
Many people wonder whether Ozempic can help with fertility, particularly given its association with weight loss. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst not approved for fertility treatment, the weight loss that may occur with Ozempic could indirectly improve reproductive health in people with obesity-related fertility problems. However, semaglutide should not be used during pregnancy and must be stopped at least two months before attempting to conceive. This article examines the evidence linking Ozempic, weight loss, and fertility, and explores alternative evidence-based treatments available through the NHS.
Quick Answer: Ozempic is not licensed for fertility treatment, but weight loss achieved with the medication may indirectly improve fertility in people with obesity-related reproductive difficulties.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood sugar levels and appetite.
The medication is administered as a once-weekly subcutaneous injection and works through several mechanisms. Primarily, it stimulates insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Ozempic also slows gastric emptying, which helps to reduce appetite and promote a feeling of fullness after eating. These combined effects lead to improved glycaemic control in people with type 2 diabetes.
Whilst Ozempic is not licensed for weight loss in the UK, clinically meaningful weight loss may occur for many people as a secondary benefit of treatment. This has led to increased interest in its potential effects on conditions associated with obesity, including fertility problems. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved semaglutide for weight management under a different brand name (Wegovy) at higher doses. These are separate UK marketing authorisations with different licensed indications and dose ranges and are not interchangeable.
It is important to note that Ozempic is not currently licensed or recommended for fertility treatment in the UK. Any use of the medication should be under the supervision of a qualified healthcare professional, and patients should discuss their individual circumstances and treatment goals with their GP or specialist.
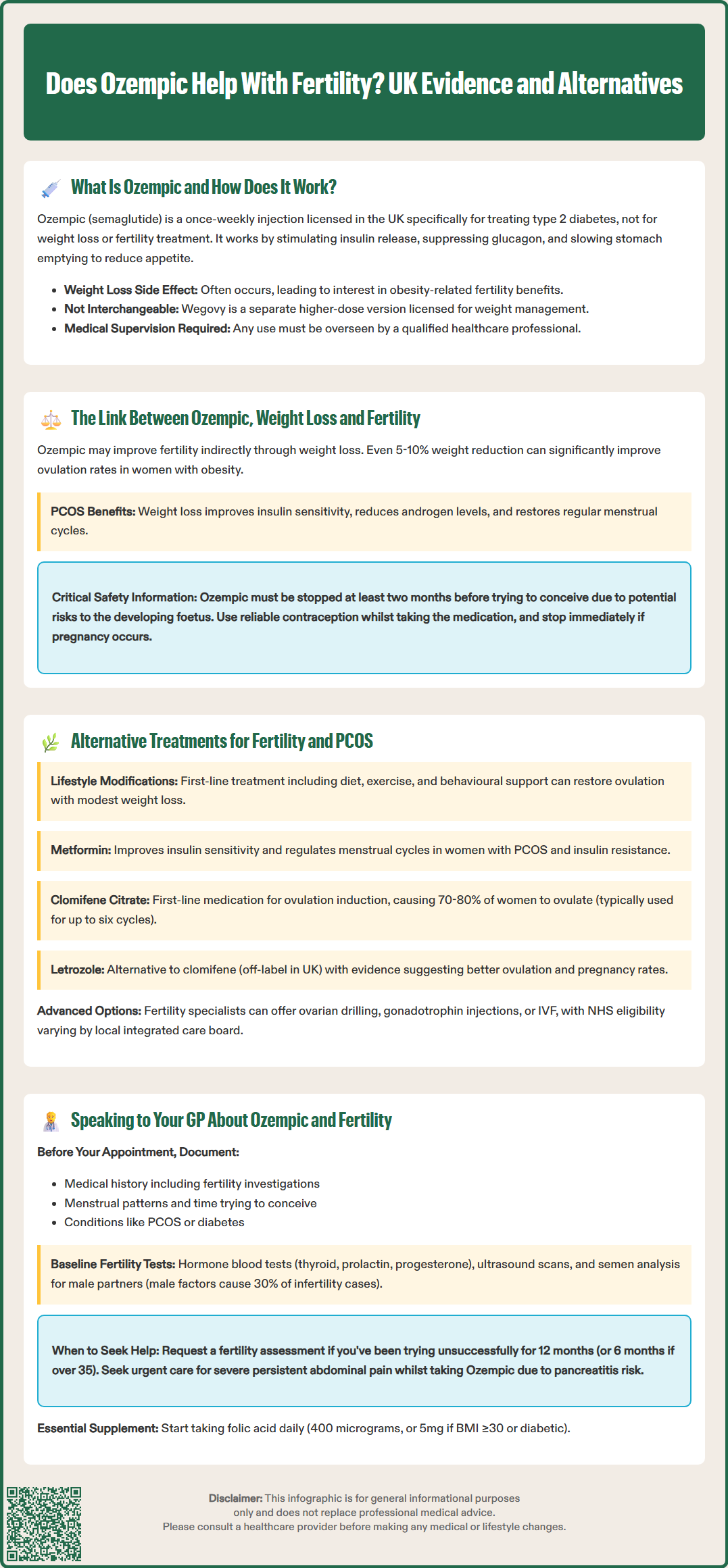
The relationship between Ozempic and fertility is indirect and primarily mediated through weight loss. Obesity is a well-established risk factor for reproductive difficulties in both women and men. In women, excess weight is strongly associated with polycystic ovary syndrome (PCOS), anovulation (lack of ovulation), and menstrual irregularities. Research demonstrates that even modest weight reduction of 5–10% can significantly improve ovulation rates and fertility outcomes in women with obesity.
Weight loss achieved through Ozempic may therefore improve fertility by addressing the underlying metabolic dysfunction associated with obesity. Studies have shown that GLP-1 receptor agonists (primarily liraglutide and exenatide, with limited semaglutide-specific data) can improve insulin sensitivity, reduce androgen levels, and restore more regular menstrual cycles in women with PCOS. These metabolic improvements create a more favourable hormonal environment for conception. However, there is no official evidence that Ozempic directly enhances fertility independent of its weight loss effects.
An important consideration is that semaglutide should not be used during pregnancy. Animal studies have shown potential risks to the developing foetus, and the medication should be discontinued at least two months before attempting to conceive. If pregnancy occurs whilst taking semaglutide, the medication should be stopped immediately and medical advice sought. Women of childbearing potential should use reliable contraception whilst taking Ozempic. While semaglutide has not shown a clinically relevant effect on combined oral contraceptive exposure, effective contraception is still advised.
Currently, NICE guidance does not recommend Ozempic specifically for fertility enhancement. Any potential fertility benefits should be viewed as secondary to its primary indication for diabetes management. Patients considering Ozempic for weight-related fertility concerns should discuss evidence-based fertility treatments with their healthcare provider.
For women experiencing fertility difficulties related to PCOS or obesity, several evidence-based treatment options are available through the NHS. The first-line approach recommended by NICE involves lifestyle modifications, including dietary changes, increased physical activity, and behavioural support to achieve sustainable weight loss. Even modest weight reduction can restore ovulation and improve pregnancy rates without pharmacological intervention.
Metformin is commonly prescribed for women with PCOS, particularly those with insulin resistance. This medication improves insulin sensitivity and can help regulate menstrual cycles, though its effect on fertility outcomes is modest. NICE guidance suggests metformin may be considered alongside clomifene citrate (see below) in women with PCOS who have not responded to lifestyle changes alone. Metformin is generally well-tolerated, with gastrointestinal side effects being the most common complaint.
Clomifene citrate (also known as clomiphene) is the first-line medical treatment for ovulation induction in women with PCOS who are not ovulating regularly according to NICE guidance. This medication stimulates the ovaries to produce eggs and is typically used for up to six cycles. Success rates vary, but approximately 70–80% of women will ovulate with clomifene treatment. For women who do not respond to clomifene, letrozole (an aromatase inhibitor) may be considered as an alternative. It is important to note that letrozole for ovulation induction is used off-label in the UK, though many fertility specialists now use it as first-line treatment based on evidence suggesting superior ovulation and pregnancy rates. Local policies may vary, so discussion with a fertility specialist is advised.
For more complex cases, referral to a fertility specialist may be appropriate. Treatment options may include ovarian drilling (a laparoscopic surgical procedure for ovulation induction), gonadotrophin injections (which require careful monitoring due to risks of multiple pregnancy and ovarian hyperstimulation syndrome), or in vitro fertilisation (IVF). The NHS provides fertility services according to specific eligibility criteria, which vary by local integrated care board (ICB). Patients should discuss their options with their GP, who can provide appropriate referrals and guidance on accessing fertility services.
If you are considering Ozempic in relation to fertility concerns, it is essential to have an open and informed discussion with your GP. Prepare for your appointment by noting down your medical history, including any previous fertility investigations, menstrual cycle patterns, duration of trying to conceive, and any diagnosed conditions such as PCOS or type 2 diabetes. This information will help your GP provide tailored advice.
Key questions to discuss include whether Ozempic is appropriate for your specific situation, what the evidence shows regarding weight loss and fertility improvement, and what alternative treatments might be more suitable. Your GP can explain the risks and benefits of different approaches and help you understand realistic expectations. It is particularly important to discuss that semaglutide should not be used during pregnancy and the need for effective contraception whilst taking the medication, as well as the recommended two-month washout period before attempting conception. If pregnancy occurs whilst taking semaglutide, stop the medication immediately and contact your healthcare provider.
Your GP may recommend baseline fertility investigations before considering any treatment. These typically include blood tests to assess hormone levels (including thyroid function, prolactin, and mid-luteal progesterone to confirm ovulation), and possibly an ultrasound scan to evaluate the ovaries and uterus. For couples, a semen analysis for the male partner is also standard practice, as male factor infertility accounts for approximately 30% of cases. Preconception advice, including taking folic acid (400 micrograms daily, or 5 mg for higher-risk groups such as those with a BMI ≥30 or diabetes), should also be discussed.
When to seek urgent advice: If you experience severe, persistent abdominal pain (with or without vomiting) whilst taking Ozempic, seek urgent medical assessment (via NHS 111, urgent care, or A&E) due to the risk of pancreatitis, and stop taking the medication pending review. Contact your GP promptly if you experience unexpected pregnancy symptoms whilst taking Ozempic or any concerning side effects from the medication. If you suspect a side effect from Ozempic, you can report it via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk). If you have been trying to conceive for 12 months without success (or 6 months if you are over 35 years old), you should request a fertility assessment. Your GP can then refer you to appropriate specialist services and discuss evidence-based treatment pathways that align with NICE guidance and your individual circumstances.
No, Ozempic should be stopped at least two months before attempting to conceive due to potential risks to the developing foetus. Women of childbearing potential should use reliable contraception whilst taking semaglutide.
There is no evidence that Ozempic directly enhances fertility. Any potential fertility benefits are indirect, resulting from weight loss and improved metabolic health in people with obesity-related reproductive difficulties.
NICE recommends lifestyle modifications as first-line treatment, followed by clomifene citrate for ovulation induction. Metformin may be considered alongside clomifene in women with insulin resistance who have not responded to lifestyle changes alone.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.