GLP-1 receptor agonists, such as semaglutide and liraglutide, are increasingly prescribed for type 2 diabetes and weight management in the UK. Many patients also live with Hashimoto's thyroiditis, an autoimmune condition causing hypothyroidism. Understanding whether GLP-1 meds and Hashimoto's can be safely managed together is essential for informed treatment decisions. This article explores the compatibility of these medications with autoimmune thyroid disease, potential interactions with levothyroxine, monitoring requirements, and when to seek medical advice. Evidence-based guidance helps patients and clinicians navigate this common clinical scenario confidently.
Quick Answer: GLP-1 receptor agonists can generally be used safely in patients with Hashimoto's thyroiditis, with no absolute contraindication, though individualised assessment and thyroid function monitoring are essential.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
GLP-1 medications work through several complementary mechanisms. They stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared with some other diabetes treatments. Simultaneously, these drugs suppress glucagon release, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver.
Beyond glucose control, GLP-1 receptor agonists slow gastric emptying, which prolongs the feeling of fullness after meals and reduces appetite. This mechanism contributes significantly to weight loss, which is why medications such as semaglutide (Ozempic, Wegovy) and liraglutide (Victoza, Saxenda) have gained approval for weight management in addition to diabetes treatment.
Commonly prescribed GLP-1 medications in the UK include semaglutide, dulaglutide (Trulicity), liraglutide, and exenatide (Byetta, Bydureon). These are typically administered via subcutaneous injection, either daily or weekly depending on the specific formulation. Oral semaglutide (Rybelsus) is also available. These medications are licensed in the UK following rigorous clinical trials demonstrating their efficacy and safety profile, though like all medicines, they carry potential adverse effects including nausea, vomiting, diarrhoea, and pancreatitis. Pancreatitis has been reported with GLP-1 medications; patients should seek urgent medical attention if they experience severe, persistent abdominal pain, with or without vomiting.
GLP-1 medications may also increase the risk of gallbladder disease, including gallstones and inflammation of the gallbladder. Patients should be aware of symptoms such as right upper abdominal pain, fever, or yellowing of the skin or eyes, which warrant prompt medical assessment.
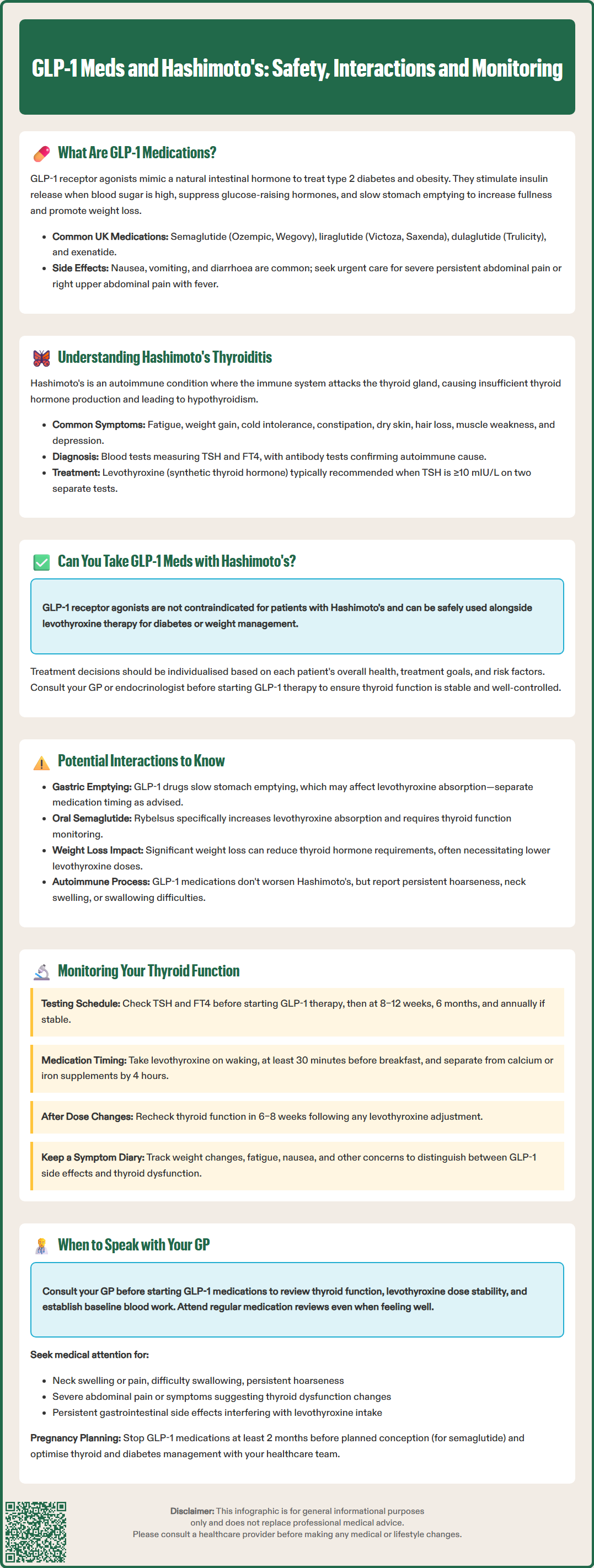
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, is the most common cause of hypothyroidism (underactive thyroid) in the UK and other areas with sufficient iodine intake. This autoimmune condition occurs when the body's immune system mistakenly attacks the thyroid gland, gradually destroying thyroid tissue and impairing its ability to produce thyroid hormones.
The thyroid gland, located in the front of the neck, produces two primary hormones: thyroxine (T4) and triiodothyronine (T3). These hormones regulate metabolism, energy production, body temperature, heart rate, and numerous other physiological processes. In Hashimoto's disease, the immune system produces antibodies—particularly thyroid peroxidase antibodies (TPO) and thyroglobulin antibodies (TG)—that target thyroid tissue, leading to inflammation and progressive damage.
Symptoms of Hashimoto's thyroiditis typically develop gradually and may include fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, muscle weakness, and depression. Some individuals may experience a goitre (enlarged thyroid gland). However, many people remain asymptomatic in the early stages, with the condition detected only through routine blood tests.
Diagnosis involves measuring thyroid-stimulating hormone (TSH) and free thyroxine (FT4) levels. Primary hypothyroidism is confirmed biochemically by elevated TSH with low or normal FT4. Thyroid antibody testing supports an autoimmune aetiology but may be absent in some cases of Hashimoto's thyroiditis. According to NICE guidance (NG145), treatment with levothyroxine is typically recommended when TSH is ≥10 mIU/L on two separate occasions, with individualised decisions for lower TSH levels based on symptoms and risk factors.
Treatment typically involves levothyroxine replacement therapy, which provides synthetic thyroid hormone to restore normal metabolic function. According to NICE guidance, thyroid function should be monitored regularly, particularly when initiating treatment or adjusting doses, to ensure optimal hormone levels and symptom control.
There is no absolute contraindication to using GLP-1 receptor agonists in patients with Hashimoto's thyroiditis. The presence of autoimmune thyroid disease does not automatically preclude treatment with these medications for type 2 diabetes or weight management. Many individuals with both conditions successfully use GLP-1 medications whilst managing their thyroid condition with levothyroxine replacement therapy.
The decision to prescribe GLP-1 medications should be individualised, taking into account the patient's overall health status, treatment goals, concurrent medications, and any additional risk factors. Healthcare professionals will consider whether the benefits of improved glycaemic control or weight loss outweigh potential risks in each specific case.
It is worth noting that weight loss itself—a common effect of GLP-1 medications—may influence thyroid hormone requirements in patients with Hashimoto's disease. As body weight decreases, the dose of levothyroxine often needs to be reduced to maintain optimal thyroid hormone levels. This is because thyroid hormone requirements are partly determined by body mass.
Some specific considerations apply to certain GLP-1 medications. Oral semaglutide (Rybelsus) increases thyroxine exposure, which may affect thyroid function. If these medications are co-prescribed, thyroid function should be monitored, and patients should discuss with their healthcare provider about appropriate timing of each medication.
Patients with Hashimoto's thyroiditis who are considering GLP-1 medications should have a thorough discussion with their GP or endocrinologist. This conversation should cover their current thyroid function status, the stability of their thyroid hormone replacement, and any symptoms they may be experiencing. Well-controlled Hashimoto's disease, with stable thyroid function tests and appropriate levothyroxine dosing, generally poses no barrier to GLP-1 therapy. However, close monitoring during the initial treatment period is advisable to ensure both conditions remain well managed.
Whilst GLP-1 medications can generally be used safely in patients with Hashimoto's thyroiditis, there are several important considerations regarding potential interactions and effects on thyroid function.
Thyroid C-cell tumours have been observed in rodent studies with GLP-1 receptor agonists, though the relevance to humans remains uncertain. The European Medicines Agency's Pharmacovigilance Risk Assessment Committee (PRAC) reviewed this issue in 2023 and did not confirm a causal association between GLP-1 receptor agonists and thyroid cancer in humans. Nevertheless, patients should be advised to report symptoms such as persistent hoarseness, neck swelling, difficulty swallowing, or breathing problems, which warrant prompt medical assessment. UK clinical practice follows the precautions outlined in the Summary of Product Characteristics (SmPC) for each medication.
The pharmacokinetic interaction between GLP-1 medications and levothyroxine warrants attention. Because GLP-1 receptor agonists slow gastric emptying, they may theoretically affect the absorption of oral medications, including levothyroxine. Levothyroxine is typically taken on an empty stomach, at least 30 minutes before food, to optimise absorption. The delayed gastric emptying caused by GLP-1 drugs could potentially alter levothyroxine absorption patterns.
Oral semaglutide (Rybelsus) specifically has a documented interaction with levothyroxine, increasing thyroxine exposure. The SmPC recommends monitoring thyroid function when these medications are co-prescribed. Patients should separate the timing of these medications and follow their healthcare provider's advice on appropriate dosing intervals.
Weight loss induced by GLP-1 medications represents an indirect but clinically relevant interaction. As patients lose weight, their metabolic rate and thyroid hormone requirements may change. Studies have shown that thyroid hormone levels can shift with significant weight changes, often necessitating a reduction in levothyroxine dose. Patients should have thyroid function monitored during substantial weight loss, with dose adjustments based on TSH and FT4 results.
There is no established link between GLP-1 medications and worsening of autoimmune thyroid disease or acceleration of thyroid tissue destruction in Hashimoto's thyroiditis. The autoimmune process underlying Hashimoto's disease operates independently of GLP-1 receptor pathways.
Regular monitoring of thyroid function is essential for patients with Hashimoto's thyroiditis who commence GLP-1 receptor agonist therapy. This surveillance ensures that both conditions remain optimally controlled and allows for timely adjustment of thyroid hormone replacement if needed.
For patients with stable, well-controlled Hashimoto's disease on established levothyroxine therapy, NICE guidance (NG145) typically recommends thyroid function testing annually. However, when initiating GLP-1 medications, more frequent monitoring may be prudent. A reasonable approach includes:
Baseline thyroid function tests (TSH and FT4) before starting GLP-1 therapy
Repeat testing at 8–12 weeks after commencing treatment, particularly if significant weight loss occurs
Further monitoring at 6 months, then annually if thyroid function remains stable
Additional testing if symptoms of thyroid dysfunction develop
After any levothyroxine dose change, NICE NG145 recommends re-checking thyroid function in 6–8 weeks to assess the adequacy of the adjustment.
Symptoms warranting thyroid function assessment include unexplained fatigue, weight changes beyond those expected from GLP-1 therapy, changes in heart rate, mood alterations, temperature intolerance, or changes in bowel habits. These may indicate either under-replacement or over-replacement with levothyroxine.
Patients should be advised to maintain consistent timing of levothyroxine administration—ideally on waking, at least 30 minutes before breakfast—and to take it separately from other medications. Levothyroxine should be separated from calcium or iron supplements by at least 4 hours, as these can impair absorption. If using oral semaglutide (Rybelsus), patients should follow the SmPC recommendations regarding timing and monitor thyroid function if co-prescribed with levothyroxine.
If gastrointestinal side effects from GLP-1 medications are significant, patients should discuss with their GP whether the timing of levothyroxine administration needs adjustment.
Self-monitoring plays an important role. Patients should be encouraged to track symptoms, weight changes, and any new or worsening concerns. Keeping a symptom diary can help healthcare professionals distinguish between side effects of GLP-1 medications (such as nausea or fatigue) and symptoms of thyroid dysfunction. This information proves invaluable during clinical reviews and supports informed decision-making regarding medication adjustments.
Open communication with your GP or specialist is crucial when considering or using GLP-1 medications alongside Hashimoto's thyroiditis. Several specific situations warrant prompt medical consultation.
Before starting GLP-1 therapy, schedule a discussion with your healthcare provider if you have Hashimoto's disease. This consultation should cover your current thyroid function status, levothyroxine dose stability, and any relevant medical history. Your GP will review recent thyroid function tests and may order updated blood work to establish a baseline before commencing treatment.
Contact your GP if you experience:
New or worsening symptoms suggesting thyroid dysfunction, such as extreme fatigue, significant unintended weight changes, palpitations, anxiety, or depression
Persistent gastrointestinal side effects from GLP-1 medications that interfere with taking levothyroxine appropriately
Neck swelling, pain, difficulty swallowing or persistent hoarseness, which could indicate thyroid changes requiring assessment, potentially via urgent suspected cancer pathways if concerning features are present
Symptoms of hypoglycaemia (if you have diabetes), particularly if you take other glucose-lowering medications alongside GLP-1 therapy
Severe, persistent abdominal pain (with or without vomiting), which could indicate pancreatitis requiring urgent medical attention
Right upper abdominal pain, fever, or yellowing of the skin or eyes, which might suggest gallbladder problems, a known risk with GLP-1 medications and rapid weight loss
New or worsening visual symptoms if you have diabetic retinopathy, as rapid improvement in blood glucose can sometimes temporarily worsen retinopathy
Regular medication reviews are essential. Even if you feel well, attend scheduled appointments to monitor thyroid function and assess the effectiveness of both your GLP-1 medication and levothyroxine therapy. These reviews allow for proactive dose adjustments before symptoms develop.
If you are planning pregnancy, discuss this with your healthcare team well in advance. GLP-1 medications are not recommended during pregnancy, and for semaglutide specifically, treatment should be stopped at least 2 months before planned conception due to its long half-life. Both thyroid function and diabetes management require careful optimisation before conception. Your treatment plan will need adjustment to ensure the best outcomes for both you and your baby.
Finally, if you have concerns about medication costs, side effects, or treatment goals, raise these with your GP. Alternative treatment options may be available, and shared decision-making ensures your care plan aligns with your individual circumstances and preferences. Your healthcare team is there to support you in managing both conditions effectively and safely.
If you suspect you have experienced a side effect from your medication, report it to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Yes, there is no absolute contraindication to using GLP-1 receptor agonists with Hashimoto's disease. Many patients successfully use these medications alongside levothyroxine, though individualised assessment and regular thyroid function monitoring are recommended.
Weight loss from GLP-1 therapy may reduce your thyroid hormone requirements, potentially necessitating a lower levothyroxine dose. Thyroid function should be monitored at baseline, 8–12 weeks after starting treatment, and during significant weight changes to ensure optimal dosing.
No GLP-1 medications are specifically contraindicated in Hashimoto's thyroiditis. However, oral semaglutide (Rybelsus) increases thyroxine exposure and requires thyroid function monitoring when used with levothyroxine, with careful attention to timing of administration.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.