Understanding how to measure and administer your GLP-1 receptor agonist correctly is essential for safe and effective diabetes management. The volume in millilitres (mL) is not the same as your prescribed dose strength, which is measured in milligrams (mg) or micrograms (mcg). GLP-1 medications come in pre-filled pens with specific concentrations, and you should never need to calculate mL equivalents yourself. Your healthcare provider prescribes a specific dose strength, which you select using your pen's dose counter or receive via a fixed-dose pen. This article explains GLP-1 dosing, how to administer your injection correctly, and when dose adjustments occur, helping you follow your treatment plan safely whilst achieving optimal glycaemic control.
Quick Answer: You should not measure GLP-1 in mL yourself; instead, follow your prescribed dose strength (mg or mcg) using your pen's dose selector or fixed-dose pen as instructed by your healthcare provider.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWhen prescribed a glucagon-like peptide-1 (GLP-1) receptor agonist, understanding the difference between millilitres (mL) and dose strength is essential for safe medication administration. The volume in mL is not the same as the actual dose of medication you receive. GLP-1 medications come in pre-filled pens or autoinjectors with specific concentrations, meaning the amount of active drug per mL varies between products and formulations.
The important thing to understand is that the dose strength (measured in milligrams or micrograms) represents the actual amount of active medication, which is what your prescriber considers when determining your treatment plan. The mL measurement simply indicates the volume of liquid containing that dose, and this varies between different products and pen strengths.
GLP-1 pens come in different designs. Many are dose-selector devices, where you dial the prescribed dose (e.g., 0.25 mg, 0.5 mg, 1 mg), while others are single-dose fixed-strength pens that deliver a pre-set amount of medication. In either case, you should never need to measure millilitres yourself.
It is crucial never to convert doses between different GLP-1 products or attempt to calculate mL equivalents yourself, as concentrations vary significantly. Always follow your healthcare provider's specific instructions and the Patient Information Leaflet (PIL) regarding which medication you've been prescribed and the dose strength to administer. If you're uncertain about your dosing, contact your GP surgery or diabetes specialist nurse before taking your injection. Incorrect dosing can lead to inadequate glycaemic control or increased risk of adverse effects.
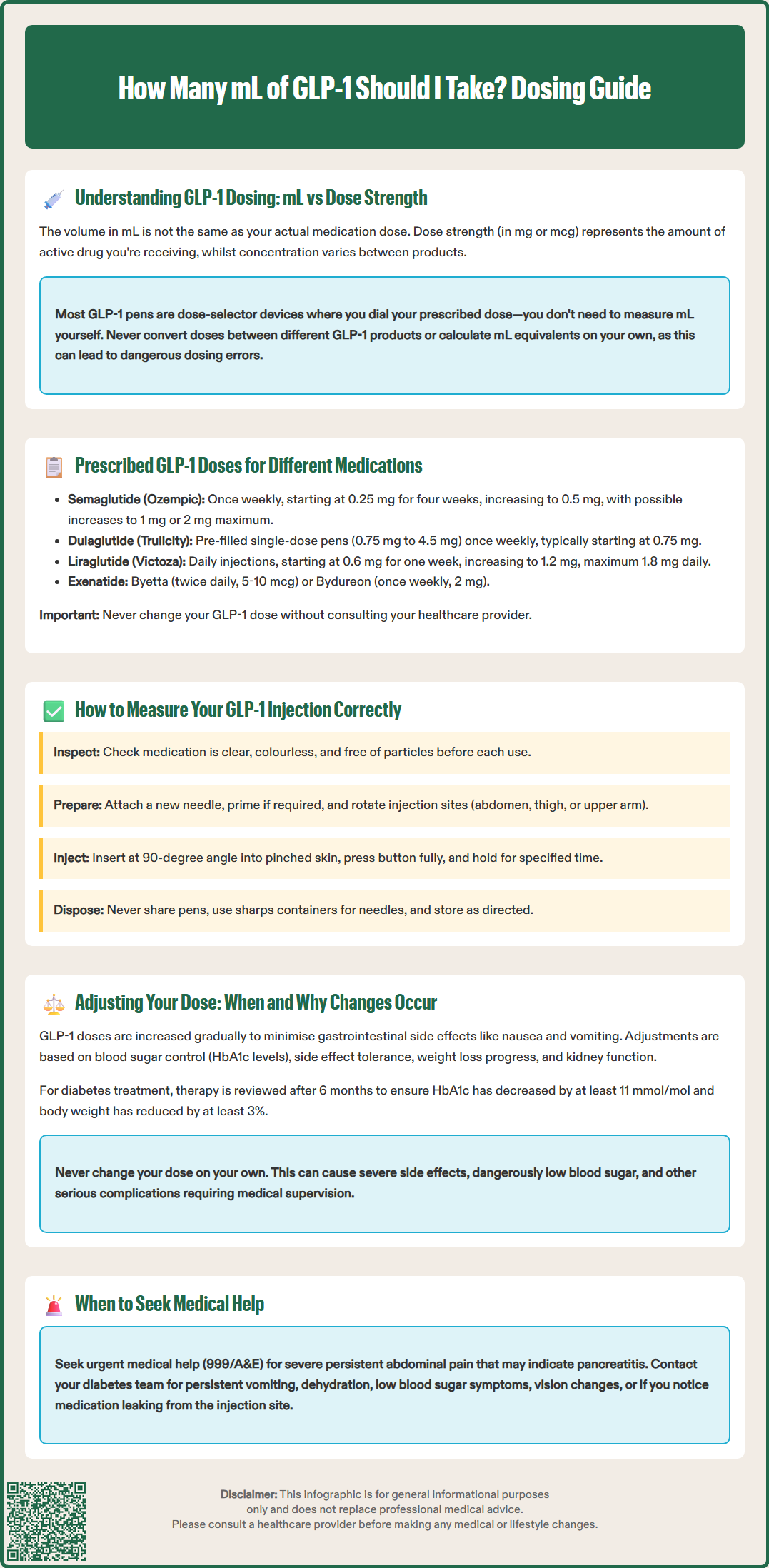
GLP-1 receptor agonists available in the UK include several medications, each with distinct dosing schedules and strengths. Semaglutide (Ozempic) for type 2 diabetes typically starts at 0.25 mg once weekly for four weeks, then increases to 0.5 mg weekly. If additional glycaemic control is needed, the dose may be increased to 1 mg weekly after at least four weeks, with a maximum dose of 2 mg weekly available for some patients. For pens with dose selectors, you select the appropriate number on the dose counter.
Dulaglutide (Trulicity) comes in single-dose pens containing 0.75 mg, 1.5 mg, 3 mg or 4.5 mg, administered once weekly. The starting dose is usually 0.75 mg, which may be increased to 1.5 mg after at least four weeks if required for adequate glucose control. Higher strengths (3 mg and 4.5 mg) are available for patients requiring intensification.
Liraglutide (Victoza) is administered daily, starting at 0.6 mg for one week, then increasing to 1.2 mg. If further glycaemic improvement is needed after at least one week, the dose can be increased to the maximum of 1.8 mg daily. This medication requires daily injections, unlike the weekly alternatives.
Exenatide is available in two formulations: immediate-release (Byetta), given twice daily starting at 5 mcg and potentially increasing to 10 mcg, and extended-release (Bydureon), administered as 2 mg once weekly. Exenatide is not recommended for patients with severe renal impairment (eGFR <30 mL/min/1.73 m²).
NICE guidance (NG28) recommends GLP-1 therapy for type 2 diabetes when metformin and other oral medications haven't achieved adequate control, typically in combination with insulin or as an alternative to insulin in specific circumstances. NICE criteria include BMI considerations and specific treatment contexts. Your prescribed dose depends on multiple factors including your current HbA1c, body weight, renal function, other medications, and treatment goals. Never adjust your dose without consulting your healthcare provider, as changes should be made systematically with appropriate monitoring.
Administering your GLP-1 injection correctly ensures you receive the prescribed dose safely and effectively. GLP-1 pens are designed for ease of use, with many having built-in dose selectors while others are single-use fixed-dose pens. Before each injection, inspect your pen to ensure the medication appears clear and colourless (or as described in your Patient Information Leaflet), with no particles or discolouration.
To prepare your injection:
Check your specific pen instructions in the Patient Information Leaflet (PIL)
Attach a new pen needle for each injection, following the manufacturer's instructions
Prime the pen if required by your specific product (usually for the first use or if the pen hasn't been used recently) by following the PIL instructions
For dose-selector pens, select your prescribed dose by turning the dose selector until the correct number appears in the window
Choose an injection site on your abdomen, thigh, or upper arm (some injections in the upper arm may require assistance), rotating sites to prevent lipohypertrophy
During injection, insert the needle at a 90-degree angle into pinched skin (or as instructed), press the injection button fully, and hold for the time recommended in your PIL (this varies by product). For dose-selector pens, you should see the dose counter return to zero, confirming the full dose has been administered.
Important safety points:
Never share your pen with anyone else, even if you change the needle
Always use a new needle for each injection
Dispose of used needles in a proper sharps container
Store your medication according to the PIL (usually refrigerated before first use, with specific in-use storage times)
Follow product-specific instructions for missed doses
If you notice medication leaking from the injection site or have any concerns about your injection technique, contact your diabetes specialist nurse for guidance. Do not attempt to re-inject or adjust the dose yourself. Your healthcare team can provide hands-on training to ensure proper technique, and many surgeries offer injection technique reviews as part of routine diabetes care.
GLP-1 dose adjustments follow a structured approach based on clinical response, tolerability, and treatment goals. Dose escalation typically occurs gradually to minimise gastrointestinal adverse effects, which are the most common side effects of GLP-1 therapy. These include nausea, vomiting, diarrhoea, and reduced appetite, which usually improve as your body adjusts to the medication.
Your healthcare provider will consider several factors when adjusting your dose:
Glycaemic control: HbA1c levels and blood glucose monitoring results determine whether your current dose is achieving target glucose levels
Tolerability: Persistent or severe gastrointestinal symptoms may require slower dose escalation or remaining at a lower dose
Weight response: For medications prescribed for weight management, weight loss trajectory influences dosing decisions
Renal function: Dose adjustments may be necessary if kidney function changes; exenatide is not recommended in severe renal impairment (eGFR <30 mL/min/1.73 m²)
For type 2 diabetes management, NICE (NG28) recommends reviewing GLP-1 therapy after 6 months, assessing both HbA1c reduction (at least 11 mmol/mol decrease) and weight loss (at least 3% body weight reduction) to determine whether to continue treatment. If targets aren't met, your clinician may increase the dose (if not already at maximum), add additional glucose-lowering medications, or consider alternative therapies.
Never adjust your GLP-1 dose independently. Increasing your dose without medical supervision can lead to severe gastrointestinal effects, hypoglycaemia (particularly if you're taking other diabetes medications), and other adverse reactions. For patients using semaglutide, rapid improvements in blood glucose can sometimes worsen diabetic retinopathy; report any new or worsening visual symptoms promptly.
Contact your GP or diabetes team if you experience:
Persistent severe nausea or vomiting preventing adequate fluid intake
Severe, persistent abdominal pain (with or without vomiting), which could indicate pancreatitis – seek urgent medical help (999/A&E) for this symptom
Signs of severe dehydration – also requiring urgent medical attention
Symptoms of hypoglycaemia
Concerns about medication effectiveness
If you experience any suspected side effects, you can report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). Your healthcare team will schedule regular reviews to monitor your response and make evidence-based decisions about dose optimisation, ensuring you receive maximum benefit whilst minimising risks.
No, you do not measure mL yourself. GLP-1 pens have dose selectors where you dial your prescribed dose strength (e.g., 0.5 mg) or are fixed-dose pens that deliver a pre-set amount automatically.
Dose strength (mg or mcg) is the actual amount of active medication prescribed by your doctor, whilst mL is the liquid volume containing that dose. Concentrations vary between products, so you should always follow your prescribed dose strength, not mL measurements.
Contact your GP or diabetes team if you experience persistent severe nausea or vomiting, severe abdominal pain, signs of dehydration, hypoglycaemia symptoms, or have concerns about medication effectiveness. Never adjust your dose independently.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.