Does Ozempic make you sleepy? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst sleepiness is not listed as a common side effect in the MHRA-approved Summary of Product Characteristics, some patients report fatigue during treatment. This tiredness is typically indirect, linked to gastrointestinal effects such as nausea and reduced appetite, blood glucose fluctuations, or the underlying diabetes itself. Understanding the causes of fatigue and knowing when to seek medical advice can help you manage your treatment effectively and maintain your quality of life.
Quick Answer: Ozempic does not typically cause sleepiness, but some patients report fatigue, usually linked to gastrointestinal side effects, reduced food intake, or blood glucose changes rather than direct sedative effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is administered as a once-weekly injection, with doses typically starting low and gradually increasing over time. Whilst sleepiness or drowsiness is not listed as a common side effect in the official Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), some patients do report feeling tired or fatigued whilst taking this medication.
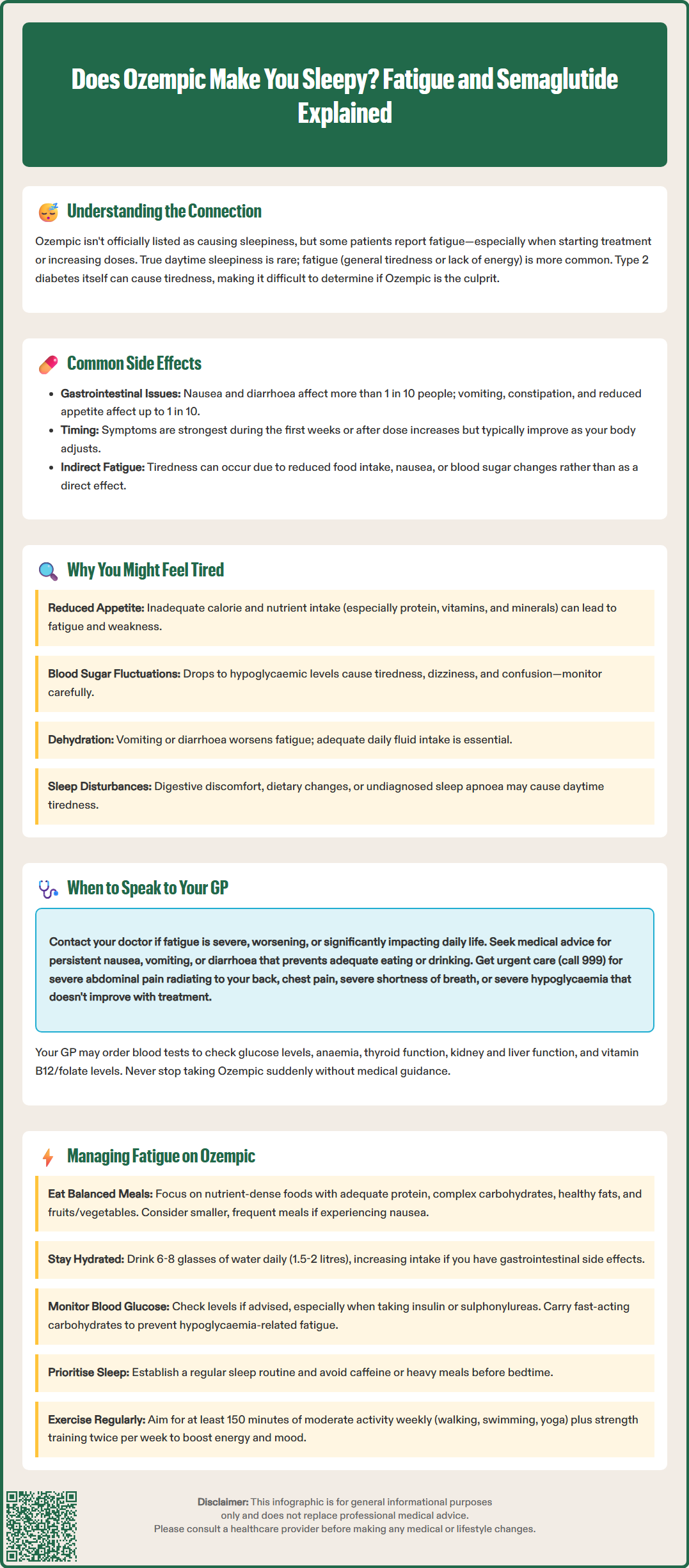
It is important to distinguish between sleepiness (somnolence) and fatigue (a general sense of tiredness or lack of energy). True sleepiness—an overwhelming urge to sleep during the day—is rarely directly attributed to Ozempic. However, fatigue may be reported by some patients, particularly during the initial weeks of treatment or following dose increases.
Understanding whether tiredness is related to the medication itself, the underlying condition being treated, or other lifestyle factors is essential. Type 2 diabetes can itself cause fatigue, particularly when blood glucose levels are poorly controlled. Additionally, the gastrointestinal side effects commonly associated with Ozempic—such as nausea, vomiting, and reduced appetite—may indirectly contribute to feelings of tiredness by affecting nutritional intake and overall wellbeing.
This article explores the relationship between Ozempic and feelings of tiredness, examines the potential mechanisms behind fatigue in patients using this medication, and provides practical guidance on when to seek medical advice and how to manage symptoms effectively.
Ozempic works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. These mechanisms contribute to improved glycaemic control and often result in weight loss, both of which are therapeutic goals in type 2 diabetes management.
According to the MHRA-approved SmPC, the most commonly reported side effects of Ozempic include:
Nausea (very common: may affect more than 1 in 10 people)
Diarrhoea (very common: may affect more than 1 in 10 people)
Vomiting (common: may affect up to 1 in 10 people)
Constipation (common: may affect up to 1 in 10 people)
Abdominal pain (common: may affect up to 1 in 10 people)
Decreased appetite (common: may affect up to 1 in 10 people)
These gastrointestinal symptoms are typically most pronounced during the initial weeks of treatment or following dose escalation, and they often improve over time as the body adjusts to the medication. However, persistent nausea and reduced food intake can lead to inadequate calorie and nutrient consumption, which may manifest as generalised fatigue or low energy levels.
Whilst fatigue itself is not classified as a common side effect in clinical trial data, it has been reported by some patients. The relationship is likely indirect—stemming from the gastrointestinal effects, changes in eating patterns, or adjustments in blood glucose levels rather than a direct pharmacological action on the central nervous system.
Additionally, hypoglycaemia (low blood sugar) can occur, particularly when Ozempic is used in combination with other glucose-lowering medications such as sulphonylureas or insulin. The risk of hypoglycaemia with Ozempic monotherapy is low. Hypoglycaemia is a well-recognised cause of fatigue, weakness, and confusion, and patients should be aware of the symptoms and how to manage them appropriately.
It's important to be aware of serious but rare side effects that require urgent medical attention, including severe, persistent abdominal pain (with or without vomiting) which may indicate acute pancreatitis, or right upper abdominal pain, fever or jaundice which could suggest gallbladder disease.
Several factors may contribute to feelings of tiredness in individuals taking Ozempic, and it is important to consider these in a holistic manner rather than attributing fatigue solely to the medication.
Caloric restriction and nutritional deficiency are significant contributors. Ozempic reduces appetite and can lead to decreased energy intake. Whilst this is beneficial for weight loss, insufficient energy intake—particularly if protein, vitamins, and minerals are lacking—can result in fatigue, weakness, and reduced physical stamina. Patients may inadvertently under-eat, especially if nausea is prominent.
Blood glucose fluctuations also play a role. As Ozempic improves glycaemic control, patients who were previously experiencing hyperglycaemia (high blood sugar) may notice a period of adjustment as their glucose levels normalise. Conversely, if blood glucose drops too low, hypoglycaemia can cause acute tiredness, dizziness, and confusion. If you have been advised to self-monitor your blood glucose, this is particularly important during the initial treatment period and following dose adjustments, especially if you are also taking insulin or sulphonylureas.
Dehydration secondary to gastrointestinal side effects such as vomiting or diarrhoea can exacerbate feelings of fatigue. Maintaining adequate hydration is crucial, and patients should be encouraged to drink sufficient fluids throughout the day.
Sleep disturbances may also be a factor. Some patients report changes in sleep patterns, possibly related to gastrointestinal discomfort, dietary changes, or anxiety about managing a chronic condition. Poor-quality sleep naturally leads to daytime tiredness. Additionally, obstructive sleep apnoea, which is more common in people with obesity or type 2 diabetes, can contribute to fatigue if undiagnosed or untreated.
Finally, it is essential to consider that underlying type 2 diabetes itself is a common cause of fatigue, particularly if glycaemic control has been suboptimal for an extended period. Other comorbidities such as thyroid dysfunction, anaemia, depression, or sleep apnoea should also be considered if fatigue is persistent or severe.
Whilst mild, transient tiredness during the initial weeks of Ozempic treatment may be expected as the body adjusts, there are specific circumstances in which you should contact your GP or diabetes specialist nurse for further assessment.
Seek medical advice if:
Fatigue is severe or worsening and is significantly affecting your daily activities, work, or quality of life.
You experience symptoms of hypoglycaemia, such as sweating, trembling, confusion, palpitations, or dizziness, particularly if you are taking other diabetes medications. Treat mild hypoglycaemia immediately with fast-acting carbohydrates (e.g., glucose tablets, fruit juice).
You have persistent nausea, vomiting, or diarrhoea that prevents you from eating or drinking adequately, or if you notice signs of dehydration (dark urine, dry mouth, dizziness on standing).
You develop new or unexplained symptoms such as shortness of breath, chest pain, swelling of the legs, or significant unintentional weight loss beyond what is expected.
You notice mood changes, low mood, or loss of interest in activities, which may indicate depression—a condition that can coexist with chronic illness and contribute to fatigue.
Seek urgent medical attention if:
You experience severe, persistent abdominal pain (with or without vomiting) or pain radiating to your back, which could indicate acute pancreatitis.
You develop right-sided upper abdominal pain, fever, or yellowing of the skin or eyes (jaundice), which may suggest gallbladder disease.
You have chest pain or severe shortness of breath – call 999 immediately.
You have severe hypoglycaemia that doesn't improve with treatment or if someone becomes unconscious – call 999.
Your GP may wish to perform a clinical assessment and arrange investigations such as:
Blood glucose monitoring (including HbA1c to assess overall glycaemic control)
Full blood count (to exclude anaemia)
Thyroid function tests (to rule out hypothyroidism)
Renal and liver function tests
Vitamin B12 and folate levels, particularly if you are also taking metformin
It is important not to stop Ozempic abruptly without medical guidance. Your healthcare team can help determine whether the fatigue is related to the medication, your diabetes management, or another underlying cause, and they can adjust your treatment plan accordingly.
If you suspect your symptoms are related to Ozempic, you can report side effects directly via the MHRA Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for 'MHRA Yellow Card' in the Google Play or Apple App Store.
If you are experiencing tiredness whilst taking Ozempic, there are several practical strategies that may help improve your energy levels and overall wellbeing.
Optimise your nutrition: Even though your appetite may be reduced, it is essential to consume balanced, nutrient-dense meals. Focus on:
Adequate protein intake (lean meats, fish, eggs, pulses, dairy) to support muscle mass and energy
Complex carbohydrates (whole grains, vegetables) for sustained energy release
Healthy fats (nuts, seeds, oily fish, avocado)
Plenty of fruits and vegetables to ensure sufficient vitamins and minerals
Eating smaller, more frequent meals may be better tolerated if nausea is an issue. Consider consulting a registered dietitian with experience in diabetes management for personalised advice.
Stay well hydrated: Aim for 6-8 drinks daily (about 1.5 to 2 litres), and increase this if you are experiencing gastrointestinal side effects.
Monitor your blood glucose if advised: If you have been recommended to self-monitor your blood glucose, this helps identify patterns of hypoglycaemia or hyperglycaemia that may be contributing to fatigue. This is particularly important if you are also taking insulin or sulphonylureas. If you are at risk of hypoglycaemia, always carry fast-acting carbohydrate (such as glucose tablets or fruit juice) with you.
Prioritise good sleep hygiene: Establish a regular sleep routine, avoid caffeine and heavy meals before bed, and create a comfortable sleep environment.
Engage in regular physical activity: Whilst it may seem counterintuitive, gentle exercise such as walking, swimming, or yoga can actually boost energy levels and improve mood. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity per week for adults, plus strength activities on at least 2 days per week.
Manage stress and mental health: Chronic illness can be emotionally taxing. Consider speaking to your GP about psychological support or counselling if you are feeling overwhelmed.
If you are taking Ozempic alongside insulin or sulphonylureas, discuss with your healthcare provider whether dose adjustments of these medications might be needed to reduce the risk of hypoglycaemia.
By taking a proactive, holistic approach to managing your health whilst on Ozempic, you can minimise fatigue and maximise the therapeutic benefits of your treatment.
No, sleepiness is not listed as a common side effect in the MHRA-approved product information for Ozempic. However, some patients may experience fatigue, often related to gastrointestinal side effects, reduced food intake, or blood glucose changes rather than a direct sedative effect of the medication.
Tiredness on Ozempic may result from reduced appetite leading to inadequate nutrition, blood glucose fluctuations, dehydration from gastrointestinal side effects, or the underlying type 2 diabetes itself. Hypoglycaemia can also cause fatigue, particularly if Ozempic is combined with insulin or sulphonylureas.
Contact your GP if fatigue is severe or worsening, if you experience symptoms of hypoglycaemia, persistent nausea or vomiting preventing adequate intake, or new symptoms such as shortness of breath or mood changes. Seek urgent care for severe abdominal pain, jaundice, chest pain, or severe hypoglycaemia.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.