LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many people prescribed Wegovy (semaglutide 2.4 mg) for weight management wonder why they're not seeing expected results. Whilst clinical trials show significant weight loss for most patients, individual responses vary considerably. Several factors can influence Wegovy's effectiveness, including treatment duration, dosing, lifestyle modifications, medication interactions, and underlying medical conditions. Understanding these variables is essential for optimising outcomes. This article explores common reasons why Wegovy may not be working as anticipated and provides guidance on when to seek medical advice and what alternative options exist within UK weight management services.
Quick Answer: Wegovy may not work effectively due to insufficient treatment duration, inadequate dosing, lifestyle factors, medication interactions, or individual biological variation.
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. The medication works by mimicking the natural hormone GLP-1, which regulates appetite and food intake through several mechanisms.
Semaglutide acts on receptors in the brain's appetite centres, particularly the hypothalamus, to reduce hunger and increase feelings of fullness. It also slows gastric emptying, meaning food remains in the stomach longer, contributing to prolonged satiety. Additionally, Wegovy may influence the reward pathways in the brain that govern food cravings and eating behaviour.
Expected weight loss outcomes vary considerably between individuals. Clinical trials (STEP 1-4) demonstrated that participants without diabetes lost an average of 15% of their initial body weight over 68 weeks when combining Wegovy with lifestyle modifications. For people with type 2 diabetes, weight loss was lower at approximately 9-10% (STEP 2). However, these represent averages—some people lose significantly more, whilst others experience more modest results. NICE guidance (TA875) emphasises that weight loss medications should be used alongside reduced-calorie diets and increased physical activity, not as standalone treatments.
It's important to understand that Wegovy is not a quick fix. Weight loss typically occurs gradually, with most significant changes appearing after 3–6 months of treatment. The medication requires dose escalation over 16 weeks (0.25 mg → 0.5 mg → 1.0 mg → 1.7 mg → 2.4 mg at 4-weekly increments) to reach the full maintenance dose of 2.4 mg weekly, though escalation can be delayed if needed for tolerability. If 2.4 mg is not tolerated, 1.7 mg may be used as a maintenance dose. Initial weight loss may be slower than anticipated, so setting realistic expectations is crucial—if you're not seeing dramatic changes in the first few weeks, this doesn't necessarily indicate treatment failure.
Several factors can influence individual response to Wegovy, and understanding these can help identify why the medication may not be producing expected results. Insufficient treatment duration is perhaps the most common reason for perceived lack of efficacy. Many patients expect rapid weight loss, but semaglutide's full effects typically manifest after reaching the maintenance dose and continuing treatment for several months.
Inadequate dosing can significantly impact outcomes. The dose escalation schedule exists to minimise gastrointestinal side effects, but some patients may remain on lower doses longer than recommended due to tolerability issues. Staying at 0.5 mg or 1 mg weekly when 2.4 mg is the target therapeutic dose will naturally produce less pronounced weight loss, though some patients may still benefit from the 1.7 mg maintenance dose if the full 2.4 mg is not tolerated.
Individual biological variation plays a substantial role in medication response. Genetic factors, hormonal differences, metabolic rate, and underlying medical conditions all influence how your body responds to GLP-1 receptor agonists. Some people are naturally less responsive to this class of medication, though this represents a minority of patients.
Previous weight loss history may also affect outcomes. Individuals who have undergone multiple cycles of weight loss and regain may experience adaptive metabolic changes that could make subsequent weight loss more challenging, though individual responses vary. Similarly, those with long-standing obesity may experience slower progress than those with more recent weight gain.
Medication adherence is critical—missing doses or inconsistent administration can substantially reduce effectiveness. Wegovy must be administered weekly on the same day to maintain stable drug levels and optimal appetite suppression. If you miss a dose, take it as soon as possible within 5 days of the scheduled dose. If more than 5 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day.
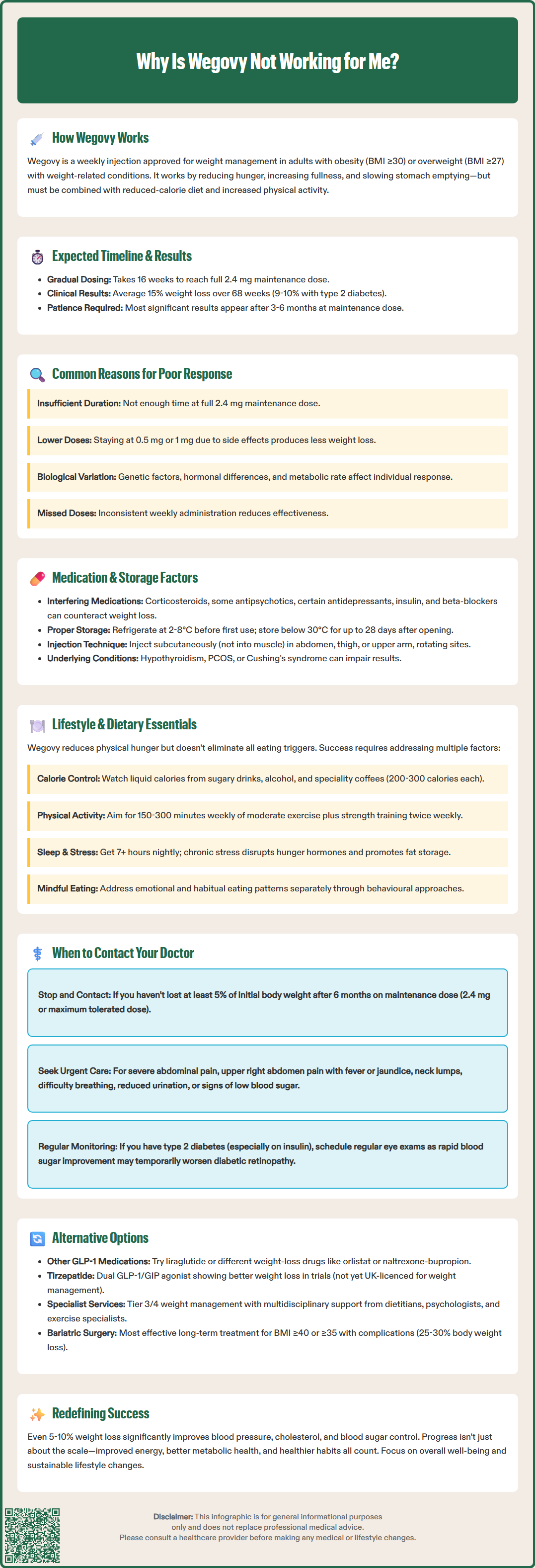
Several pharmaceutical and physiological factors can interfere with Wegovy's efficacy. Drug interactions are relatively uncommon with semaglutide, but certain medications can indirectly affect weight loss outcomes. Corticosteroids (such as prednisolone), some antipsychotics (including olanzapine and quetiapine), certain antidepressants (particularly mirtazapine and some tricyclics), and mood stabilisers like valproate are associated with weight gain and may counteract Wegovy's effects.
Insulin and sulfonylureas used for diabetes management can promote weight gain, potentially offsetting some of semaglutide's benefits. If you're taking these medications alongside Wegovy, discuss with your healthcare provider whether adjustments might be appropriate. Some beta-blockers, commonly prescribed for hypertension and heart conditions, may contribute to weight gain or make weight loss more difficult in some individuals, though this effect varies between different agents and patients.
Wegovy's delayed gastric emptying effect may impact the absorption of oral medicines, particularly those with a narrow therapeutic index. If you're taking warfarin or other coumarin anticoagulants, more frequent INR monitoring may be needed when starting or adjusting Wegovy.
Injection technique and storage can affect drug stability and absorption. Wegovy must be stored according to the specific instructions in the Patient Information Leaflet. Before first use, store in a refrigerator (2-8°C). After first use, the pen can be stored below 30°C or in a refrigerator for up to 28 days. Exposure to heat or freezing can denature the protein, rendering it less effective. Ensure you're injecting subcutaneously (under the skin, not into muscle) in recommended sites—abdomen, thigh, or upper arm—and rotating injection sites to prevent lipohypertrophy (fatty lumps) that can impair absorption.
Underlying medical conditions may influence treatment response. Hypothyroidism, polycystic ovary syndrome (PCOS), Cushing's syndrome, and other endocrine disorders can make weight loss more challenging. If you have such conditions, ensure they're optimally managed. While antibodies to semaglutide can theoretically develop, the EMA's assessment report indicates this is rare and clinically significant antibody formation is uncommon with current formulations.
Wegovy's effectiveness is substantially enhanced when combined with appropriate lifestyle modifications—the medication is licensed specifically as an adjunct to diet and exercise, not as monotherapy. Caloric intake remains fundamental to weight loss. Whilst Wegovy reduces appetite, it's still possible to consume excess calories, particularly through calorie-dense foods or beverages. Some patients find that whilst they eat less volume, they may unconsciously choose higher-calorie options, negating the medication's benefits.
Liquid calories are a common pitfall. Sugary drinks, fruit juices, alcohol, and high-calorie coffees can contribute substantial energy intake without triggering the same satiety signals as solid food. Many patients report that they may still consume liquid calories even when feeling less hungry for solid foods. A single large latte or glass of wine can contain 200–300 calories, easily undermining a caloric deficit.
Physical activity levels significantly influence weight loss outcomes. The UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity weekly, with evidence suggesting that up to 300 minutes weekly may be beneficial for weight loss. Additionally, muscle-strengthening activities on at least two days per week are recommended. Exercise not only burns calories but also helps preserve lean muscle mass during weight loss, maintains metabolic rate, and improves insulin sensitivity. Sedentary behaviour, even with reduced caloric intake, typically results in slower weight loss and greater loss of muscle tissue relative to fat.
Sleep quality and stress management are often overlooked factors. Poor sleep (less than 7 hours nightly) disrupts hunger hormones, increasing ghrelin (which stimulates appetite) and decreasing leptin (which signals fullness). Chronic stress elevates cortisol, which promotes abdominal fat storage and can drive emotional eating.
Mindful eating practices—eating slowly, without distractions, and recognising true hunger versus emotional or habitual eating—can maximise Wegovy's appetite-suppressing effects. Some patients report that whilst Wegovy reduces physical hunger, psychological or emotional eating patterns persist and require separate attention, potentially through cognitive behavioural approaches.
Practical strategies for managing gastrointestinal side effects include eating smaller, more frequent meals, avoiding high-fat or spicy foods, stopping eating when comfortably full, and ensuring adequate hydration.
Regular monitoring is essential when using Wegovy, and certain situations warrant prompt discussion with your GP or prescribing clinician. According to the Wegovy SmPC, treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 6 months on the maintenance dose (2.4 mg or 1.7 mg if the higher dose is not tolerated).
Contact your healthcare provider if you experience persistent or severe side effects that prevent dose escalation or regular use. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which typically improve over time. However, if these symptoms are intolerable or preventing you from reaching therapeutic doses, your clinician may suggest management strategies or slower titration schedules.
People with type 2 diabetes, particularly those on insulin, should be aware that rapid improvement in glucose control may be associated with temporary worsening of diabetic retinopathy. Regular eye monitoring is recommended, especially during the initial period of treatment.
Warning signs requiring urgent medical attention include:
Severe, persistent abdominal pain (potentially indicating pancreatitis)
Signs of gallbladder problems (pain in the upper right abdomen, fever, yellowing of skin or eyes)
New lump or swelling in the neck, hoarseness, or difficulty swallowing
Severe allergic reactions (rash, difficulty breathing, swelling of face or throat)
Signs of kidney problems (reduced urination, swelling in legs, unusual fatigue)
Symptoms of hypoglycaemia if taking other diabetes medications (shakiness, confusion, rapid heartbeat)
Discuss with your healthcare provider if you're taking new medications that might interact with Wegovy or affect weight loss. Similarly, if you've been diagnosed with new medical conditions or if existing conditions have changed, these may impact treatment efficacy. If you're planning pregnancy, Wegovy should be discontinued at least 2 months before conception, as safety data in pregnancy are limited.
You can report suspected side effects to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk or search for 'MHRA Yellow Card' in the Google Play or Apple App Store.
Your prescriber can help you reassess your weight management strategy and explore whether continuing, adjusting, or changing treatment is most appropriate for your individual circumstances.
If Wegovy isn't producing satisfactory results after adequate trial duration (typically 6 months at maintenance dose), several alternative approaches exist. Other GLP-1 receptor agonists may be considered, though cross-reactivity is possible—if you don't respond to semaglutide, response to liraglutide (Saxenda) may also be limited. However, individual variation means some patients respond better to one agent than another. Note that Wegovy should not be used concomitantly with other GLP-1 receptor agonists.
Combination pharmacotherapy represents an emerging approach. Tirzepatide, a dual GLP-1 and GIP receptor agonist, has shown superior weight loss compared to semaglutide in clinical trials but is not currently licensed in the UK for weight management (as of publication date). Other weight management medications licensed in the UK include orlistat (which reduces fat absorption) and naltrexone-bupropion combination (which acts on appetite and reward pathways). These work through different mechanisms and might be effective when GLP-1 agonists are not.
Specialist weight management services (Tier 3/4) can provide comprehensive, multidisciplinary support. These services typically include dietitians, psychologists, exercise specialists, and physicians who can address the complex factors contributing to obesity. NICE guidance (TA875) specifies that Wegovy should be prescribed within specialist weight management services. Referral criteria vary by local Integrated Care System (ICS), but most accept patients with BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities who haven't achieved adequate weight loss with standard approaches.
Bariatric surgery remains the most effective long-term treatment for severe obesity. NICE guidance (CG189) recommends considering surgery for adults with BMI ≥40 kg/m² or ≥35 kg/m² with obesity-related conditions when non-surgical measures have been unsuccessful. Lower BMI thresholds (≥30 kg/m²) apply for people with recent-onset type 2 diabetes, and BMI thresholds should be adjusted for people from certain ethnic backgrounds. Procedures such as gastric bypass or sleeve gastrectomy typically produce 25–30% total body weight loss and can lead to remission of type 2 diabetes and other conditions.
Reassessing fundamentals is always worthwhile. Working with a registered dietitian to accurately assess caloric intake (many people significantly underestimate consumption), engaging with structured exercise programmes, and addressing psychological factors through counselling or cognitive behavioural therapy can enhance outcomes. Remember that even modest weight loss (5–10% of body weight) produces significant health benefits, including improved blood pressure, cholesterol, blood glucose control, and reduced cardiovascular risk—outcomes that matter regardless of whether you've reached your ideal weight goal.
Wegovy typically requires 3–6 months to show significant weight loss effects, as it takes 16 weeks to reach the full maintenance dose of 2.4 mg weekly. Treatment efficacy is assessed after 6 months on the maintenance dose, with discontinuation recommended if less than 5% initial body weight is lost.
Yes, certain medications can reduce Wegovy's effectiveness, including corticosteroids, some antipsychotics (olanzapine, quetiapine), specific antidepressants (mirtazapine, tricyclics), insulin, sulfonylureas, and some beta-blockers. Discuss all medications with your prescriber to optimise weight loss outcomes.
Consult your healthcare provider to review dosing, lifestyle modifications, potential medication interactions, and underlying medical conditions. If you've been on the maintenance dose for 6 months without losing at least 5% of initial body weight, alternative treatments or referral to specialist weight management services may be appropriate.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.