
Many people using Ozempic (semaglutide) for type 2 diabetes wonder whether the medication's effects diminish as the week progresses between injections. Ozempic is a once-weekly GLP-1 receptor agonist that works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying. With a half-life of approximately one week, the medication is specifically designed to maintain stable therapeutic levels throughout the entire dosing interval. Whilst some patients report fluctuating appetite suppression or gastrointestinal symptoms during the week, the glucose-lowering efficacy remains consistent. Understanding how Ozempic works and what to expect can help you manage your diabetes effectively and recognise when to seek medical advice.
Quick Answer: Ozempic does not wear off during the week—its one-week half-life maintains stable therapeutic concentrations and consistent glucose-lowering effects throughout the seven-day dosing interval.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. This medication enhances glucose-dependent insulin secretion from pancreatic beta cells, meaning it stimulates insulin release only when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia compared to some other diabetes medications. However, this risk increases when Ozempic is used in combination with insulin or sulfonylureas.
Beyond its effects on insulin, Ozempic also suppresses glucagon secretion from pancreatic alpha cells, which helps prevent the liver from releasing excess glucose into the bloodstream. Additionally, it slows gastric emptying, meaning food moves more gradually from the stomach into the small intestine. This mechanism contributes to increased satiety and reduced appetite, which can support weight management—a beneficial effect for many patients with type 2 diabetes, though Ozempic is not licensed specifically for weight management (Wegovy is the licensed semaglutide product for weight management).
Ozempic is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. According to the MHRA product information, the medication has a long half-life of approximately one week (around 165 hours), which allows it to maintain therapeutic levels in the body between doses. After starting treatment or increasing the dose, it takes roughly four to five weeks to reach steady-state concentrations in the bloodstream. This pharmacokinetic profile is specifically designed to provide consistent glucose control throughout the entire week, rather than requiring daily dosing like some other diabetes medications.
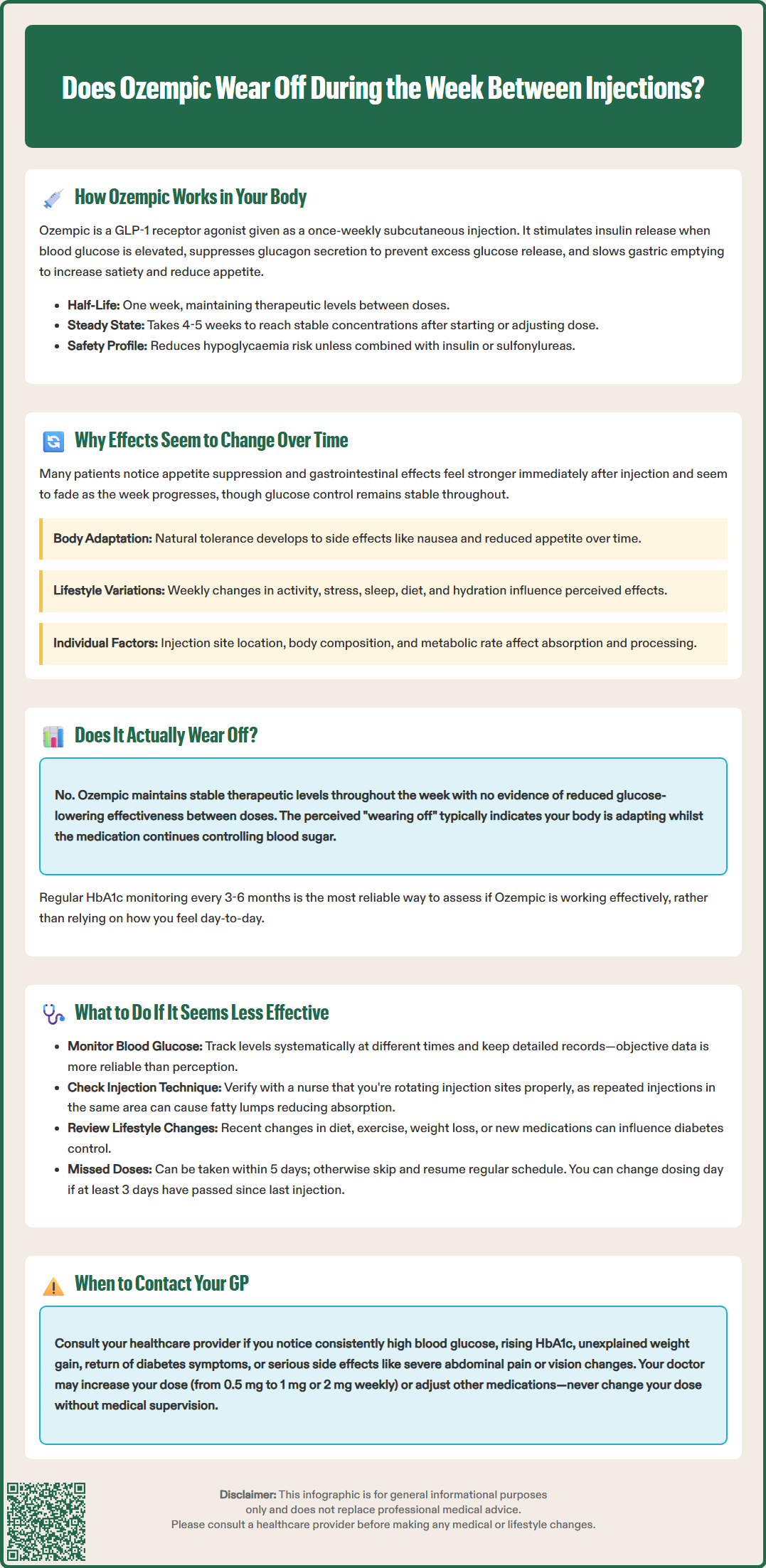
Many patients report experiencing fluctuating effects from Ozempic during the week, particularly regarding appetite suppression and gastrointestinal symptoms. These perceived changes can occur for several physiological and practical reasons, though it's important to understand that the medication's glucose-lowering effects remain relatively stable throughout the dosing interval.
One common reason for perceived variation is the natural fluctuation in appetite and eating patterns. Immediately following your weekly injection, you may notice more pronounced appetite suppression or gastrointestinal effects such as nausea or early satiety. As the week progresses, your body may adapt to the medication's presence, and these subjective effects might feel less intense. However, this doesn't necessarily mean the drug is wearing off—rather, your body is adjusting to its presence.
Tolerance to side effects is a well-recognised phenomenon with GLP-1 receptor agonists. The MHRA product information notes that gastrointestinal adverse effects, including nausea and reduced appetite, are most frequent during dose initiation and titration and typically diminish over time as treatment continues. This adaptation doesn't indicate reduced efficacy for glucose control, but it may create the impression that the medication is becoming less effective.
Additionally, lifestyle factors can influence how you perceive Ozempic's effects. Variations in physical activity, stress levels, sleep quality, dietary choices, and hydration throughout the week can all impact appetite, energy levels, and blood glucose control. These external factors may interact with the medication's effects, creating a perception of inconsistency. It's also worth noting that individual pharmacokinetics vary—factors such as injection site, body composition, and metabolic rate can subtly influence how the medication is absorbed and distributed in your body.
If you feel that Ozempic is becoming less effective, the first step is to monitor your blood glucose levels systematically. Keep a detailed record of your readings at different times of day, noting any patterns or trends. This objective data is far more reliable than subjective feelings and will help your healthcare team assess whether there's a genuine reduction in glycaemic control. NICE guidance (NG28) recommends individualised HbA1c targets for people with type 2 diabetes, typically aiming for 48 mmol/mol (6.5%) for those not on medications that cause hypoglycaemia, and 53 mmol/mol (7.0%) for those taking insulin or sulfonylureas.
Review your injection technique with your practice nurse or diabetes specialist nurse. Ensure you're rotating injection sites appropriately, as repeated injections in the same area can cause lipohypertrophy (fatty lumps under the skin), which may affect medication absorption. The injection should be administered subcutaneously (under the skin, not into muscle).
Consider whether lifestyle factors have changed. Weight loss, dietary modifications, increased physical activity, or changes in other medications can all influence diabetes control and may necessitate dose adjustments. Keep a food and activity diary for a week or two to identify any patterns.
If you miss a dose, the MHRA product information advises that you should administer it as soon as possible within 5 days after the missed dose. If more than 5 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. You can change your regular dosing day if necessary, provided at least 3 days have passed since your last dose.
Contact your GP or diabetes care team if you notice:
Consistently elevated blood glucose readings
HbA1c rising above your agreed target
Unexplained weight gain
Return of diabetes symptoms (increased thirst, frequent urination, fatigue)
Severe and persistent abdominal pain (with or without vomiting), which could indicate pancreatitis
Symptoms of gallbladder disease (pain in upper right abdomen, nausea, vomiting)
Signs of dehydration (dizziness, dry mouth, reduced urination)
New or worsening visual symptoms, particularly if you have diabetic retinopathy
Your healthcare provider may consider dose escalation (Ozempic starts at 0.25 mg weekly for 4 weeks as an initiation dose only, then 0.5 mg, with possible increases to 1 mg and 2 mg weekly doses if needed and tolerated) or investigate other factors affecting your diabetes control. If you're also taking insulin or sulfonylureas, dose adjustments of these medications may be needed to reduce the risk of hypoglycaemia. Never adjust your dose without medical supervision.
If you experience side effects, report them to your healthcare professional and consider reporting suspected adverse reactions via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
From a pharmacological perspective, Ozempic does not truly "wear off" during the week when used as prescribed. The medication's extended half-life of approximately one week means that therapeutic concentrations remain relatively stable in your bloodstream throughout the seven-day dosing interval. The MHRA product information and EMA European Public Assessment Report (EPAR) indicate consistent glucose-lowering effects across the entire week, with no significant decline in efficacy between doses.
However, there is no official evidence to suggest that Ozempic's glucose-lowering efficacy diminishes substantially as you approach your next injection day. The medication reaches steady-state concentrations after approximately four to five weeks of regular dosing, creating a stable therapeutic effect.
That said, some patients do report subjective changes in how they feel during the week, particularly regarding appetite suppression and gastrointestinal effects. These symptoms may be more noticeable in the first few days after injection and become less prominent later in the week. This pattern likely reflects your body's adaptation to the medication's presence rather than the drug wearing off. The appetite-suppressing effects, while beneficial for weight management, are not the primary therapeutic target—glucose control is.
If you consistently experience problematic fluctuations in symptoms or glucose control, discuss this with your healthcare provider. Ozempic should be administered once weekly on the same day each week as prescribed, and doses should not be divided. Your healthcare provider may need to optimise your dose or consider additional diabetes medications. The key message is that perceived changes in subjective effects don't necessarily indicate reduced therapeutic efficacy. Regular HbA1c monitoring (typically every 3–6 months) provides the most reliable assessment of long-term glucose control and medication effectiveness.
Remember that Ozempic should be administered according to the prescribed schedule. If you need to change your weekly dosing day, you can do so as long as at least 3 days have passed since your last dose. If you miss a dose, administer it as soon as possible within 5 days; otherwise, skip that dose and resume on your next scheduled day.
Ozempic has a half-life of approximately one week (around 165 hours), which allows it to maintain therapeutic levels in your body throughout the entire seven-day dosing interval. It takes roughly four to five weeks of regular weekly injections to reach steady-state concentrations in the bloodstream.
Increased hunger later in the week likely reflects your body adapting to the medication's presence rather than the drug wearing off. Appetite suppression and gastrointestinal effects are often most noticeable immediately after injection and may feel less intense as the week progresses, but glucose-lowering efficacy remains stable throughout.
If you miss a dose, administer it as soon as possible within 5 days after the missed dose. If more than 5 days have passed, skip the missed dose and administer your next dose on the regularly scheduled day without doubling up.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.