How long does a GLP-1 injection last in your system? The duration varies significantly depending on which medication you use. GLP-1 receptor agonists are injectable treatments for type 2 diabetes and obesity, available in both daily and weekly formulations. Short-acting options like exenatide (Byetta) clear within 24 hours, whilst long-acting versions such as semaglutide (Ozempic, Wegovy) remain active for approximately one week per dose and may be detectable for 5–6 weeks after stopping. Understanding your medication's duration helps you manage dosing schedules, missed doses, and what to expect if treatment changes. This guide explains the pharmacokinetics of different GLP-1 injections and factors affecting how long they work.
Quick Answer: GLP-1 injections last between 24 hours and one week per dose depending on the formulation, with short-acting versions like exenatide clearing within a day and long-acting options like semaglutide remaining therapeutically active for approximately seven days.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
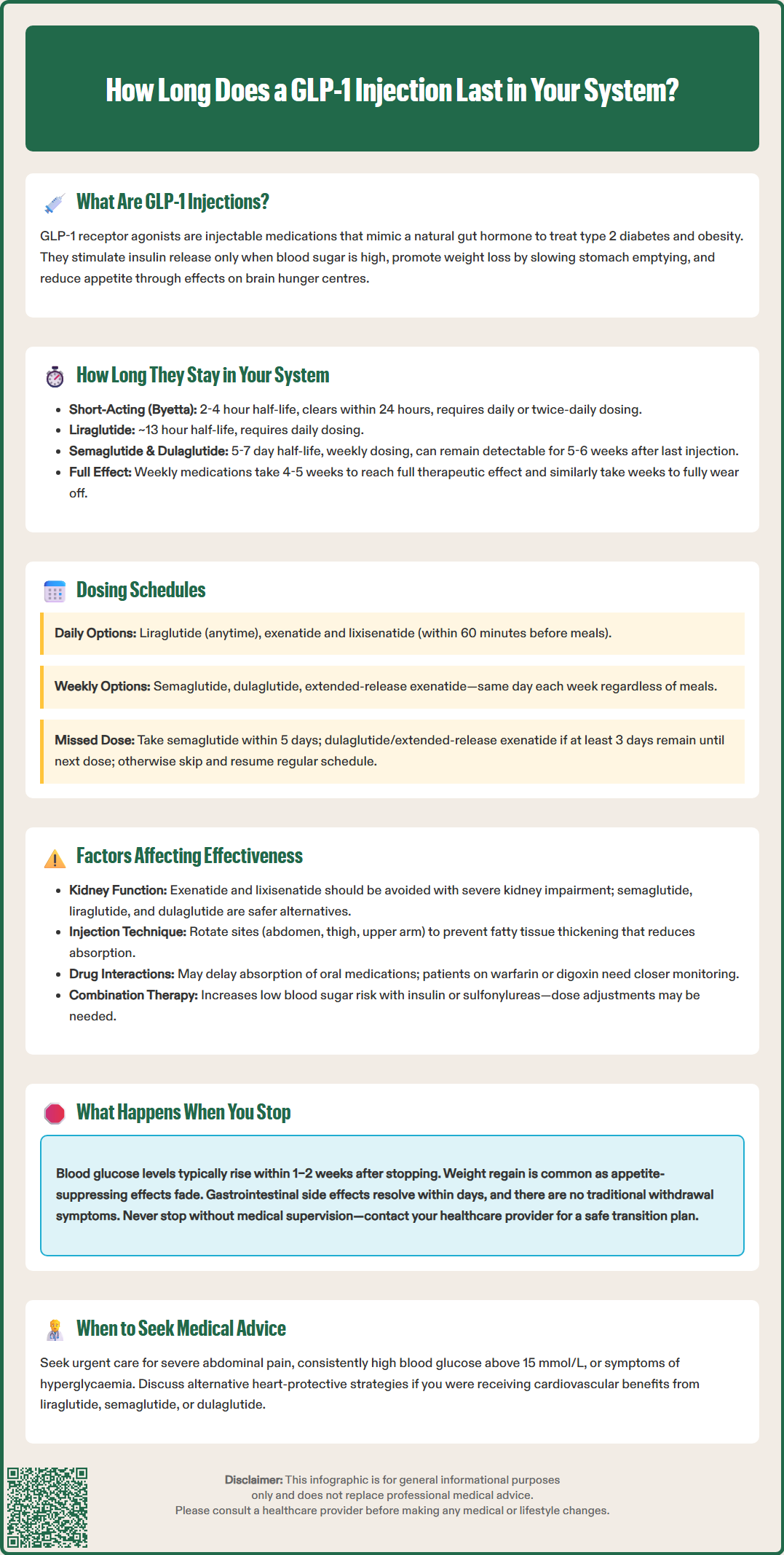
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications primarily used to manage type 2 diabetes mellitus and, in some formulations, obesity. These medicines mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestine following food intake. GLP-1 receptor agonists approved for use in the UK include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), exenatide (Byetta, Bydureon), and lixisenatide (Lyxumia).
The mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which stimulates glucose-dependent insulin secretion. This means insulin is released only when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia compared with some other diabetes medications. Additionally, GLP-1 receptor agonists suppress glucagon secretion from pancreatic alpha cells, further helping to lower blood glucose levels.
Beyond glycaemic control, these medications slow gastric emptying, which prolongs the sensation of fullness after eating and contributes to weight loss. They also act on appetite centres in the brain, reducing hunger and food intake. Cardiovascular benefits have been demonstrated in clinical trials for specific GLP-1 receptor agonists, with liraglutide, semaglutide, and dulaglutide showing reductions in major adverse cardiovascular events in patients with established cardiovascular disease or high cardiovascular risk.
The National Institute for Health and Care Excellence (NICE) recommends GLP-1 receptor agonists for adults with type 2 diabetes when metformin and other oral therapies have not achieved adequate glycaemic control. NICE guidance (NG28) specifies that these agents should generally be considered in people with a BMI ≥30 kg/m² (or lower in certain ethnic groups) and specific problems associated with high weight, or if insulin would have significant occupational implications. Treatment should only be continued if there is a beneficial metabolic response (reduction of at least 11 mmol/mol [1%] in HbA1c and weight loss of at least 3% of initial body weight at 6 months).
For weight management, NICE has approved liraglutide 3 mg (Saxenda) and semaglutide 2.4 mg (Wegovy) under specific criteria, including BMI thresholds and provision through specialist weight management services.
It is important to note that GLP-1 receptor agonists are not indicated for type 1 diabetes. When used with insulin or sulfonylureas, they may increase the risk of hypoglycaemia, and dose adjustments of these medications may be necessary.
These medications are administered via subcutaneous injection, typically in the abdomen, thigh, or upper arm.
The duration that a GLP-1 injection remains active in your system depends primarily on the specific medication and its pharmacokinetic properties. GLP-1 receptor agonists are designed with varying half-lives, which determine how long the drug remains therapeutically active in the body.
Short-acting formulations such as exenatide (Byetta) and lixisenatide (Lyxumia) have half-lives of approximately 2–4 hours. These medications are typically administered once or twice daily and are largely eliminated from the system within 24 hours. Despite their shorter duration, they provide effective glucose control around mealtimes by slowing gastric emptying and reducing post-prandial glucose excursions.
Long-acting formulations have been engineered for extended duration of action. Liraglutide (Victoza) has a half-life of approximately 13 hours, allowing for once-daily dosing. Semaglutide (Ozempic, Wegovy) has a half-life of approximately 7 days (approximately 165 hours), whilst dulaglutide (Trulicity) has a similar half-life of around 5 days. Extended-release exenatide (Bydureon) uses a microsphere depot formulation that provides sustained release over time, allowing for weekly dosing despite different pharmacokinetics from other weekly agents.
It is important to understand that the half-life indicates the time taken for the drug concentration to reduce by half. After approximately five half-lives, a medication is considered largely eliminated from the body. For semaglutide, this means the drug may remain detectable in your system for approximately 5–6 weeks after the final injection, though therapeutic effects diminish sooner.
Weekly GLP-1 receptor agonists typically reach steady-state concentrations after 4–5 weeks of regular dosing. This means that both the onset of full effect when starting treatment and the waning of effect when stopping treatment may take several weeks.
The Medicines and Healthcare products Regulatory Agency (MHRA) provides detailed pharmacokinetic information in the Summary of Product Characteristics for each GLP-1 receptor agonist, which healthcare professionals use to guide prescribing decisions.
GLP-1 receptor agonists are available in both daily and weekly formulations, each offering distinct advantages depending on patient preference, lifestyle, and clinical circumstances.
Daily GLP-1 injections include liraglutide (Victoza, Saxenda), exenatide immediate-release (Byetta), and lixisenatide (Lyxumia). Liraglutide can be administered at any time of day, independent of meals, as long as the timing is consistent. In contrast, exenatide immediate-release and lixisenatide should be administered before meals (within 60 minutes before the main meals of the day). Daily dosing allows for flexible dose adjustments. Some patients prefer daily injections as they feel more in control of their treatment regimen. However, adherence can be challenging for individuals who struggle with daily medication routines.
Weekly GLP-1 injections include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and extended-release exenatide (Bydureon). These formulations are administered once weekly on the same day each week, regardless of meals. The primary advantage is improved convenience and potentially better adherence, as patients only need to remember one injection per week. Clinical studies have shown that weekly formulations achieve comparable or superior glycaemic control and weight loss compared with daily options.
If you miss a dose of a weekly GLP-1 medication, specific guidance varies by product. For semaglutide, administer the missed dose as soon as possible within 5 days after the missed dose. For dulaglutide and extended-release exenatide, administer the missed dose if there are at least 3 days (72 hours) until the next scheduled dose. If outside these windows, wait until the next regularly scheduled dose.
NICE guidance does not mandate preference for daily versus weekly formulations but recommends individualising treatment choice based on patient factors including:
Lifestyle and convenience: Weekly injections may suit busy schedules
Tolerability: Some patients experience fewer gastrointestinal side effects with certain formulations
Clinical efficacy: Specific medications may provide better glucose control or weight loss for individual patients
Cost-effectiveness: NHS formularies may influence availability
Your GP or diabetes specialist nurse will discuss which dosing schedule best suits your circumstances, taking into account your treatment goals and personal preferences.
Several physiological and clinical factors influence the duration and effectiveness of GLP-1 receptor agonists in individual patients.
Renal function affects drug clearance differently depending on the specific GLP-1 receptor agonist. Exenatide and lixisenatide are primarily eliminated through the kidneys and are not recommended in severe renal impairment (eGFR <30 ml/min/1.73m²). In contrast, semaglutide, liraglutide, and dulaglutide undergo proteolytic degradation with minimal renal clearance, making them suitable options for patients with renal impairment, though caution is still advised. The MHRA recommends monitoring renal function in patients taking these medications, particularly if they experience dehydration from gastrointestinal side effects.
Body weight and composition can influence drug distribution and pharmacokinetics. Higher body weight may affect the volume of distribution, though standard dosing protocols generally account for this variation. Clinical trials have demonstrated efficacy across diverse body mass index (BMI) ranges.
Injection technique and site impact absorption rates. Subcutaneous injections should be administered correctly, rotating injection sites to prevent lipohypertrophy (thickening of fatty tissue), which can impair drug absorption. All approved injection sites (abdomen, thigh, and upper arm) provide appropriate absorption when used correctly.
Drug interactions are relatively uncommon with GLP-1 receptor agonists, but their effect on gastric emptying can delay the absorption of oral medications. For medicines with a narrow therapeutic index (e.g., warfarin, digoxin), additional monitoring may be appropriate when starting or stopping GLP-1 therapy. Patients taking warfarin should have more frequent INR monitoring when initiating GLP-1 therapy.
Antibody formation occurs in some patients, particularly with exenatide, though this rarely has clinical significance. If glycaemic control deteriorates despite good adherence, your clinician may investigate alternative causes including antibody development.
Concomitant medications can affect overall glucose control. When GLP-1 receptor agonists are used with insulin or sulfonylureas, the risk of hypoglycaemia increases, and dose reductions of these medications may be necessary.
Adherence to dosing schedule is crucial. Missing doses or inconsistent timing can result in suboptimal glucose control and reduced therapeutic benefit. Following the specific missed-dose guidance for your medication is important for maintaining consistent blood glucose levels.
Discontinuing GLP-1 receptor agonist therapy leads to gradual loss of therapeutic effects as the medication is eliminated from your system. Understanding what to expect can help you make informed decisions about your treatment.
Glycaemic control typically begins to deteriorate within days to weeks after stopping, depending on the medication's half-life. For weekly formulations like semaglutide, glucose levels may remain relatively stable for 1–2 weeks before rising. Blood glucose monitoring becomes particularly important during this period, and your healthcare team may need to adjust other diabetes medications to maintain control.
Weight regain is commonly observed after discontinuation. Clinical studies, including the STEP 1 extension trial with semaglutide 2.4 mg, have shown that patients often regain a significant proportion of weight lost during GLP-1 therapy, typically over several months. This occurs because the appetite-suppressing effects diminish as the drug clears from your system. Maintaining dietary modifications and physical activity established during treatment can help mitigate weight regain.
Gastrointestinal symptoms such as nausea, which some patients experience during treatment, typically resolve within days of stopping. However, there is no evidence of withdrawal symptoms in the traditional sense when discontinuing GLP-1 receptor agonists.
Cardiovascular considerations are important for patients who were receiving cardiovascular benefits from their GLP-1 therapy (particularly liraglutide, semaglutide, or dulaglutide). Discuss alternative cardioprotective strategies with your GP if discontinuing treatment.
When to contact your healthcare professional:
Seek medical advice if you experience significantly elevated blood glucose readings (consistently above 15 mmol/L) or symptoms of hyperglycaemia (excessive thirst, frequent urination, fatigue)
Seek urgent medical attention for severe, persistent abdominal pain (with or without vomiting) which could indicate pancreatitis, or symptoms of gallbladder disease (right upper abdominal pain, fever, jaundice)
Contact your GP if you are considering stopping your medication
Never discontinue prescribed diabetes treatment without medical supervision. Your healthcare team can provide a structured plan for safely transitioning to alternative therapies if GLP-1 treatment is no longer appropriate, including adjustments to any insulin or sulfonylurea doses to prevent hypoglycaemia.
If you experience any suspected side effects from GLP-1 receptor agonists, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Semaglutide has a half-life of approximately 7 days, meaning it may remain detectable in your system for 5–6 weeks after your final injection. However, therapeutic effects begin to diminish sooner, with blood glucose levels typically rising within 1–2 weeks of discontinuation.
Yes, switching between daily and weekly GLP-1 formulations is possible under medical supervision. Your GP or diabetes specialist will provide guidance on timing the transition and monitoring your blood glucose levels during the changeover period to ensure continued glycaemic control.
For semaglutide, administer the missed dose within 5 days of when it was due. For dulaglutide and extended-release exenatide, take the missed dose if there are at least 3 days (72 hours) until your next scheduled injection. If outside these windows, skip the missed dose and resume your regular schedule.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.