
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or those who are overweight with weight-related comorbidities. As with any prescription medicine, patients and healthcare professionals may have concerns about potential side effects, including neurological events such as seizures. This article examines the clinical evidence regarding seizure risk with Wegovy, reviews recognised neurological side effects, and provides guidance on safety monitoring in line with UK regulatory standards from the MHRA, NICE, and current pharmacovigilance data.
Quick Answer: There is no established causal link between Wegovy (semaglutide) and seizures based on current clinical trial data and UK post-marketing surveillance.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management but have demonstrated significant efficacy in promoting weight loss.
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. Semaglutide binds to GLP-1 receptors in multiple tissues throughout the body, including the pancreas, gastrointestinal tract, and specific regions of the brain involved in appetite regulation. In the pancreas, it enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, thereby improving glycaemic control. Within the gastrointestinal system, it slows gastric emptying, which prolongs satiety and reduces hunger signals. This reduced gastric emptying is transient and may affect the absorption of some oral medicines, particularly those with a narrow therapeutic index.
Crucially, semaglutide acts on GLP-1 receptors in the hypothalamus and other brain regions that regulate appetite and food intake. By modulating these central pathways, Wegovy reduces appetite, increases feelings of fullness, and helps patients consume fewer calories. The medication is administered once weekly via subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose is gradually increased over 16–20 weeks (starting at 0.25 mg and increasing through 0.5 mg, 1.0 mg, and 1.7 mg to the maintenance dose of 2.4 mg at 4-week intervals) to minimise gastrointestinal side effects and allow the body to adjust to the medication. This titration schedule may be extended if not well tolerated and is essential for tolerability and adherence to treatment.
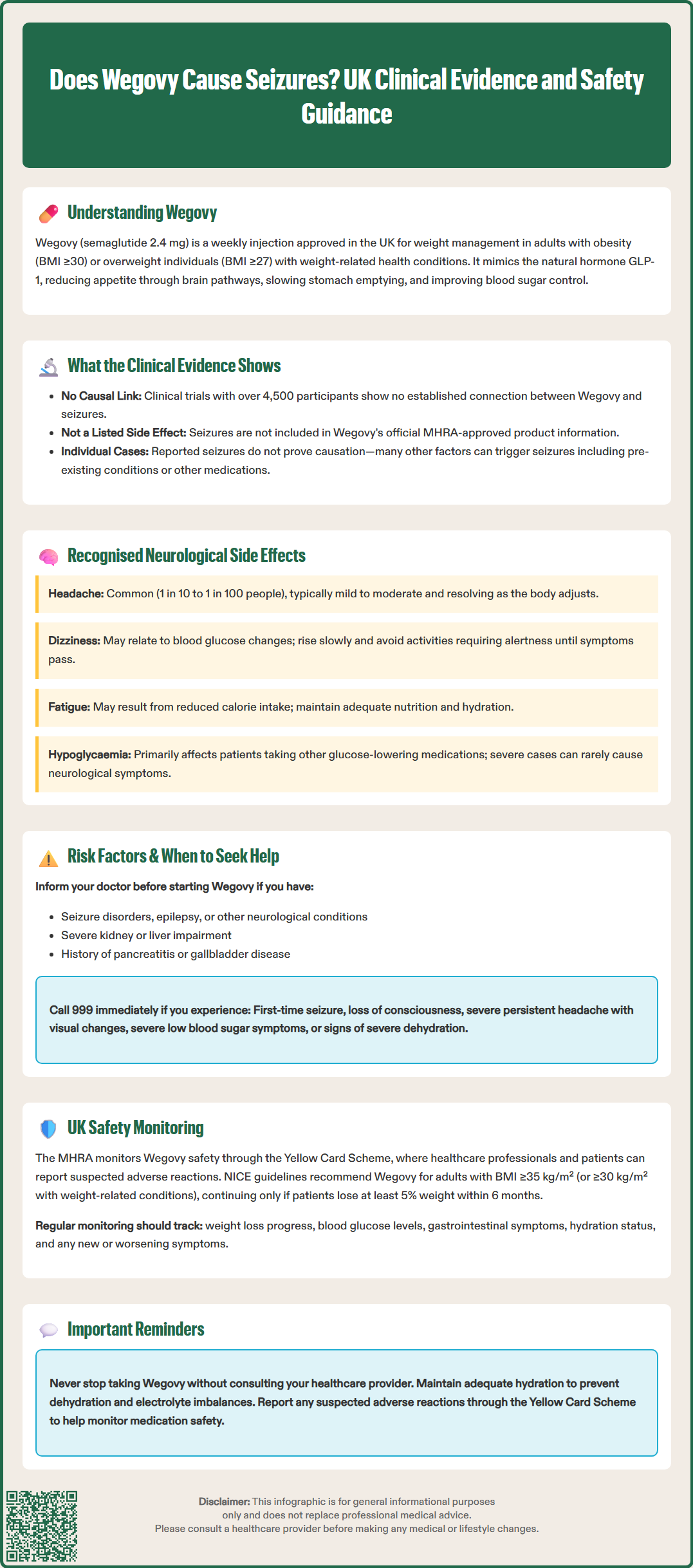
There is currently no established causal link between Wegovy (semaglutide) and seizures based on the available clinical trial data and post-marketing surveillance. Seizures were not identified as a recognised adverse effect in the pivotal STEP (Semaglutide Treatment Effect in People with obesity) clinical trial programme, which enrolled over 4,500 participants and formed the basis for regulatory approval.
The Summary of Product Characteristics (SmPC) for Wegovy, as approved by the Medicines and Healthcare products Regulatory Agency (MHRA), does not list seizures among the known side effects. Post-marketing pharmacovigilance data collected since the medication's approval has not identified a safety signal suggesting an increased risk of seizure activity in patients taking semaglutide for weight management, according to current MHRA safety updates.
However, it is important to recognise that individual case reports may exist where patients experienced seizures whilst taking Wegovy, but this does not necessarily indicate causation. Many factors can contribute to seizure activity, including pre-existing neurological conditions, metabolic disturbances, concurrent medications, or unrelated medical events. The temporal association between starting a medication and experiencing a seizure does not automatically establish a causal relationship.
Healthcare professionals and patients are encouraged to report any suspected adverse drug reactions through the Yellow Card Scheme, which allows the MHRA to continuously monitor the safety profile of all medications, including Wegovy. This ongoing surveillance is essential for detecting rare or previously unrecognised side effects that may not have been apparent during clinical trials. If you experience a seizure whilst taking Wegovy, you should call 999 or attend A&E immediately, especially if it is your first seizure, and inform healthcare providers about all medications you are taking.
Whilst seizures are not recognised as a side effect of Wegovy, the medication does have several documented neurological effects that patients and healthcare professionals should be aware of. According to the MHRA-approved SmPC, headache is a common side effect (affecting between 1 in 10 and 1 in 100 people) during treatment. These headaches are typically mild to moderate in severity and often resolve as the body adjusts to the medication.
Dizziness is another recognised side effect, categorised as common in the SmPC. This may be related to changes in blood glucose levels or could potentially be associated with other effects of the medication. Patients experiencing dizziness should be advised to rise slowly from sitting or lying positions and to avoid activities requiring alertness until symptoms resolve.
Some patients report experiencing fatigue or tiredness, which may be related to the caloric restriction that often accompanies treatment with Wegovy. As patients consume fewer calories due to reduced appetite, they may initially feel less energetic. Ensuring adequate nutrition within the reduced calorie intake and maintaining proper hydration can help mitigate this effect.
It is worth noting that hypoglycaemia (low blood sugar) can occur, though this is primarily a risk in patients taking Wegovy alongside other glucose-lowering medications such as insulin or sulphonylureas. The SmPC advises that doses of these medications may need to be reduced when starting Wegovy. Severe hypoglycaemia can, in rare cases, lead to neurological symptoms including confusion, seizures, or loss of consciousness. Patients with diabetes should work closely with their healthcare team to adjust other medications appropriately when starting Wegovy.
Patients should report any persistent or concerning neurological symptoms to their healthcare provider for appropriate assessment and management.
Certain patient populations may require additional monitoring or caution when using Wegovy, particularly those with pre-existing conditions that could theoretically increase vulnerability to neurological events. Patients with a history of seizure disorders, epilepsy, or other neurological conditions should inform their prescriber before starting treatment, as any new medication may potentially interact with existing conditions or treatments.
Individuals with severe renal or hepatic impairment should be monitored carefully, as altered drug metabolism or excretion could theoretically affect medication levels in the body. Whilst semaglutide is primarily eliminated via protein catabolism rather than renal excretion, significant organ dysfunction warrants closer supervision.
Dehydration represents an important risk factor to consider, as Wegovy commonly causes gastrointestinal side effects including nausea, vomiting, and diarrhoea, particularly during dose escalation. Severe dehydration can lead to electrolyte imbalances, which may lower the seizure threshold in susceptible individuals. Patients should be counselled to maintain adequate fluid intake and to contact their GP if they experience persistent vomiting or diarrhoea.
Seek immediate medical attention (call 999 or go to A&E) if you experience:
A seizure or convulsion for the first time
Loss of consciousness or altered awareness
Severe, persistent headache, especially if accompanied by visual changes, confusion, or neck stiffness
Signs of severe hypoglycaemia (confusion, difficulty speaking, loss of coordination)
Symptoms of severe dehydration (reduced urination, extreme thirst, dizziness, rapid heartbeat)
Contact your GP or healthcare provider if you experience:
New or worsening headaches that don't respond to simple analgesia
Persistent dizziness affecting daily activities
Unusual fatigue or weakness
Any neurological symptoms that concern you
Patients should not discontinue Wegovy without discussing with their healthcare professional, as clinical review is advised when stopping treatment. Any concerns about side effects should be discussed with a healthcare professional rather than stopping treatment independently.
The Medicines and Healthcare products Regulatory Agency (MHRA) maintains ongoing surveillance of Wegovy's safety profile through several mechanisms. The Yellow Card Scheme allows healthcare professionals and patients to report suspected adverse drug reactions directly to the MHRA, contributing to the continuous assessment of medication safety. This pharmacovigilance system is crucial for identifying rare adverse effects that may not have been detected during pre-marketing clinical trials.
NICE Technology Appraisal 875 (TA875) provides recommendations for the use of semaglutide in weight management within the NHS. These guidelines specify that Wegovy should be prescribed as part of a specialist weight management service for adults with a BMI of at least 35 kg/m² (or at least 30 kg/m² with weight-related comorbidities). Treatment should only continue beyond 6 months if patients achieve at least 5% weight loss, ensuring that the medication is providing meaningful benefit. The maximum duration of NHS treatment is 2 years.
Healthcare professionals prescribing Wegovy should conduct a thorough medical history before initiation, including assessment of:
Previous or current neurological conditions
History of pancreatitis or gallbladder disease
Diabetic retinopathy (in patients with diabetes)
Renal function
Concurrent medications that may interact
Regular monitoring during treatment should include:
Assessment of weight loss progress and tolerability
Blood glucose monitoring (particularly in patients with diabetes)
Review of gastrointestinal symptoms and hydration status
Evaluation of any new or worsening symptoms
The European Medicines Agency (EMA) and MHRA require manufacturers to submit periodic safety update reports, which analyse all available safety data from clinical trials, post-marketing surveillance, and published literature. These reports undergo rigorous review by regulatory authorities, who can mandate label changes, additional warnings, or further studies if safety concerns emerge.
Patients should be provided with comprehensive information about Wegovy, including the patient information leaflet, and encouraged to report any unexpected symptoms. Healthcare providers should maintain open communication channels, ensuring patients feel comfortable discussing concerns about their treatment. This collaborative approach to safety monitoring helps ensure that Wegovy is used appropriately and that any potential risks are identified and managed promptly.
No, there is currently no established causal link between Wegovy and seizures based on clinical trial data and UK post-marketing surveillance. Seizures are not listed as a recognised side effect in the MHRA-approved product information.
Common neurological side effects of Wegovy include headache and dizziness. Fatigue may also occur, often related to reduced calorie intake, and hypoglycaemia can cause neurological symptoms in patients taking other glucose-lowering medications.
Call 999 or attend A&E immediately if you experience a first seizure, loss of consciousness, severe persistent headache with visual changes, or signs of severe hypoglycaemia. Contact your GP for persistent headaches, dizziness affecting daily activities, or any concerning neurological symptoms.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.