Tirzepatide is a once-weekly injectable medication licensed in the UK for treating type 2 diabetes mellitus, marketed as Mounjaro. It represents a significant advancement in metabolic medicine through its unique dual mechanism of action. Unlike earlier treatments that target a single pathway, tirzepatide simultaneously activates both GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) receptors. This innovative dual agonism enhances glycaemic control whilst promoting weight loss. Understanding how tirzepatide works helps patients and clinicians make informed decisions about its role in diabetes management and metabolic health.
Quick Answer: Tirzepatide works by simultaneously activating both GIP and GLP-1 receptors, stimulating glucose-dependent insulin secretion, suppressing glucagon, slowing gastric emptying, and promoting satiety.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is an injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. Marketed under the brand name Mounjaro, tirzepatide represents an important addition to metabolic medicine.
The medication belongs to a class of drugs known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. This dual mechanism distinguishes tirzepatide from earlier GLP-1 receptor agonists such as semaglutide or liraglutide, which target only one receptor pathway.
In the UK, tirzepatide received marketing authorisation from the Medicines and Healthcare products Regulatory Agency (MHRA). For type 2 diabetes, it is indicated as an adjunct to diet and exercise to improve glycaemic control. NICE Technology Appraisal (TA) 870 recommends tirzepatide as an option for treating type 2 diabetes in adults with inadequate glycaemic control, specifically as part of a triple therapy regimen or as a dual therapy with insulin when certain criteria are met.
The medication is administered once weekly via subcutaneous injection, offering convenience compared to daily treatments. Patients should be assessed by a healthcare professional to determine suitability, as tirzepatide is not appropriate for everyone and requires careful monitoring throughout treatment.
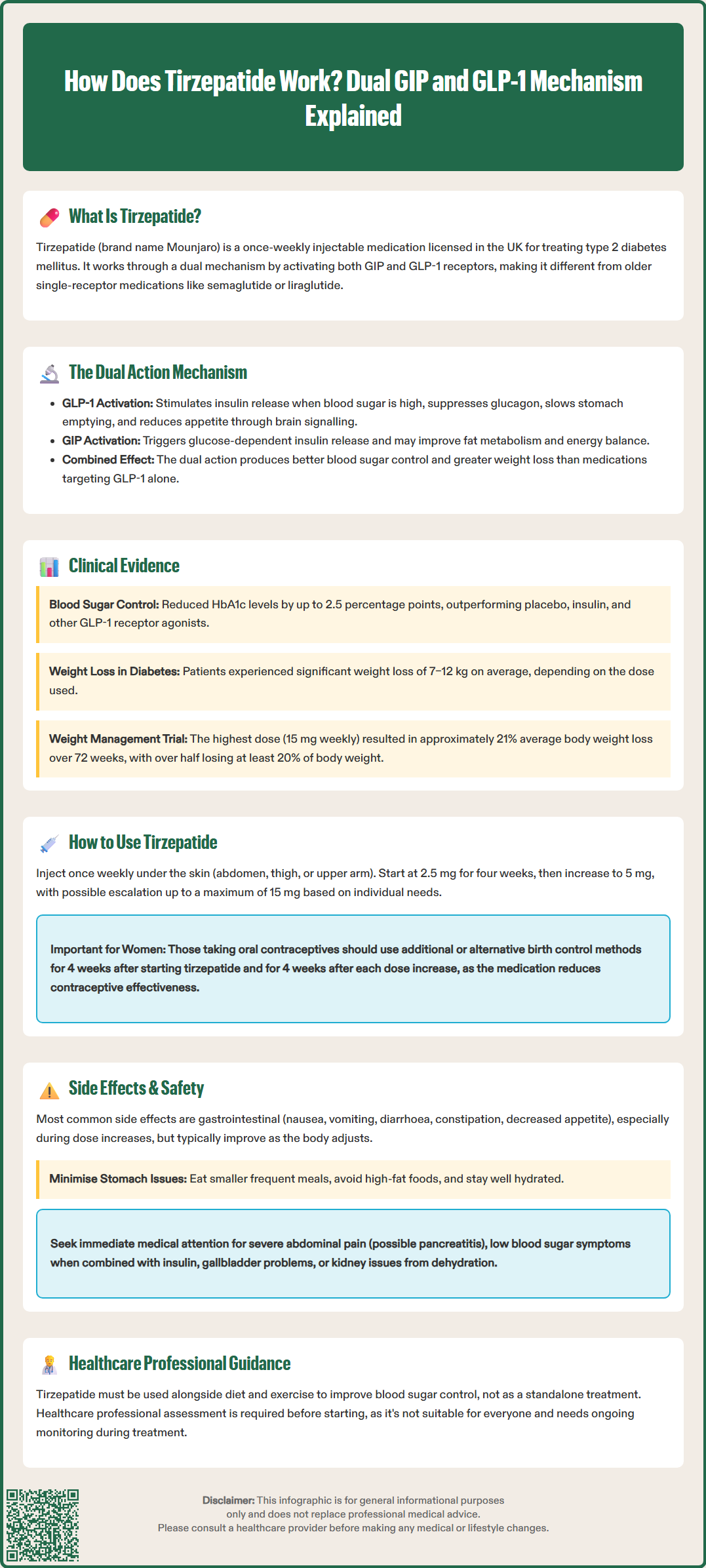
Understanding how tirzepatide works requires knowledge of two key hormones involved in glucose metabolism and appetite regulation: GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1). Both are incretin hormones—naturally occurring substances released by the intestine in response to food intake.
GLP-1 receptor agonism is well established in diabetes management. When tirzepatide activates GLP-1 receptors, it stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. GLP-1 activation also suppresses glucagon secretion (a hormone that raises blood glucose), slows gastric emptying, and promotes satiety by acting on appetite centres in the brain.
GIP receptor agonism adds a complementary dimension. GIP also stimulates insulin secretion in a glucose-dependent fashion and may enhance the effects of GLP-1 on beta-cell function. Based on preclinical and early human data, GIP may also influence fat metabolism and energy homeostasis, potentially contributing to tirzepatide's weight loss effects. The combined action of both pathways appears to result in enhanced glycaemic control and greater weight reduction than seen with GLP-1 agonism alone, as demonstrated in clinical trials.
Tirzepatide is a synthetic peptide engineered to activate both receptor types simultaneously. Its molecular structure includes modifications that extend its half-life, allowing once-weekly dosing. This dual agonism represents an innovative approach in incretin-based therapy, offering metabolic benefits through complementary mechanisms that address multiple aspects of type 2 diabetes pathophysiology.
Tirzepatide's efficacy has been extensively evaluated in the SURPASS clinical trial programme for type 2 diabetes. These large-scale, randomised controlled trials provide robust evidence supporting its therapeutic benefits.
In the SURPASS trials, tirzepatide demonstrated superior HbA1c reduction compared to placebo, insulin, and other GLP-1 receptor agonists including semaglutide 1 mg weekly (SURPASS-2). Patients achieved HbA1c reductions of up to 2.5 percentage points, with a substantial proportion reaching target HbA1c levels below 7% (53 mmol/mol). In the trials, some patients achieved HbA1c below 5.7% (39 mmol/mol), though this is not a routine treatment target in UK clinical practice. These improvements were accompanied by significant weight loss, averaging 7–12 kg depending on the dose, which is clinically meaningful for cardiovascular and metabolic health.
The SURMOUNT-1 trial specifically examined tirzepatide for weight management in adults without diabetes. Participants receiving the highest dose (15 mg weekly) achieved an average weight loss of approximately 20.9% of baseline body weight over 72 weeks—substantially greater than placebo. More than half of participants lost at least 20% of their body weight, a threshold associated with improvements in obesity-related comorbidities such as hypertension, dyslipidaemia, and obstructive sleep apnoea.
Regarding cardiovascular outcomes, tirzepatide has shown favourable effects on cardiovascular risk factors including blood pressure and lipid profiles. Dedicated cardiovascular outcome trials are ongoing to assess effects on major adverse cardiovascular events. NICE has evaluated tirzepatide's cost-effectiveness and clinical positioning within UK treatment pathways for type 2 diabetes. While results are impressive, it is important to note that individual responses vary, and tirzepatide is most effective when combined with lifestyle modifications including dietary changes and regular physical activity.
Tirzepatide is administered as a subcutaneous injection once weekly, on the same day each week, at any time of day, with or without food. It is supplied in pre-filled, single-dose pens designed for self-administration, similar to insulin pens. Patients should receive proper training from a healthcare professional before starting treatment.
Dosing schedule follows a gradual escalation to minimise gastrointestinal side effects:
Starting dose: 2.5 mg once weekly for four weeks
Maintenance dose: Increase to 5 mg once weekly after the initial four weeks
Dose escalation: If additional glycaemic control or weight loss is needed, the dose may be increased in 2.5 mg increments at four-week intervals
Maximum dose: 15 mg once weekly
The injection should be administered subcutaneously in the abdomen, thigh, or upper arm, rotating injection sites to reduce the risk of lipodystrophy. Patients should inspect the solution before use—it should be clear and colourless to slightly yellow. If the solution appears cloudy, discoloured, or contains particles, it should not be used.
Important administration considerations:
If a dose is missed, it should be administered as soon as possible within four days. If more than four days have passed, skip the missed dose and resume the regular schedule.
Tirzepatide pens should be stored in a refrigerator (2–8°C), protected from light, and should not be frozen. Once in use, pens may be kept at room temperature (up to 30°C) for up to 21 days, protected from direct heat and sunlight.
Needles must be removed after each injection and disposed of safely in a sharps container.
No dose adjustment is required for patients with renal or hepatic impairment, though monitoring is advised if significant gastrointestinal adverse effects occur.
Importantly, tirzepatide can reduce the exposure to oral contraceptives. Women using oral contraceptives should consider using a non-oral or additional barrier method for 4 weeks after initiation and for 4 weeks after each dose increase.
Patients should be counselled on recognising and managing side effects, and advised to contact their GP or diabetes specialist nurse if they experience persistent symptoms or have concerns about their treatment.
Like all medications, tirzepatide can cause side effects, though not everyone experiences them. The most common adverse effects are gastrointestinal, particularly during dose escalation, and typically diminish over time as the body adjusts.
Common side effects (affecting more than 1 in 10 people) include:
Nausea and vomiting: Often most pronounced in the first few weeks
Diarrhoea or constipation: Gastrointestinal motility changes are expected
Decreased appetite: This contributes to weight loss but may be uncomfortable
Abdominal pain or discomfort
Injection site reactions: Redness, itching, or swelling at the injection site
To minimise gastrointestinal symptoms, patients should eat smaller, more frequent meals, avoid high-fat foods, and stay well hydrated. If symptoms are severe or persistent, dose escalation may need to be delayed, or the dose reduced temporarily.
Serious but less common side effects require immediate medical attention:
Pancreatitis: Severe, persistent abdominal pain radiating to the back, often accompanied by vomiting, warrants urgent assessment. Tirzepatide should be discontinued if pancreatitis is suspected.
Hypoglycaemia: Risk is increased when tirzepatide is used with insulin or sulfonylureas. Patients should recognise symptoms (tremor, sweating, confusion, palpitations) and know how to treat low blood sugar.
Gallbladder problems: Rapid weight loss increases the risk of gallstones. Symptoms include severe upper abdominal pain, fever, and jaundice.
Acute kidney injury: Dehydration from vomiting or diarrhoea can impair kidney function, particularly in patients with pre-existing renal impairment.
Allergic reactions: Severe reactions including anaphylaxis are rare but possible.
Special warnings and precautions:
Hypersensitivity to tirzepatide is a contraindication. Tirzepatide should not be used in type 1 diabetes or diabetic ketoacidosis.
Tirzepatide should be used with caution in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, due to thyroid C-cell tumour findings in animal studies (though there is no established link in humans).
Patients with diabetic retinopathy should be monitored for worsening of retinopathy, particularly during rapid improvement in glycaemic control.
Tirzepatide is not recommended during pregnancy; women of childbearing potential should use effective contraception and discontinue tirzepatide at least one month before a planned pregnancy. As noted previously, women using oral contraceptives should consider additional contraceptive measures during dose initiation and escalation.
Regular monitoring of HbA1c, weight, and renal function is recommended. Patients should attend scheduled follow-up appointments and report any concerning symptoms promptly to their healthcare team. The decision to continue tirzepatide should be reviewed periodically, considering efficacy, tolerability, and individual treatment goals.
Patients and healthcare professionals are encouraged to report suspected adverse reactions via the Yellow Card Scheme at yellowcard.mhra.gov.uk.
Tirzepatide is the first medication to activate both GIP and GLP-1 receptors simultaneously, whereas earlier treatments like semaglutide target only GLP-1. This dual mechanism provides enhanced glycaemic control and greater weight reduction through complementary pathways affecting insulin secretion, glucagon suppression, gastric emptying, and appetite regulation.
Tirzepatide begins lowering blood glucose levels within days of the first injection, though optimal glycaemic control develops gradually over several weeks as the dose is escalated. Maximum therapeutic effects on HbA1c are typically observed after 3–6 months of treatment at the maintenance dose.
Tirzepatide has a low risk of causing hypoglycaemia when used alone because it stimulates insulin secretion only when blood glucose is elevated (glucose-dependent mechanism). However, the risk increases significantly when tirzepatide is combined with insulin or sulfonylureas, requiring dose adjustments of these medications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.