
Starting a GLP-1 receptor agonist can feel daunting, but understanding what to expect during your first week helps you prepare and manage the transition effectively. GLP-1 medications such as semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity) are prescribed in the UK for type 2 diabetes or weight management under NICE guidance. During the initial week, most patients experience gastrointestinal side effects—particularly nausea and reduced appetite—as the body adjusts to the medication's effects on digestion and satiety. Whilst these symptoms can be uncomfortable, they typically diminish within a few weeks. This article outlines the common experiences, practical management strategies, and when to seek medical advice during your first week on GLP-1 therapy.
Quick Answer: During the first week of GLP-1 therapy, most patients experience gastrointestinal side effects such as nausea, reduced appetite, and changes in digestion, which typically improve within 2–4 weeks as the body adjusts.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management, though some specific formulations are now licensed for weight management in adults with obesity or overweight with weight-related comorbidities. In the UK, medications such as semaglutide (Ozempic for diabetes; Wegovy for weight management), dulaglutide (Trulicity), liraglutide (Victoza for diabetes; Saxenda for weight management), and oral semaglutide (Rybelsus) are prescribed under NICE guidance for specific clinical indications.
These medications work by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. GLP-1 receptor agonists exert their therapeutic effects through several mechanisms: they stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, suppress glucagon release (which reduces hepatic glucose production), slow gastric emptying, and act on appetite centres in the hypothalamus to promote satiety and reduce food intake.
The glucose-dependent mechanism of insulin secretion means that GLP-1 medications generally carry a lower risk of hypoglycaemia compared to some other diabetes treatments. However, when combined with insulin or sulfonylureas, the risk of hypoglycaemia increases significantly, and dose adjustments of these medications may be necessary. Most GLP-1 receptor agonists are administered via subcutaneous injection, either daily or weekly depending on the specific formulation, with Rybelsus being the exception as an oral tablet.
When initiating GLP-1 therapy, prescribers typically start with a low dose and gradually titrate upwards over several weeks. This dose escalation strategy helps minimise gastrointestinal side effects whilst allowing the body to adapt to the medication's effects. Patients with pre-existing diabetic retinopathy should be aware that rapid improvements in glucose control with semaglutide may temporarily worsen retinopathy and should report any visual changes promptly.
GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding. Patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not use these medications, as studies in rodents have shown an increased risk of thyroid C-cell tumours (though the relevance to humans remains uncertain).
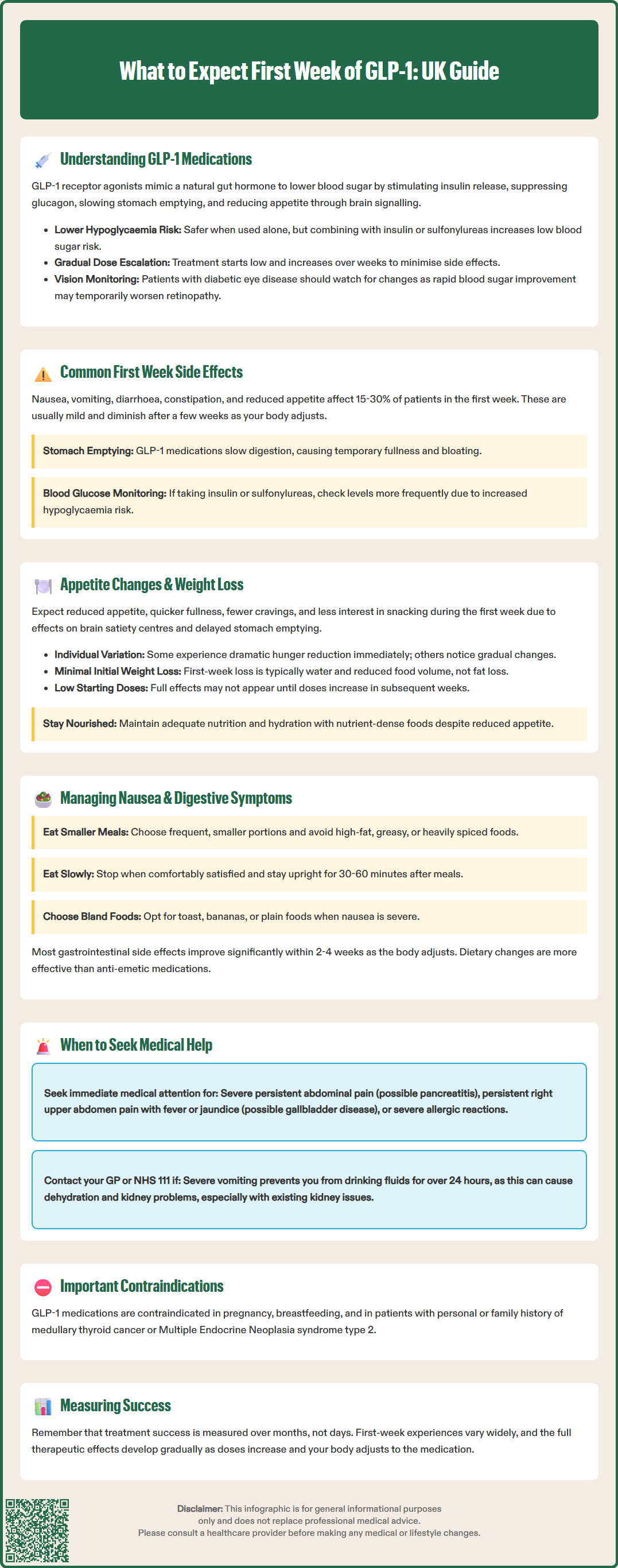
During the first week of GLP-1 therapy, patients commonly experience gastrointestinal side effects, which are the most frequently reported adverse reactions. These typically include nausea, vomiting, diarrhoea, constipation, abdominal discomfort, and reduced appetite. According to product SmPCs, nausea affects approximately 15-30% of patients on standard doses, though rates vary by specific product and dose, with higher frequencies during dose escalation.
The gastrointestinal symptoms occur primarily because GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach for longer periods. Whilst this mechanism contributes to the medication's appetite-suppressing effects, it can initially cause feelings of fullness, bloating, or discomfort. Most patients find these side effects are mild to moderate in severity and tend to diminish significantly after the first few weeks as the body adjusts to the medication.
Other side effects that may emerge during the first week include headache, fatigue, dizziness, and injection site reactions such as redness, itching, or mild swelling. Some patients report changes in taste or a general feeling of being unwell as their body adapts to the medication. It is important to note that not everyone experiences side effects, and some individuals tolerate GLP-1 medications very well from the outset.
Patients taking insulin or sulfonylureas alongside GLP-1 receptor agonists should monitor their blood glucose more frequently during the first week, as the combination can increase the risk of hypoglycaemia. Discuss with your healthcare provider whether dose adjustments of these medications might be needed.
Serious adverse effects are rare but require immediate medical attention. If you experience severe, persistent abdominal pain (particularly if radiating to the back), you should stop taking the medication and seek urgent medical care, as this could indicate pancreatitis. Signs of gallbladder disease requiring prompt assessment include persistent pain in the right upper abdomen, fever, yellowing of the skin or eyes (jaundice), pale stools, or dark urine. Severe allergic reactions, though very rare, require emergency treatment.
Patients should contact their GP or NHS 111 if they experience severe or persistent vomiting that prevents adequate fluid intake, as this may lead to dehydration and acute kidney injury, particularly in those with pre-existing renal impairment. Any suspected side effects can be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
One of the most noticeable effects during the first week of GLP-1 therapy is a marked reduction in appetite and changes in eating patterns. Many patients report feeling full more quickly during meals, experiencing reduced food cravings, and having less interest in eating between meals. This appetite suppression is a direct result of the medication's action on satiety centres in the brain and the delayed gastric emptying that creates prolonged feelings of fullness.
The degree of appetite reduction varies considerably between individuals. Some patients describe a dramatic decrease in hunger from the very first dose, whilst others notice more gradual changes over the first week. It is not uncommon for patients to find that foods they previously enjoyed no longer appeal to them, or that they can only manage smaller portion sizes than usual. These changes are expected therapeutic effects rather than concerning side effects, though they can feel quite pronounced initially.
Regarding weight loss in the first week, expectations should be realistic and individualised. Early weight changes are highly variable; while some patients may notice a small reduction during the initial week, others may see no change at all. Any early weight loss often reflects fluid loss and reduced food volume in the digestive system rather than significant fat loss. Sustainable fat loss typically occurs more gradually over subsequent weeks and months. NICE guidance emphasises that GLP-1 medications for weight management (Wegovy and Saxenda) should be used alongside lifestyle modifications, including dietary changes and increased physical activity.
Patients should be aware that the starting dose of GLP-1 medication is intentionally low to minimise side effects, meaning the full appetite-suppressing and weight-reducing effects may not be apparent until the dose is titrated upwards. It is important to maintain adequate nutrition and hydration during this adjustment period, focusing on nutrient-dense foods even when appetite is reduced. Patients should not expect dramatic weight loss in the first week, and healthcare professionals typically assess treatment response over a period of months rather than days.
For those prescribed GLP-1 medications specifically for weight management (Wegovy or Saxenda), treatment continuation will be assessed according to NICE criteria, which typically require a minimum percentage weight loss within a specified timeframe. Remember that Ozempic, Victoza, Trulicity, and Rybelsus are licensed for type 2 diabetes management, not weight loss, though weight reduction may occur as a beneficial side effect.
Nausea is the most commonly reported side effect during the first week of GLP-1 therapy, but several practical strategies can help minimise this symptom and improve tolerability. Dietary modifications are often the most effective first-line approach. Patients should consider eating smaller, more frequent meals rather than three large meals, as this reduces the burden on the already-slowed digestive system. Avoiding high-fat, greasy, or heavily spiced foods can also help, as these take longer to digest and may exacerbate feelings of fullness and nausea. Minimising alcohol consumption, particularly around injection days or dose increases, is also advisable.
Practical tips for managing nausea include:
Eating slowly and chewing food thoroughly to aid digestion
Stopping eating as soon as you feel comfortably satisfied, rather than finishing everything on your plate
Avoiding lying down immediately after meals; remaining upright for at least 30–60 minutes aids gastric emptying
Staying well-hydrated with small, frequent sips of water throughout the day
Choosing bland, easily digestible foods such as toast, crackers, rice, or bananas if nausea is pronounced
Avoiding strong food odours that may trigger nausea
Taking the injection at a time of day when nausea would be least disruptive (some patients prefer evening injections so they sleep through peak side effects)
For patients experiencing constipation, increasing dietary fibre intake gradually, maintaining good hydration, and engaging in regular physical activity can help promote bowel regularity. Conversely, those with diarrhoea should ensure adequate fluid and electrolyte replacement to prevent dehydration. Over-the-counter oral rehydration solutions can be helpful if diarrhoea or vomiting is significant.
Patients taking insulin or sulfonylureas should monitor their blood glucose more frequently when reducing meal sizes, as the risk of hypoglycaemia may increase. Discuss with your healthcare provider whether dose adjustments of these medications might be needed.
When to seek medical advice: Patients should contact their GP or prescribing clinician if nausea is severe and persistent, if they are unable to keep down fluids for more than 24 hours, if they experience severe abdominal pain, or if side effects significantly impact their quality of life. In some cases, the dose may need to be reduced temporarily, or the titration schedule adjusted. Anti-emetic medications are generally not recommended as first-line treatment, as most nausea resolves with dietary adjustments and time. However, if symptoms are particularly troublesome, healthcare professionals may consider short-term symptomatic relief whilst the body adjusts to the medication. Most patients find that gastrointestinal side effects improve significantly after the first 2–4 weeks of treatment, and the benefits of the medication become more apparent as tolerance develops.
Nausea is most common during the first week of GLP-1 therapy and typically improves significantly within 2–4 weeks as your body adjusts to the medication. Eating smaller, more frequent meals and avoiding high-fat foods can help manage symptoms during this adjustment period.
Weight loss during the first week is highly variable and often minimal, as starting doses are intentionally low. Any early weight changes typically reflect fluid loss rather than significant fat loss, which occurs more gradually over subsequent weeks and months with dose escalation.
Seek urgent medical attention if you experience severe persistent abdominal pain (especially radiating to the back), signs of gallbladder disease such as right upper abdominal pain with fever or jaundice, or inability to keep down fluids for more than 24 hours. Contact your GP if side effects significantly impact your quality of life.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.