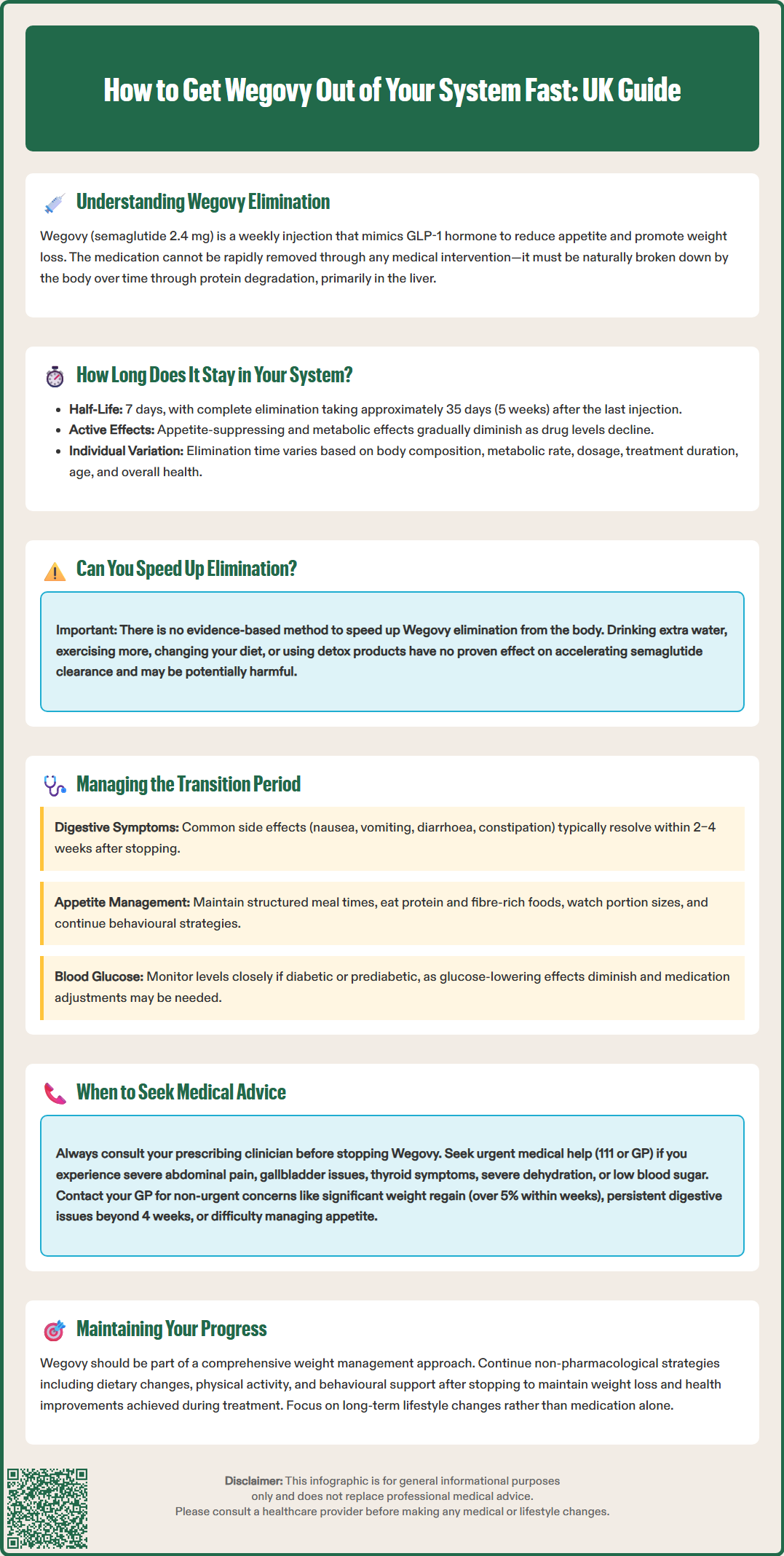
Wegovy has a half-life of approximately 7 days (around 165–184 hours), which is considerably longer than many other medications. The half-life refers to the time it takes for half of the drug concentration in the bloodstream to be eliminated. This extended half-life is intentional, allowing for convenient once-weekly dosing rather than daily injections.
Based on standard pharmacokinetic principles, it typically takes five half-lives for a medication to be considered essentially eliminated from the body. For Wegovy, this means approximately 35 days (5 weeks) after the last injection before semaglutide levels become negligible in the bloodstream. However, significant individual variation exists based on factors such as:
Body composition and weight – distribution volume may differ
Metabolic rate – affects how quickly proteins are broken down
Dose and duration of treatment – higher doses and longer treatment may extend elimination time
Individual patient factors – age, overall health status, and concurrent medications
Patients who have been taking Wegovy at the full 2.4 mg maintenance dose should expect the medication to remain active in their system for several weeks after discontinuation. During this time, the appetite-suppressing and metabolic effects will gradually diminish as drug levels decline. There is currently no evidence-based method to accelerate this natural elimination process.
It is worth noting that even after Wegovy is no longer detectable in the blood, some physiological changes induced by the medication—such as alterations in eating patterns or metabolic adaptations—may persist temporarily. The body requires time to readjust to functioning without the medication's influence on appetite regulation and glucose metabolism.
There is currently no evidence-based method to accelerate the elimination of Wegovy from the body. Unlike some medications that can be removed through dialysis, activated charcoal, or forced diuresis, semaglutide must be naturally metabolised through proteolytic breakdown. The medication's chemical structure and extensive protein binding mean it cannot be filtered out or flushed from the system.
Several commonly suggested approaches have no proven effect on speeding up Wegovy elimination:
Increased hydration – whilst important for general health, drinking extra water does not significantly enhance semaglutide clearance, as the drug is not primarily eliminated via the kidneys in unchanged form
Exercise – physical activity supports overall metabolic health but does not accelerate the enzymatic breakdown of semaglutide
Dietary changes – no specific foods or supplements have been shown to increase the rate of semaglutide metabolism
Detoxification products – these have no scientific basis for affecting GLP-1 receptor agonist elimination
Attempting unproven methods to remove Wegovy from your system may be ineffective at best and potentially harmful at worst. Some "detox" products can cause dehydration, electrolyte imbalances, or interactions with other medications.
The safest approach is to allow natural elimination to occur whilst managing any side effects appropriately. If you have stopped Wegovy due to adverse effects or other concerns, focus on symptomatic management and maintaining good general health practices. Adequate hydration, balanced nutrition, and regular communication with your healthcare provider are the most appropriate strategies during the elimination period. Patients should never attempt to "flush out" medications without medical supervision, as this can lead to complications or mask symptoms that require clinical attention.
As Wegovy gradually leaves your system over approximately 5 weeks, you may experience changes in both side effects and the therapeutic effects you had become accustomed to. Understanding what to expect can help you manage this transition period more effectively.
Gastrointestinal symptoms, the most common side effects of Wegovy, typically improve as drug levels decline. These include:
Nausea and vomiting
Diarrhoea or constipation
Abdominal discomfort or bloating
Reduced appetite
These symptoms usually resolve within 2–4 weeks after stopping treatment, though the timeline varies individually. During this period, focus on gentle, easily digestible foods and small, frequent meals if nausea persists. Adequate hydration remains important, particularly if you have experienced vomiting or diarrhoea.
Return of appetite is one of the most noticeable changes patients report after discontinuing Wegovy. As the medication's appetite-suppressing effects wane, you may experience increased hunger and food cravings. This is a normal physiological response and does not indicate a problem. To manage this transition:
Maintain structured meal times with balanced, nutritious foods
Include adequate protein and fibre to promote satiety
Stay mindful of portion sizes
Continue any behavioural strategies learned during treatment
Consider support from a dietitian for ongoing weight management
Blood glucose levels may change in patients with type 2 diabetes or prediabetes, as Wegovy's glucose-lowering effects diminish. If you monitor your blood glucose, continue regular testing and report any significant changes to your diabetes care team. Adjustments to other diabetes medications may be necessary.
Some patients report fatigue or mood changes during the discontinuation period, though there is no official link established between stopping Wegovy and these symptoms. Maintaining good sleep hygiene, regular physical activity, and stress management techniques can support overall wellbeing during this adjustment phase.
Rare but serious adverse reactions can occur with Wegovy, including thyroid C-cell tumours, pancreatitis, gallbladder problems, and diabetic retinopathy complications. If you experience any concerning symptoms after stopping Wegovy, seek medical advice. Patients are encouraged to report suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Discontinuing Wegovy should ideally be discussed with your prescribing clinician before stopping treatment, though this is not always possible in emergency situations. Certain circumstances require prompt medical attention during or after stopping Wegovy.
Seek urgent medical advice (contact 111 or your GP) if you experience:
Severe or persistent abdominal pain, particularly if accompanied by vomiting – this could indicate pancreatitis, a rare but serious side effect that requires immediate assessment
Signs of gallbladder problems – pain in the upper right abdomen, fever, yellowing of skin or eyes
Symptoms of thyroid problems – lump or swelling in the neck, persistent hoarseness, difficulty swallowing
Severe dehydration – inability to keep fluids down, dizziness, reduced urination, confusion
Hypoglycaemia symptoms in patients with diabetes – particularly if taking insulin or sulfonylureas alongside Wegovy
Contact your GP or diabetes team for non-urgent concerns such as:
Significant weight regain (more than 5% of body weight) within weeks of stopping
Difficulty managing appetite or eating behaviours
Changes in blood glucose control requiring medication adjustment
Persistent gastrointestinal symptoms beyond 4 weeks after the last dose
Questions about restarting Wegovy or alternative weight management options
If you stopped Wegovy due to side effects, inform your prescriber so they can document this in your medical records and consider reporting via the Yellow Card Scheme. This information is important for future prescribing decisions and helps identify patterns of adverse reactions. Your clinician can also provide guidance on alternative weight management strategies, including other medications, dietary support, or referral to specialist weight management services.
NICE guidance (TA875 and NG136) emphasises that pharmacological treatment for obesity should be part of a comprehensive approach including dietary modification, physical activity, and behavioural interventions. In the UK, Wegovy is typically prescribed through specialist weight management services (tier 3 or 4) according to specific eligibility criteria. Continuing non-pharmacological strategies after stopping Wegovy provides the best opportunity for maintaining weight loss and metabolic improvements achieved during treatment.
Wegovy takes approximately 5 weeks (35 days) to be essentially eliminated from your system after the last injection, based on its 7-day half-life. Individual factors such as body composition, metabolic rate, and treatment duration may cause slight variations in this timeline.
No, increased hydration does not significantly accelerate Wegovy elimination. Semaglutide is broken down through proteolytic degradation rather than being excreted unchanged in urine, so drinking extra water will not speed up the clearance process.
Appetite typically returns gradually as Wegovy leaves your system over several weeks. Patients often experience increased hunger and food cravings as the medication's appetite-suppressing effects diminish, making it important to maintain structured eating patterns and behavioural strategies learned during treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.