
Does Ozempic make you thirsty? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst increased thirst is not listed as a common adverse effect in the Summary of Product Characteristics, some patients may experience this symptom during treatment. Thirst is not a direct pharmacological effect of Ozempic, but may arise from improved glycaemic control, gastrointestinal side effects such as nausea or diarrhoea causing dehydration, or changes in fluid balance. Understanding the underlying cause is essential for appropriate management and ensuring patient safety throughout treatment.
Quick Answer: Ozempic does not directly cause thirst, but some patients may experience this symptom due to improved glycaemic control, gastrointestinal side effects leading to dehydration, or changes in fluid balance.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Increased thirst is not listed as a common adverse effect in the Summary of Product Characteristics (SmPC), though some patients may experience thirst during treatment. Understanding whether this symptom relates to the medication itself or reflects underlying metabolic changes is important for both patients and healthcare professionals.
The mechanism of action of semaglutide involves enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. These effects help to lower blood glucose levels in people with type 2 diabetes. Thirst itself is not a recognised direct pharmacological effect of Ozempic, but several indirect factors may contribute to this sensation during treatment.
When patients experience thirst whilst taking Ozempic, it is essential to consider the broader clinical context. Improved glycaemic control may reduce the excessive thirst (polydipsia) that often accompanies poorly controlled diabetes. Gastrointestinal side effects such as nausea, vomiting, and diarrhoea—which are very common with GLP-1 receptor agonists according to the SmPC—can lead to dehydration and secondary thirst.
Patients should be reassured that mild thirst is generally manageable and often reflects the body's natural response to changes in fluid balance or glucose metabolism. However, persistent or severe thirst warrants further evaluation to exclude complications such as hyperglycaemia or dehydration.
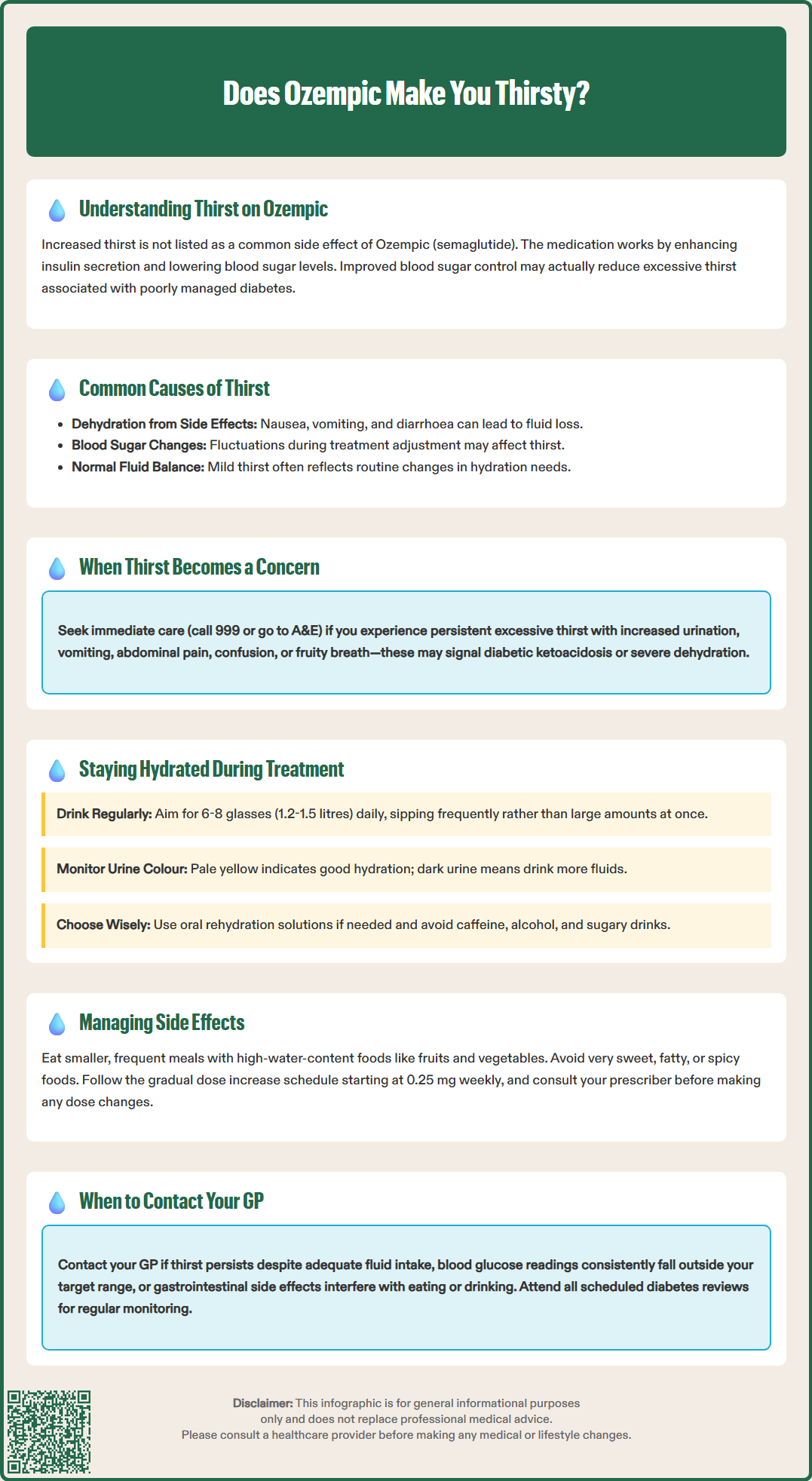
Whilst mild thirst during Ozempic treatment may be benign, certain patterns or accompanying symptoms should prompt clinical concern. Persistent or excessive thirst (polydipsia) may indicate inadequate diabetes control, particularly if blood glucose levels remain elevated despite treatment. Hyperglycaemia causes an osmotic diuresis, leading to increased urination (polyuria) and compensatory thirst. Patients should be advised to monitor their blood glucose levels regularly, especially if thirst is accompanied by increased urination, fatigue, or blurred vision.
Patients taking Ozempic alongside other glucose-lowering medications such as sulphonylureas or insulin have an increased risk of hypoglycaemia. Typical symptoms of hypoglycaemia include sweating, tremor, hunger, confusion, and palpitations. Thirst is not a typical symptom of hypoglycaemia, but patients should check their blood glucose if experiencing any concerning symptoms and follow their individualised hypoglycaemia management plan.
Dehydration is an important consideration, especially in patients experiencing gastrointestinal adverse effects. Nausea and diarrhoea are very common, and vomiting is common with GLP-1 receptor agonists according to the SmPC, and can lead to significant fluid loss. Signs of dehydration include dry mouth, reduced urine output, dizziness, and concentrated urine. Elderly patients and those with comorbidities such as chronic kidney disease are at higher risk of dehydration and subsequent acute kidney injury.
Rarely, excessive thirst may indicate diabetic ketoacidosis (DKA), although this is uncommon in type 2 diabetes. Warning signs include persistent hyperglycaemia, nausea, vomiting, abdominal pain, and fruity-smelling breath. DKA is a medical emergency requiring immediate hospital assessment—patients should call 999 or go to A&E if these symptoms develop.
Patients should also be aware of symptoms of acute pancreatitis, a rare but serious adverse reaction associated with GLP-1 receptor agonists. Severe, persistent abdominal pain radiating to the back, with or without vomiting, requires urgent medical assessment and Ozempic should be discontinued if pancreatitis is suspected, as stated in the SmPC.
Maintaining adequate hydration is essential for patients taking Ozempic, particularly during the initial titration phase when gastrointestinal side effects are most common. Patients should be encouraged to drink regularly throughout the day, aiming for 6-8 drinks (approximately 1.2-1.5 litres) daily, in line with NHS guidance. This should be adjusted according to individual needs, activity levels, and climate. Patients with conditions requiring fluid restriction (such as heart failure or advanced kidney disease) should seek specific advice from their healthcare team. Sipping water frequently rather than consuming large volumes at once may help those experiencing nausea.
For patients with gastrointestinal symptoms, oral rehydration solutions may be beneficial, particularly if vomiting or diarrhoea is present. These solutions contain balanced electrolytes and glucose to optimise fluid absorption. Patients should avoid excessive caffeine and alcohol, as both can contribute to dehydration. Sugar-sweetened beverages should be avoided, especially during periods of hyperglycaemia. Monitoring urine colour is a simple, practical method to assess hydration status—pale yellow urine generally indicates adequate hydration, whilst dark urine suggests the need for increased fluid intake.
Blood glucose monitoring plays a crucial role in managing thirst related to glycaemic fluctuations. Patients should test their blood glucose levels as advised by their diabetes care team, particularly if thirst is accompanied by other symptoms. Keeping a symptom diary can help identify patterns and triggers, facilitating discussions with healthcare professionals about potential treatment adjustments.
Dietary modifications may also help manage side effects and maintain hydration. Eating smaller, more frequent meals can reduce nausea and improve tolerance of oral fluids. Foods with high water content, such as fruits and vegetables, contribute to overall hydration. Patients should be advised to avoid very sweet, fatty, or spicy foods if these exacerbate gastrointestinal symptoms.
Gradual dose titration, as recommended in the prescribing information, helps minimise adverse effects. The standard initiation regimen begins with 0.25 mg once weekly for four weeks (an initiation dose not intended for glycaemic control), increasing to 0.5 mg weekly, with further increases to 1 mg or 2 mg if required for glycaemic control. If gastrointestinal side effects occur, clinicians may delay dose escalation or step down to a previously tolerated dose. Patients should not adjust their dose without consulting their prescriber.
Patients should be advised to contact their GP or diabetes care team if thirst persists despite adequate fluid intake or if it is accompanied by concerning symptoms. Immediate medical attention is required if thirst occurs alongside signs of severe dehydration (dizziness, confusion, reduced urine output), persistent vomiting preventing oral intake, or symptoms suggestive of diabetic ketoacidosis (persistent high blood glucose, abdominal pain, rapid breathing, altered consciousness). In these emergency situations, patients should call 999 or go directly to A&E.
Patients should also seek urgent medical care if they develop symptoms of acute pancreatitis (severe, persistent abdominal pain radiating to the back, with or without vomiting). The SmPC advises that Ozempic should be discontinued if pancreatitis is suspected.
Routine GP consultation is appropriate if thirst is persistent and unexplained, particularly if blood glucose readings are consistently outside the target range. Patients should bring their blood glucose diary and a list of all medications to the appointment. The GP may need to review the overall diabetes management plan, assess for potential drug interactions, or investigate alternative causes of thirst such as hypercalcaemia or diabetes insipidus.
Patients experiencing significant gastrointestinal side effects that interfere with hydration or nutrition should also seek medical advice. The GP may recommend antiemetic medications, delaying dose escalation, or stepping down to a previously tolerated dose. According to NICE guidance on type 2 diabetes management (NG28), treatment should be individualised, and medications causing intolerable side effects should be reviewed.
Regular monitoring is essential for all patients taking Ozempic. This includes periodic assessment of HbA1c, renal function, and body weight. Patients should attend scheduled diabetes reviews and report any new or worsening symptoms promptly. Healthcare professionals should provide clear safety-netting advice, ensuring patients understand when to seek help and how to access urgent care if needed.
For non-urgent concerns about thirst or hydration, patients can contact their GP practice, diabetes specialist nurse, or NHS 111 for advice. Patients and healthcare professionals are encouraged to report suspected adverse reactions to Ozempic via the MHRA Yellow Card Scheme. Maintaining open communication with the healthcare team enables timely identification and management of potential complications, optimising both safety and treatment outcomes during Ozempic therapy.
Thirst is not listed as a common adverse effect in the Ozempic Summary of Product Characteristics. However, some patients may experience thirst indirectly due to gastrointestinal side effects causing dehydration or changes in glycaemic control affecting fluid balance.
Contact your GP if thirst persists despite adequate fluid intake, is accompanied by consistently high blood glucose readings, or occurs with signs of dehydration. Seek immediate medical attention (999 or A&E) if you experience persistent vomiting, confusion, severe abdominal pain, or symptoms of diabetic ketoacidosis.
Maintain adequate hydration by drinking 6-8 drinks daily (approximately 1.2-1.5 litres), sipping water frequently throughout the day. Monitor your blood glucose regularly, keep a symptom diary, and consider oral rehydration solutions if experiencing gastrointestinal side effects such as nausea or diarrhoea.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.