
Concerns about whether Rybelsus causes depression have emerged amongst some patients taking this oral medication for type 2 diabetes. Rybelsus (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist that helps control blood glucose levels by mimicking natural gut hormones. Whilst depression is not listed as an established side effect in UK regulatory guidance, understanding the relationship between diabetes medications and mental wellbeing is important. This article examines the evidence surrounding Rybelsus and mood changes, explores how to recognise mental health concerns, and outlines what steps to take if you experience low mood whilst taking this medication.
Quick Answer: Depression is not listed as an established side effect of Rybelsus in UK regulatory guidance, and a 2024 EMA review found no causal link between GLP-1 receptor agonists and suicidal thoughts.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists. Rybelsus is typically prescribed when diet and exercise alone have not achieved adequate blood glucose control, and it may be used alongside other diabetes medications such as metformin. It is not indicated for type 1 diabetes or diabetic ketoacidosis.
The active ingredient, semaglutide, works by mimicking the action of a naturally occurring hormone called GLP-1. This hormone is released by the gut in response to food intake and has several important effects on glucose metabolism. Semaglutide stimulates insulin secretion from the pancreas when blood glucose levels are elevated, helping to lower blood sugar after meals. It also suppresses the release of glucagon, a hormone that raises blood glucose, and slows gastric emptying, which reduces the rate at which glucose enters the bloodstream.
Additionally, Rybelsus acts on receptors in the brain that regulate appetite, often leading to reduced hunger and food intake. This can result in weight loss, which is beneficial for many people with type 2 diabetes, although it's important to note that Rybelsus is not licensed for weight management.
Rybelsus must be taken once daily on an empty stomach with up to 120ml of water only. The tablet should be swallowed whole (not split or crushed) at least 30 minutes before the first food, drink, or other oral medications of the day. If a dose is missed, the patient should skip that dose and take the next scheduled dose the following day.
Rybelsus is available in three tablet strengths—3 mg, 7 mg, and 14 mg. Treatment begins with 3 mg once daily for 30 days, which is a starter dose to improve tolerability and is not intended for glycaemic control. After 30 days, the dose is increased to 7 mg once daily. If additional glycaemic control is needed after at least another 30 days, the dose may be increased to 14 mg once daily. When used with sulfonylureas or insulin, dose reductions of these medications may be needed to reduce the risk of hypoglycaemia.
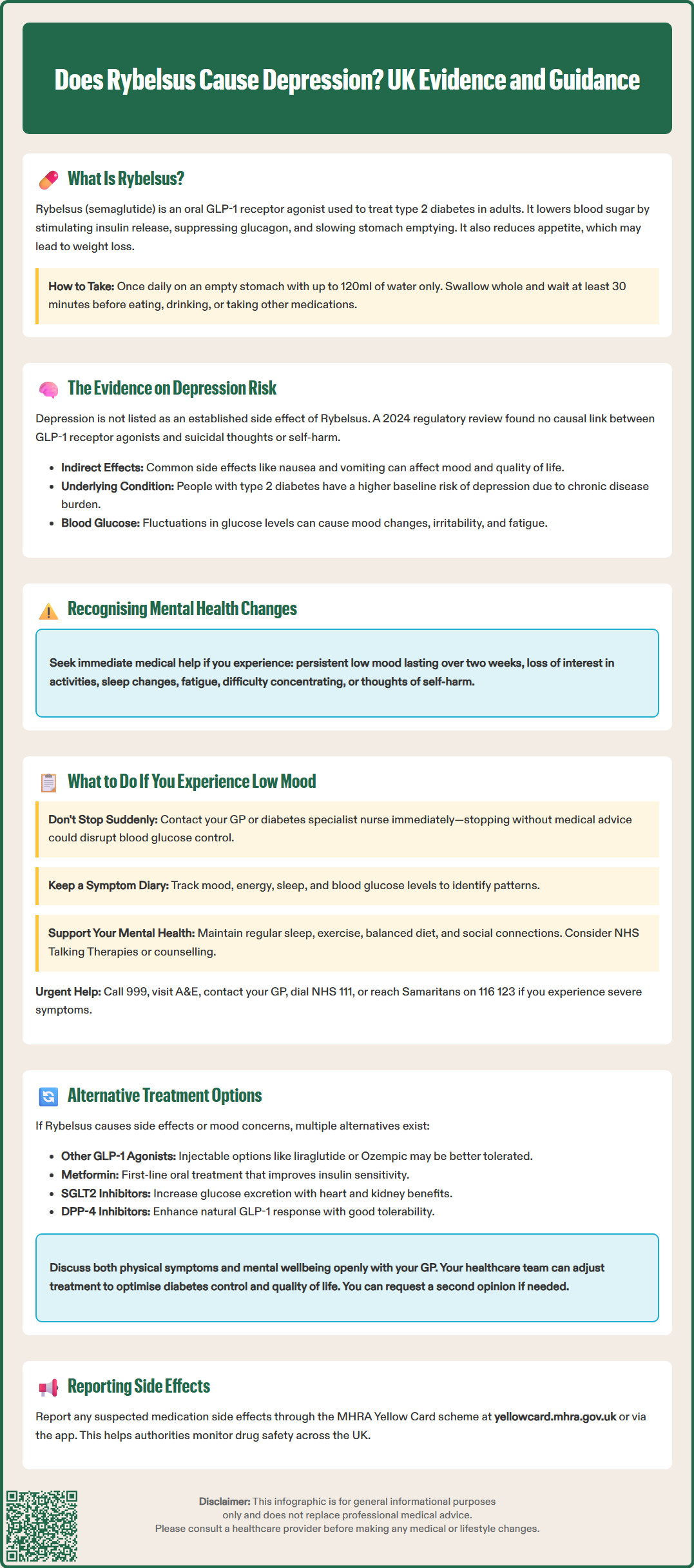
Concerns about whether Rybelsus causes depression have been raised by some patients and healthcare professionals. It is important to note that depression is not listed as a common or established side effect in the official Summary of Product Characteristics (SmPC) for Rybelsus, nor in guidance from the MHRA or European Medicines Agency (EMA). In fact, a 2024 EMA Pharmacovigilance Risk Assessment Committee (PRAC) review concluded that there is no causal association between GLP-1 receptor agonists and suicidal thoughts or self-harm.
Common side effects of Rybelsus include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, abdominal pain, and reduced appetite. These symptoms can be distressing and may indirectly affect mood and quality of life, particularly if they are persistent or severe. Feeling unwell physically can contribute to low mood, irritability, or anxiety, which may be mistaken for depression.
Additionally, people with type 2 diabetes are at higher risk of depression compared to the general population. The burden of managing a chronic condition, concerns about complications, and lifestyle adjustments can all impact mental wellbeing. Therefore, any mood changes experienced while taking Rybelsus may be related to the underlying condition rather than the medication itself.
It's also worth noting that fluctuations in blood glucose levels, including hypoglycaemia and hyperglycaemia, can cause mood changes, irritability, fatigue or confusion. If you experience mood changes, checking your blood glucose levels may help identify if glycaemic variability is contributing to your symptoms.
Signs of depression to be aware of include:
Persistent low mood or sadness lasting more than two weeks
Loss of interest or pleasure in activities you once enjoyed
Changes in sleep patterns (insomnia or excessive sleeping)
Fatigue or loss of energy
Difficulty concentrating or making decisions
Feelings of worthlessness or excessive guilt
Thoughts of self-harm or suicide
If you notice any of these symptoms, it is crucial to speak to your GP or healthcare team promptly. If you experience thoughts of suicide or self-harm, seek immediate help by calling 999, going to A&E, or contacting the Samaritans on 116 123. Early recognition and intervention can significantly improve outcomes.
If you develop low mood, anxiety, or other mental health concerns while taking Rybelsus, it is important not to stop the medication abruptly without medical advice. Sudden discontinuation could affect your blood glucose control and overall diabetes management. Instead, take the following steps:
Contact your GP or diabetes specialist nurse as soon as possible. Describe your symptoms in detail, including when they started, how severe they are, and whether they coincide with starting Rybelsus or increasing the dose. Your healthcare provider will assess whether the symptoms may be related to the medication, your diabetes, or other factors such as life stressors or concurrent health conditions.
Your doctor may recommend a medication review to evaluate whether Rybelsus is the most appropriate treatment for you. If a link between the medication and mood changes is suspected, alternatives can be considered. However, it is equally important to explore other potential causes, such as poorly controlled blood glucose levels, thyroid dysfunction, vitamin deficiencies, or sleep disorders, all of which can affect mood.
Keep a symptom diary noting your mood, energy levels, sleep quality, and any physical symptoms. It's also helpful to check and record your blood glucose levels when experiencing mood changes, as hypo- or hyperglycaemia can affect your mental state. This information can help your healthcare team identify patterns and make informed decisions about your care.
If you experience severe symptoms such as suicidal thoughts, significant changes in behaviour, or an inability to carry out daily activities, seek urgent medical attention. Call 999 or go to A&E if you're at immediate risk, contact your GP immediately, call NHS 111, or contact the Samaritans on 116 123 for 24/7 support. Mental health crises require prompt intervention, and support is available.
In addition to medical management, consider self-care strategies such as maintaining a regular sleep routine, engaging in physical activity, eating a balanced diet, and staying connected with friends and family. Psychological support, such as counselling or cognitive behavioural therapy (CBT), may also be beneficial and can be accessed through your GP, local NHS talking therapies services, or by self-referral to NHS Talking Therapies in England.
If Rybelsus is not suitable for you due to side effects or concerns about mood changes, several alternative treatments for type 2 diabetes are available. Your GP or diabetes specialist will work with you to find the most appropriate option based on your individual circumstances, including your blood glucose control, other health conditions, and personal preferences, in line with NICE guideline NG28 for type 2 diabetes in adults.
Other GLP-1 receptor agonists are available, including injectable formulations such as liraglutide (Victoza), dulaglutide (Trulicity), and once-weekly semaglutide (Ozempic). While these belong to the same drug class as Rybelsus, individual responses can vary, and some people tolerate one formulation better than another.
Alternative oral medications include:
Metformin: the first-line treatment for type 2 diabetes, which improves insulin sensitivity and reduces glucose production by the liver.
SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin): these work by increasing glucose excretion in the urine. Specific agents have evidence-based cardiovascular and renal benefits for certain patient groups as outlined in NICE guidance.
DPP-4 inhibitors (e.g., sitagliptin, linagliptin): these enhance the body's natural GLP-1 response and are generally well tolerated.
Sulphonylureas (e.g., gliclazide): these stimulate insulin release but carry a risk of hypoglycaemia and weight gain, requiring education and monitoring.
Thiazolidinediones (e.g., pioglitazone): these improve insulin sensitivity but have specific contraindications and precautions.
Insulin therapy may be necessary for some individuals, particularly if oral medications are insufficient to achieve target blood glucose levels.
When speaking to your GP, be open and honest about your concerns. Discuss not only your physical symptoms but also your mental wellbeing, as both are integral to your overall health. Your healthcare team is there to support you, and adjustments to your treatment plan can be made to optimise both your diabetes control and quality of life. If you feel your concerns are not being adequately addressed, you have the right to request a second opinion or referral to a specialist diabetes service.
If you suspect you're experiencing side effects from Rybelsus or any medication, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app). This helps authorities monitor medication safety.
Depression is not listed as a common or established side effect in the official UK Summary of Product Characteristics for Rybelsus. A 2024 EMA review concluded there is no causal association between GLP-1 receptor agonists and suicidal thoughts or self-harm.
Contact your GP or diabetes specialist nurse promptly rather than stopping Rybelsus abruptly. Your healthcare provider will assess whether symptoms are related to the medication, your diabetes control, or other factors, and can discuss alternative treatments if needed.
Yes, people with type 2 diabetes are at higher risk of depression compared to the general population. The burden of managing a chronic condition, concerns about complications, and blood glucose fluctuations can all impact mental wellbeing.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.