Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, offering significant glycaemic control and weight reduction. Whilst highly effective, the medication commonly causes gastrointestinal side effects including nausea, diarrhoea, and constipation due to delayed gastric emptying. Many patients explore probiotic supplementation to support digestive health during treatment. This article examines the evidence for probiotic use alongside Mounjaro, identifies beneficial strains for specific symptoms, and provides practical guidance on safe supplementation within the context of UK clinical practice and NICE guidance.
Quick Answer: No single probiotic has been definitively proven superior for Mounjaro users, but multi-strain formulations containing Lactobacillus and Bifidobacterium species may help manage common gastrointestinal side effects such as nausea, diarrhoea, and constipation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. The Medicines and Healthcare products Regulatory Agency (MHRA) approved tirzepatide following clinical trials demonstrating significant improvements in glycaemic control and weight reduction. The medication works by mimicking naturally occurring incretin hormones, which stimulate insulin secretion in response to food intake, suppress glucagon release, and slow gastric emptying.
The mechanism of delayed gastric emptying, whilst therapeutically beneficial for blood glucose management and satiety, frequently produces gastrointestinal adverse effects. According to the UK Summary of Product Characteristics (SmPC), the most common gastrointestinal side effects include nausea (reported in 12-24% of patients), diarrhoea (13-17%), vomiting (6-10%), and constipation (5-6%), with frequencies varying by dose. These symptoms typically diminish over several weeks as physiological adaptation occurs.
The slowed transit of food through the digestive system may alter the gut microbiome composition and function. Some preliminary research suggests that GLP-1 receptor agonists might influence the diversity and abundance of intestinal bacteria, though the clinical significance of these changes remains unproven and under investigation. The gastrointestinal symptoms experienced by many Mounjaro users have prompted interest in complementary strategies to support digestive health, including dietary modifications and probiotic supplementation.
It is important to note that tirzepatide can reduce the exposure of orally administered medications due to delayed gastric emptying. The SmPC advises that women using oral contraceptives should consider additional non-oral contraception for 4 weeks after initiation and each dose increase of Mounjaro.
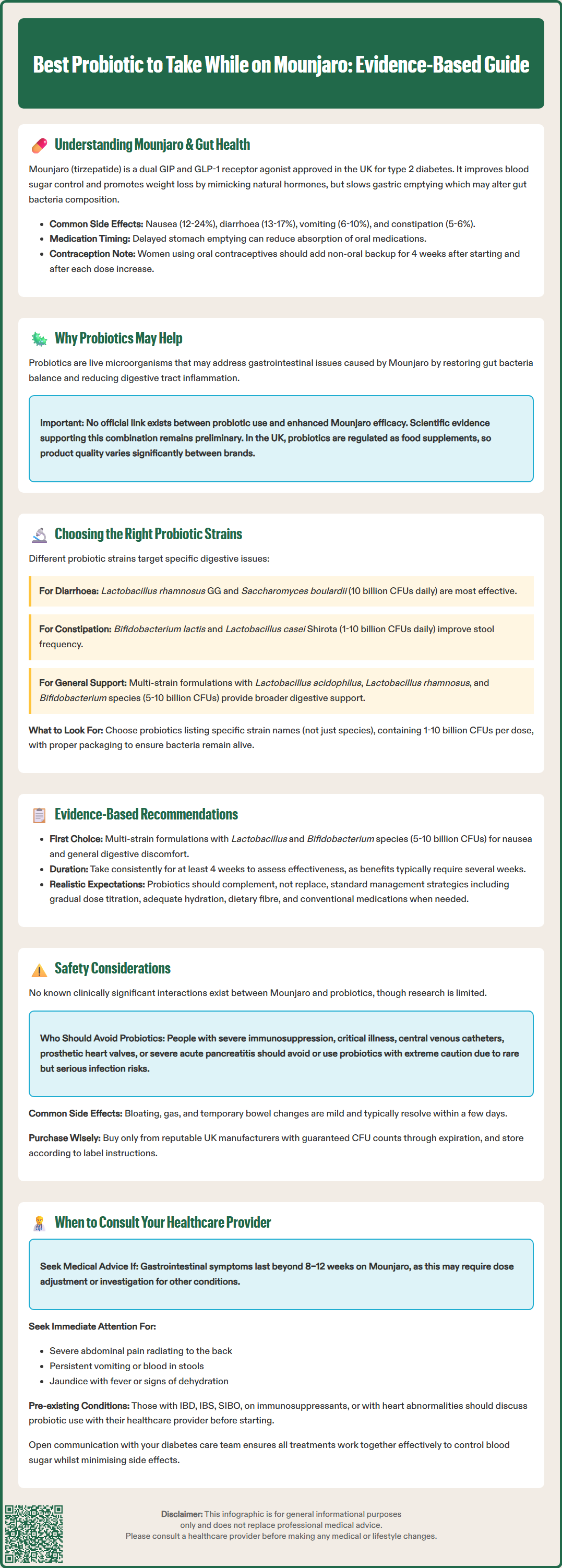
Probiotics are defined by the World Health Organization as live micro-organisms that, when administered in adequate amounts, confer a health benefit on the host. These beneficial bacteria and yeasts may theoretically address several aspects of gastrointestinal function that are affected by Mounjaro therapy. The rationale for probiotic use during GLP-1 receptor agonist treatment centres on their potential to modulate gut microbiota composition, enhance intestinal barrier function, and reduce inflammatory responses within the digestive tract.
Patients experiencing nausea and altered bowel habits whilst taking Mounjaro may find that certain probiotic strains help restore microbial balance and improve digestive comfort. Some evidence suggests that specific probiotics can reduce the severity and duration of diarrhoea, whilst others may alleviate constipation by influencing gut motility and stool consistency. The delayed gastric emptying induced by tirzepatide creates an environment where food remains in the stomach and upper intestine for extended periods, potentially affecting the microbial ecosystem.
Beyond symptomatic relief, probiotics may support the broader metabolic benefits of Mounjaro treatment. Research indicates that gut microbiota play a role in glucose metabolism, insulin sensitivity, and weight regulation—the very parameters that tirzepatide aims to improve. Certain bacterial strains produce short-chain fatty acids (SCFAs) such as butyrate, which serve as energy sources for colonocytes and may enhance metabolic health. However, it is important to note that there is no official link established between probiotic supplementation and enhanced efficacy of Mounjaro, and current evidence remains preliminary.
It should be emphasised that in the UK, probiotics are regulated as food supplements rather than medicines, and product quality and bacterial viability can vary considerably between manufacturers. The decision to use probiotics should focus primarily on managing gastrointestinal symptoms and supporting overall digestive wellness, not on enhancing the medication's efficacy.
Not all probiotics are equivalent, and selecting appropriate strains requires understanding the specific gastrointestinal challenges associated with Mounjaro therapy. The most extensively researched probiotic genera include Lactobacillus, Bifidobacterium, and Saccharomyces, each containing multiple species and strains with distinct properties and evidence bases.
For patients experiencing diarrhoea, Lactobacillus rhamnosus GG and Saccharomyces boulardii have demonstrated efficacy in clinical trials for various forms of diarrhoeal illness, including antibiotic-associated diarrhoea (Cochrane Reviews). These strains may help restore normal bowel function by competing with pathogenic organisms, producing antimicrobial substances, and modulating intestinal immune responses. Saccharomyces boulardii, a beneficial yeast rather than a bacterium, shows particular promise as it is resistant to antibiotics and can survive passage through the acidic stomach environment.
Conversely, individuals struggling with constipation may benefit from Bifidobacterium lactis strains, which have been associated with improved stool frequency and consistency in controlled studies. Lactobacillus casei Shirota has also shown potential for alleviating constipation by influencing gut transit time and stool water content.
For general digestive support and microbiome diversity, multi-strain formulations containing combinations of Lactobacillus and Bifidobacterium species may offer broader benefits. Products containing Lactobacillus acidophilus, Lactobacillus plantarum, Bifidobacterium longum, and Bifidobacterium bifidum are commonly available and generally well-tolerated. When selecting a probiotic, patients should look for products that specify the strain designation (not merely the species), provide colony-forming unit (CFU) counts (typically 1–10 billion CFUs per dose), and demonstrate stability through appropriate packaging and storage conditions as indicated on the product label.
Whilst specific clinical trials examining probiotics in conjunction with Mounjaro or other GLP-1 receptor agonists remain limited, we can extrapolate from broader evidence regarding probiotic use for gastrointestinal symptoms and metabolic health. No single probiotic product has been definitively proven superior for individuals taking tirzepatide, and recommendations must therefore be based on the best available evidence for managing similar digestive complaints.
For nausea and general gastrointestinal discomfort, multi-strain formulations containing Lactobacillus acidophilus, Lactobacillus rhamnosus, and Bifidobacterium species represent a reasonable first-line approach. These combinations have demonstrated safety and tolerability in diverse populations and may support overall digestive function during the adaptation period to Mounjaro. Products should ideally contain at least 5–10 billion CFUs per serving and be taken consistently for a minimum of 4 weeks to assess benefit.
Patients experiencing persistent diarrhoea might consider Saccharomyces boulardii or Lactobacillus rhamnosus GG (at least 10 billion CFUs daily), both of which have robust evidence from Cochrane Reviews for reducing diarrhoeal symptoms in other contexts. For constipation, Bifidobacterium lactis strains at doses of 1–10 billion CFUs daily have shown promise in improving bowel movement frequency. Always follow the manufacturer's recommended dosage instructions on the product label.
It is crucial to emphasise that probiotic supplementation should complement, not replace, other management strategies recommended by NICE guidance (NG28). These include gradual dose titration of Mounjaro as per the SmPC, adequate hydration, dietary fibre optimisation, and appropriate use of conventional anti-emetics or laxatives (such as macrogols for constipation) when clinically indicated. Patients should maintain realistic expectations, as probiotics typically require several weeks of consistent use before benefits become apparent, and individual responses vary considerably.
Probiotics are generally recognised as safe for the majority of individuals, with an excellent safety profile established through decades of use and research. However, certain populations require particular caution, and potential interactions with Mounjaro therapy warrant consideration. No known clinically significant interactions between tirzepatide and probiotic supplements have been reported, though evidence is limited and patients should monitor for any changes in symptoms.
Individuals with severe immunosuppression, critical illness, central venous catheters, or a history of prosthetic heart valves or endocarditis should exercise caution with probiotic use. Rare cases of bacteraemia and fungaemia have been reported in severely immunocompromised patients taking probiotics, though such occurrences remain exceptionally uncommon.
Persons with severe acute pancreatitis should avoid probiotics, as evidence from a randomised controlled trial (Besselink et al., NEJM 2008) suggests potential harm in this specific context. Whilst Mounjaro itself carries a small risk of pancreatitis, there is no evidence that probiotics increase this risk. However, anyone experiencing symptoms suggestive of pancreatitis should seek immediate medical attention and discontinue all non-essential supplements pending clinical assessment.
Patients taking Mounjaro should be aware of other important safety considerations: the risk of hypoglycaemia when combined with insulin or sulfonylureas (requiring glucose monitoring and possible dose adjustments of these medications), and the potential for gallbladder disease (presenting as right upper quadrant pain, fever, or jaundice).
Common adverse effects of probiotics are typically mild and transient, including bloating, flatulence, and temporary changes in bowel habits during the first few days of use. These symptoms usually resolve spontaneously as the gut microbiome adjusts. Patients should ensure they purchase probiotics from reputable UK manufacturers, with CFUs guaranteed to the end of shelf life, and store products strictly according to label instructions. Both refrigerated and shelf-stable formulations can be effective when properly stored.
Patients are advised to report any suspected side effects from Mounjaro or probiotics to the MHRA Yellow Card Scheme.
Whilst probiotics are available without prescription and generally considered safe, certain circumstances warrant professional medical guidance before commencing or continuing supplementation alongside Mounjaro therapy. Patients should consult their GP or diabetes specialist nurse if gastrointestinal symptoms persist beyond 8–12 weeks of Mounjaro treatment, as this may indicate the need for dose adjustment, alternative management strategies, or investigation for other underlying conditions.
Red flag symptoms requiring prompt medical assessment include: severe or worsening abdominal pain (particularly if radiating to the back, which may suggest pancreatitis), persistent vomiting preventing adequate hydration or medication adherence, blood in stools, right upper quadrant pain with fever or jaundice (possible gallbladder disease), unintentional weight loss beyond expected therapeutic effects, or signs of dehydration such as reduced urine output, dizziness, or confusion. For severe symptoms, contact NHS 111 or attend urgent care/A&E as appropriate. These symptoms necessitate clinical evaluation regardless of probiotic use, as they may indicate serious complications requiring specific treatment.
Individuals with pre-existing gastrointestinal conditions such as inflammatory bowel disease (Crohn's disease or ulcerative colitis), irritable bowel syndrome, or small intestinal bacterial overgrowth (SIBO) should discuss probiotic selection with their healthcare provider, as certain strains may be more appropriate than others for specific conditions. Similarly, patients taking immunosuppressive medications, those with a history of recurrent infections, or individuals with structural heart abnormalities should seek medical advice before using probiotics.
Your healthcare team can provide personalised recommendations based on your complete medical history, current medications, and specific symptom profile. They may also suggest alternative or additional interventions, such as dietary referral to a registered dietitian, prescription anti-emetics, or adjustments to your Mounjaro dosing schedule. Maintaining open communication with your diabetes care team ensures that all aspects of your treatment plan work synergistically to achieve optimal glycaemic control whilst minimising adverse effects and supporting your overall wellbeing throughout your therapeutic journey with Mounjaro.
Yes, probiotics are generally safe to take alongside Mounjaro with no known clinically significant interactions. They may help manage common gastrointestinal side effects such as nausea, diarrhoea, and constipation, though individual responses vary.
Lactobacillus rhamnosus GG and Saccharomyces boulardii have the strongest evidence for managing diarrhoea, with recommended doses of at least 10 billion CFUs daily. These strains have demonstrated efficacy in clinical trials for various forms of diarrhoeal illness.
Probiotics typically require a minimum of 4 weeks of consistent use before benefits become apparent. Individual responses vary considerably, and patients should maintain realistic expectations whilst continuing other management strategies recommended by their healthcare provider.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.