
Tracking your progress on GLP-1 receptor agonist therapy is essential for ensuring treatment effectiveness and safety. Whether you're using semaglutide (Wegovy, Ozempic), liraglutide (Saxenda, Victoza), or dulaglutide (Trulicity) for type 2 diabetes or weight management, systematic monitoring helps you and your healthcare team assess therapeutic response, identify adverse effects early, and make informed decisions about continuing treatment. NICE guidance recommends structured follow-up with specific continuation criteria that must be met. This article explains which metrics to monitor, how to track them effectively, and which tools can support your journey on GLP-1 therapy.
Quick Answer: Track GLP-1 progress by monitoring body weight weekly, recording HbA1c every 3–6 months, documenting side effects systematically, and using apps or journals to maintain comprehensive records for healthcare consultations.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 receptor agonists (GLP-1 RAs) represent a significant advancement in the management of type 2 diabetes and, more recently, weight management. These medications work by mimicking the action of the naturally occurring GLP-1 hormone, which enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety. For weight management, semaglutide 2.4 mg (Wegovy) and liraglutide 3 mg (Saxenda) are specifically licensed in the UK, while medications such as semaglutide (Ozempic), liraglutide (Victoza), and dulaglutide (Trulicity) are approved for type 2 diabetes. Importantly, all GLP-1 RAs should be used as an adjunct to diet and physical activity interventions.
Systematic tracking of your treatment progress is essential to ensure the medication is working effectively and safely. Regular monitoring allows both you and your healthcare team to assess therapeutic response, identify potential adverse effects early, and make informed decisions about dose adjustments or continuation of therapy. NICE guidance (NG28) recommends structured follow-up for patients on GLP-1 therapy, with specific continuation criteria that must be met to justify ongoing treatment.
Moreover, tracking progress provides valuable motivation and accountability. Seeing measurable improvements in weight, blood glucose control, or other health markers can reinforce positive lifestyle changes and adherence to treatment. Conversely, if progress plateaus or adverse effects become problematic, documented records enable timely intervention. The process of tracking itself often increases patient engagement with their health, leading to better overall outcomes. For those prescribed GLP-1 medications through the NHS or private services, maintaining comprehensive records ensures continuity of care and facilitates meaningful consultations with your GP, diabetes specialist nurse, or endocrinologist.
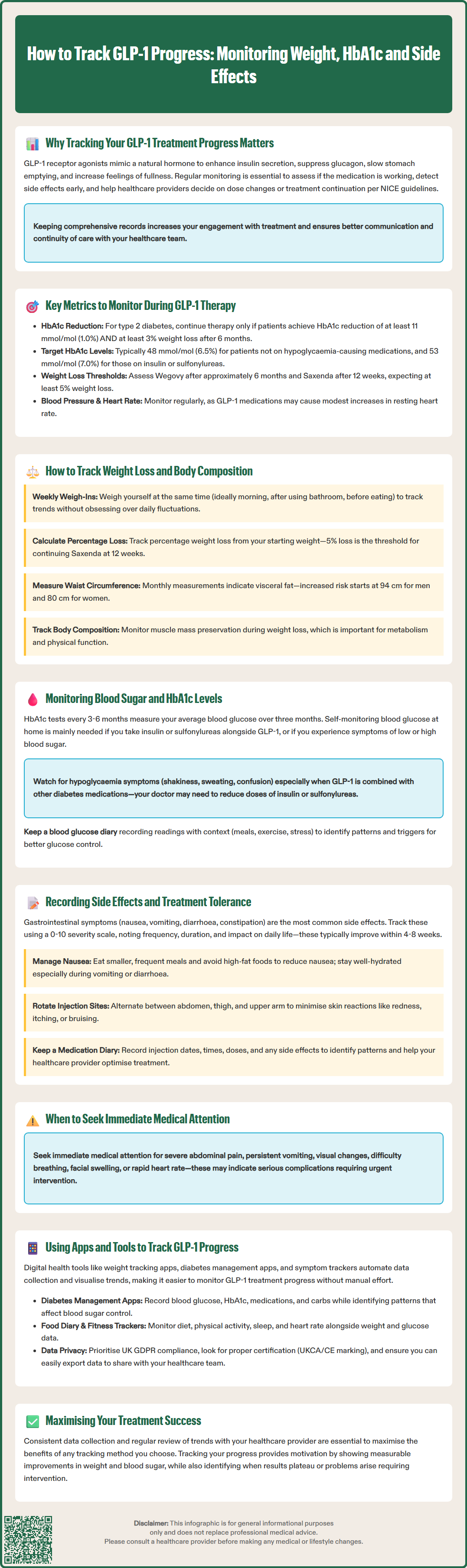
Effective monitoring of GLP-1 therapy requires attention to multiple clinical parameters, each providing insight into different aspects of treatment response and safety. Body weight remains a primary outcome measure, with different continuation criteria depending on the indication. For type 2 diabetes, NICE (NG28) recommends continuing GLP-1 therapy only if patients achieve both a reduction in HbA1c of at least 11 mmol/mol (1.0%) AND at least 3% weight loss after 6 months. For weight management, the criteria differ by medication: for Wegovy (semaglutide 2.4 mg), treatment should be evaluated after approximately 6 months; for Saxenda (liraglutide 3 mg), at least 5% weight loss should be achieved after 12 weeks on the 3 mg dose.
For diabetes management, glycaemic control—measured through HbA1c and self-monitored blood glucose—is paramount. NICE recommends individualised HbA1c targets: typically 48 mmol/mol (6.5%) for most adults with type 2 diabetes not on medications causing hypoglycaemia, and 53 mmol/mol (7.0%) for those on insulin or sulfonylureas.
Blood pressure and heart rate should be monitored regularly, as GLP-1 RAs may influence cardiovascular parameters. Some patients experience modest increases in resting heart rate, whilst others may see improvements in blood pressure as weight decreases. Lipid profiles may improve with GLP-1 therapy on average, particularly with weight loss, reflecting both direct metabolic effects and secondary benefits. Monitoring cholesterol levels helps assess cardiovascular risk reduction.
Gastrointestinal symptoms represent the most common adverse effects, including nausea, vomiting, diarrhoea, and constipation. Tracking the frequency and severity of these symptoms helps determine whether they are transient (as is typical during dose escalation) or persistent enough to warrant intervention. Injection site reactions, though less common, should also be documented.
Finally, monitoring treatment adherence and lifestyle factors—including dietary patterns, physical activity, and medication timing—provides context for interpreting clinical outcomes. These metrics collectively create a comprehensive picture of treatment response and guide ongoing management decisions.
Weight monitoring forms a cornerstone of GLP-1 therapy assessment, but the approach requires consistency and proper interpretation. Weigh yourself at the same time of day, ideally first thing in the morning after emptying your bladder and before eating, wearing similar clothing each time. Weekly measurements strike an appropriate balance—frequent enough to track trends without becoming obsessive about daily fluctuations caused by fluid retention, dietary sodium, or hormonal changes.
Record your weight in a dedicated journal, spreadsheet, or tracking application, and calculate your percentage weight loss from baseline. This metric is more meaningful than absolute weight change, particularly for clinical decision-making. For example, if you started at 100 kg and now weigh 94 kg, you have achieved 6% weight loss—exceeding the 5% threshold for Saxenda continuation at 12 weeks.
If you have a history of disordered eating, discuss an appropriate monitoring plan with your healthcare provider to ensure tracking doesn't trigger unhealthy behaviours.
Body composition provides additional valuable information beyond the number on the scales. Muscle mass preservation during weight loss is important for metabolic health and functional capacity. Consider measuring waist circumference monthly, as this reflects visceral adiposity and correlates with cardiometabolic risk. Use a tape measure positioned midway between the lowest rib and the iliac crest, measuring at the end of normal expiration. NHS guidance suggests increased health risks at waist measurements above 94 cm (37 inches) for men and 80 cm (31.5 inches) for women, with substantially increased risk above 102 cm (40 inches) for men and 88 cm (34.5 inches) for women.
Some patients benefit from bioelectrical impedance analysis (BIA) scales that estimate body fat percentage, though these measurements can be affected by hydration status and vary between devices. The trend over time on the same device is more informative than absolute values. Professional body composition assessments, such as DEXA scans, provide the most accurate data but are not routinely necessary. Photographs taken monthly in consistent lighting and clothing can also document visible changes that scales may not fully capture. Remember that weight loss typically follows a non-linear pattern, with more rapid initial loss followed by gradual, sustained reduction.
For individuals with type 2 diabetes, glycaemic monitoring is essential to assess the therapeutic efficacy of GLP-1 treatment. HbA1c (glycated haemoglobin) provides a three-month average of blood glucose levels and represents the gold standard for assessing long-term glycaemic control. Your GP or diabetes team will typically measure HbA1c every 3–6 months, with individualised targets based on your specific circumstances. NICE recommends a target of 48 mmol/mol (6.5%) for most adults with type 2 diabetes not taking medications that cause hypoglycaemia, and 53 mmol/mol (7.0%) for those on insulin or sulfonylureas. Targets may be relaxed for older adults or those with significant comorbidities.
Self-monitoring of blood glucose (SMBG) offers real-time feedback and helps identify patterns in glycaemic response. Whilst not all patients on GLP-1 monotherapy require routine SMBG, it becomes important if you are also taking insulin or sulfonylureas (which increase hypoglycaemia risk) or if you are experiencing symptoms of hypo- or hyperglycaemia. If advised to monitor, typical testing times include fasting (before breakfast) and two hours post-meal, with target ranges generally 4–7 mmol/L fasting and below 8.5 mmol/L post-prandially.
Keep a blood glucose diary noting the time, reading, and any relevant context (meals, exercise, stress, illness). This information helps identify triggers for glucose excursions and informs lifestyle modifications. Continuous glucose monitoring (CGM) or flash glucose monitoring systems are not routinely offered for type 2 diabetes patients on GLP-1 therapy alone. On the NHS, these technologies are generally commissioned for people with type 1 diabetes and selected type 2 diabetes patients on insulin therapy who meet specific criteria.
Be alert for symptoms of hypoglycaemia (shakiness, sweating, confusion, palpitations) or hyperglycaemia (increased thirst, frequent urination, fatigue). Whilst GLP-1 RAs have a low intrinsic risk of hypoglycaemia due to their glucose-dependent mechanism of action, the risk increases when combined with other glucose-lowering medications. When starting a GLP-1 RA, discuss with your healthcare provider whether your doses of sulfonylureas or insulin should be reduced to mitigate hypoglycaemia risk.
Attend your regular diabetic eye screening appointments, as rapid improvements in blood glucose control can sometimes temporarily worsen diabetic retinopathy. Report any new visual symptoms promptly to your healthcare provider.
Systematic documentation of adverse effects is crucial for optimising GLP-1 therapy and ensuring patient safety. Gastrointestinal symptoms—particularly nausea, vomiting, diarrhoea, and constipation—are common, with frequencies varying by product and dose (ranging from 10-40% in clinical trials according to SmPCs). These symptoms typically emerge during dose escalation and often improve over 4–8 weeks. Record the frequency, severity (mild, moderate, severe), and duration of these symptoms, along with any precipitating factors or effective management strategies you discover.
Use a symptom severity scale (e.g., 0–10) to quantify your experience consistently. Note whether symptoms interfere with daily activities, work, or sleep. Document any dietary modifications that help—many patients find that eating smaller, more frequent meals and avoiding high-fat foods reduces nausea. If symptoms persist beyond the initial adjustment period or significantly impact quality of life, your prescriber may recommend slower dose titration, temporary dose reduction, or anti-emetic medication.
Maintain adequate hydration, especially if experiencing vomiting or diarrhoea, as dehydration can lead to acute kidney injury. Contact your healthcare provider if you notice reduced urine output, dizziness when standing, or other signs of dehydration.
Injection site reactions—including redness, itching, or bruising—should be recorded with their location and duration. Rotating injection sites (abdomen, thigh, upper arm) typically minimises these issues. More serious but rare adverse effects require immediate medical attention and documentation. These include:
Severe abdominal pain (potentially indicating pancreatitis)—stop the medication immediately and seek urgent medical care
Persistent vomiting leading to dehydration
Visual changes or severe headaches
Persistent or symptomatic rapid heart rate or palpitations
Signs of allergic reaction (rash, difficulty breathing, facial swelling)
Symptoms of gallbladder disease (right upper quadrant pain, especially after meals)
Maintain a medication diary noting the date, time, and dose of each injection, along with any missed doses. This record helps identify patterns between dosing and symptom occurrence. If you experience severe abdominal pain, persistent vomiting, or signs of an allergic reaction, seek urgent medical attention via NHS 111 or 999 if severe.
You can report suspected side effects directly to the MHRA through the Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app, contributing to ongoing medication safety surveillance.
Digital health tools can significantly enhance the tracking process, providing convenient data collection, visualisation, and sharing capabilities. Weight tracking applications allow you to log measurements, view trend graphs, and calculate percentage changes automatically. Examples include health apps with weight-tracking features, or simple spreadsheet templates. Many apps integrate with Bluetooth-enabled scales for seamless data transfer, reducing the burden of manual entry.
Diabetes management apps provide comprehensive platforms for recording blood glucose readings, HbA1c results, medications, and carbohydrate intake. These applications often include pattern recognition features that identify trends and provide insights into factors affecting glycaemic control. Some integrate with blood glucose meters or continuous glucose monitors for those who use these devices.
Symptom tracking applications enable systematic recording of side effects, their severity, and potential triggers. These tools often include customisable symptom lists, medication reminders, and the ability to generate reports for healthcare appointments. The visual representation of symptom patterns over time can reveal whether adverse effects are improving, stable, or worsening.
Food diary apps help monitor dietary intake, which significantly influences both weight loss and glycaemic control. Such applications track calories, macronutrients, and meal timing, providing context for understanding treatment response. Some patients find that photographing meals serves as a simpler alternative to detailed calorie counting.
Fitness trackers and smartwatches monitor physical activity, heart rate, and sleep patterns—all relevant to overall health outcomes. Many integrate with health apps, creating a comprehensive health dashboard.
When selecting digital tools, consider data privacy and UK GDPR compliance. Check whether apps have appropriate certification (UKCA/CE marking where applicable) and allow easy export or sharing of information with your healthcare team. The NHS App (in England) provides a secure platform for viewing test results and communicating with your GP practice, though similar services may vary in Scotland, Wales, and Northern Ireland. Regardless of the tools chosen, consistency in data collection and regular review of trends with your healthcare provider maximise the benefits of tracking your GLP-1 treatment progress.
Weigh yourself weekly at the same time of day, ideally first thing in the morning after emptying your bladder and before eating. Weekly measurements track trends effectively without becoming obsessive about daily fluctuations caused by fluid retention or dietary changes.
NICE guidance recommends continuing GLP-1 therapy for type 2 diabetes only if you achieve both an HbA1c reduction of at least 11 mmol/mol (1.0%) AND at least 3% weight loss after 6 months of treatment.
Seek urgent medical attention if you experience severe abdominal pain (potentially pancreatitis), persistent vomiting causing dehydration, visual changes, signs of allergic reaction, or symptoms of gallbladder disease. Mild gastrointestinal symptoms typically improve over 4–8 weeks.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.