GLP-1 agonists such as semaglutide and liraglutide are increasingly prescribed for type 2 diabetes and weight management, but their use in patients with Crohn's disease requires careful consideration. Whilst current limited evidence does not suggest these medications directly worsen inflammatory bowel disease activity, their gastrointestinal side effects—including nausea, diarrhoea, and abdominal pain—may overlap with Crohn's symptoms, complicating disease monitoring. This article examines the mechanism of GLP-1 agonists, their potential risks in Crohn's disease, practical management strategies, and alternative weight management options for patients with inflammatory bowel disease.
Quick Answer: Current limited evidence does not suggest GLP-1 agonists directly worsen Crohn's disease, but their gastrointestinal side effects may complicate symptom monitoring and disease assessment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily licensed for the management of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. These medicines include semaglutide (Ozempic®, Wegovy®, Rybelsus®), dulaglutide (Trulicity®), liraglutide (Victoza®, Saxenda®), exenatide (Byetta®, Bydureon®), and lixisenatide (Lyxumia®).
GLP-1 agonists work by mimicking the action of naturally occurring GLP-1, an incretin hormone released from the intestinal L-cells in response to food intake. The mechanism of action involves several physiological processes:
Enhanced insulin secretion: They stimulate glucose-dependent insulin release from pancreatic beta cells, which helps lower blood glucose levels without causing hypoglycaemia when glucose levels are normal
Suppressed glucagon secretion: They reduce inappropriate glucagon release from pancreatic alpha cells, further improving glycaemic control
Delayed gastric emptying: They slow the rate at which food leaves the stomach, promoting satiety and reducing postprandial glucose excursions. This effect is dose-dependent and may diminish with continued use
Central appetite regulation: They act on receptors in the hypothalamus and other brain regions to reduce appetite and food intake
Most GLP-1 agonists are administered via subcutaneous injection, with dosing frequencies ranging from once daily to once weekly depending on the specific agent. Semaglutide is also available as an oral formulation (Rybelsus®). The MHRA has approved various GLP-1 agonists for specific indications, with NICE providing guidance on their use in type 2 diabetes (NG28) and weight management (TA875 for semaglutide/Wegovy®, TA664 for liraglutide/Saxenda®). It's important to note that indications differ by brand, and off-label use is not advised. The gastrointestinal effects are central to both their therapeutic benefits and their side effect profile.
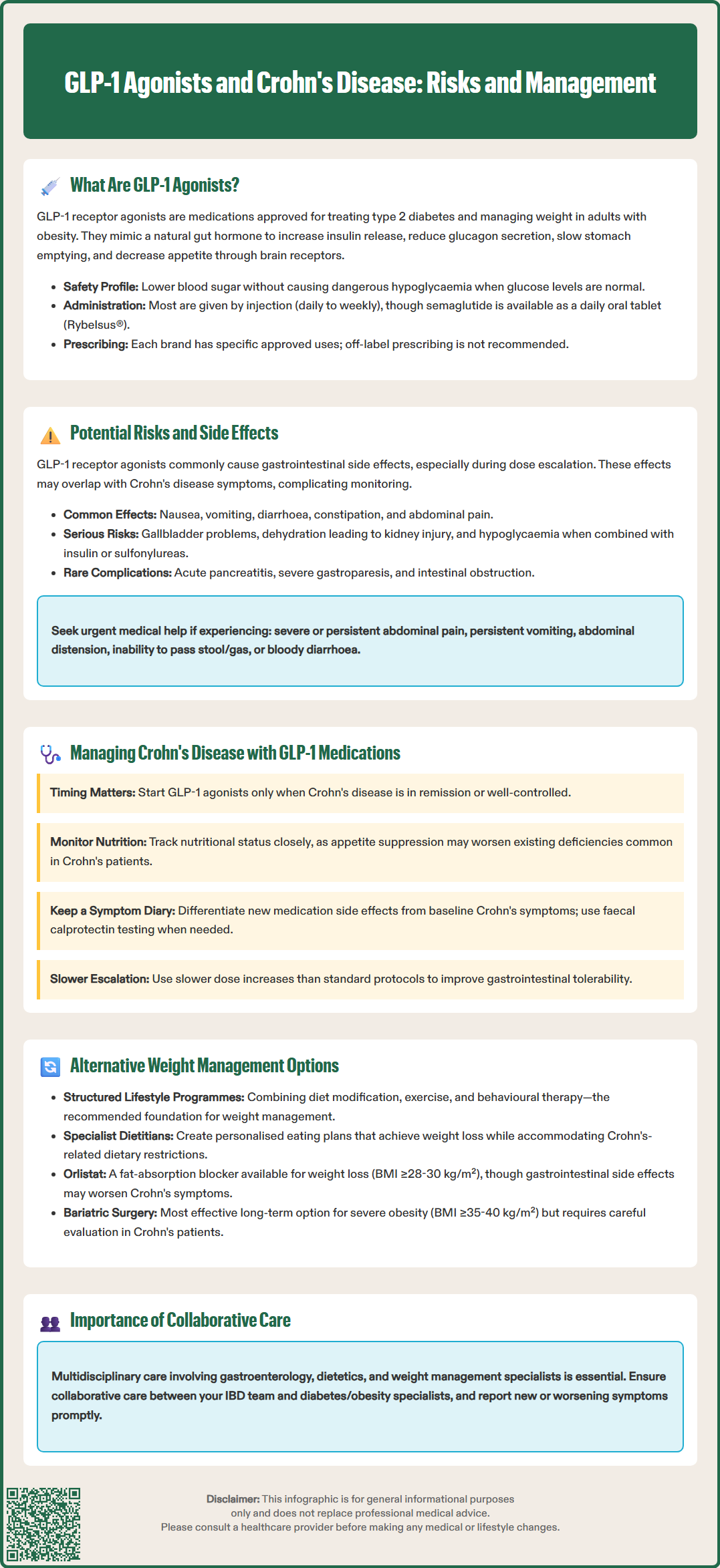
Gastrointestinal adverse effects are the most commonly reported side effects of GLP-1 receptor agonists, occurring in a significant proportion of patients. Understanding these effects is particularly important for individuals with pre-existing gastrointestinal conditions such as Crohn's disease.
The most frequent gastrointestinal side effects include:
Nausea and vomiting: Very common, typically most pronounced during dose escalation
Diarrhoea: Common to very common, though usually mild to moderate
Constipation: Can occur due to delayed gastric emptying and reduced gut motility
Abdominal pain and discomfort: Common
Dyspepsia and gastro-oesophageal reflux: May worsen in susceptible individuals
Other important adverse effects include:
Gallbladder disorders: Cholelithiasis and cholecystitis have been reported, particularly with weight loss
Dehydration and acute kidney injury: May occur secondary to severe gastrointestinal symptoms
Hypoglycaemia: Risk increases when used with insulin or sulfonylureas, which may require dose adjustment
Current limited evidence does not suggest an increased risk of inflammatory bowel disease (IBD) flares with GLP-1 agonists, though more data are needed. However, the gastrointestinal side effects of these medications may overlap with or potentially complicate the symptom profile of Crohn's disease. The delayed gastric emptying and altered gut motility could theoretically affect disease monitoring and symptom interpretation in patients with established Crohn's disease.
Rare but serious gastrointestinal complications have been reported in post-marketing surveillance, including:
Acute pancreatitis: If suspected, the GLP-1 agonist should be stopped immediately and not restarted if pancreatitis is confirmed
Severe gastroparesis: Rare post-marketing reports of severe delayed gastric emptying
Intestinal obstruction: Very rare cases reported in post-marketing surveillance
Patients should be advised to seek urgent medical help via NHS 111, A&E or 999 as appropriate if they experience severe or persistent abdominal pain, persistent vomiting, abdominal distension, inability to pass stool or gas, or bloody diarrhoea whilst taking GLP-1 agonists. Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
For patients with established Crohn's disease who are considering or currently taking GLP-1 receptor agonists, careful clinical assessment and ongoing monitoring are essential. While current limited evidence does not suggest these medications directly worsen Crohn's disease activity, their gastrointestinal effects require thoughtful management.
Pre-treatment considerations should include:
Disease activity assessment: GLP-1 agonists should ideally be initiated when Crohn's disease is in remission or well-controlled, as distinguishing medication side effects from disease flare becomes challenging during active inflammation
Nutritional status evaluation: Patients with Crohn's disease may already have compromised nutritional status; the appetite-suppressing effects of GLP-1 agonists require careful consideration
Medication absorption: Delayed gastric emptying may theoretically affect the absorption of oral Crohn's disease medications, though clinical significance remains unclear
Ongoing monitoring strategies include:
Symptom diary: Patients should maintain records distinguishing new gastrointestinal symptoms from their baseline Crohn's pattern
Faecal calprotectin testing: When clinically indicated to differentiate inflammatory activity from functional symptoms, in line with NICE DG11 guidance
Nutritional surveillance: Regular assessment of weight, body composition, and nutritional markers (albumin, vitamins, minerals)
Dose titration: Slower than standard dose escalation may improve gastrointestinal tolerability
Collaborative care between gastroenterology and diabetes/obesity services is strongly recommended. Patients should be advised to contact their IBD team or GP for new or changing symptoms, and to use NHS 111 or attend A&E for severe acute symptoms. Consider temporary interruption of the GLP-1 agonist during assessment if diagnostic uncertainty persists.
The decision to continue GLP-1 therapy should be individualised, weighing metabolic benefits against gastrointestinal tolerability and disease control. Documentation of baseline symptoms and faecal calprotectin before initiation where feasible can help with subsequent assessment. If symptoms cannot be adequately distinguished from Crohn's activity, temporary discontinuation may be necessary to clarify the clinical picture.
For patients with Crohn's disease who require weight management but cannot tolerate or are unsuitable for GLP-1 receptor agonists, several alternative approaches are available, aligned with NICE guidance on obesity management (CG189).
Pharmacological alternatives include:
Orlistat: A lipase inhibitor that reduces dietary fat absorption by approximately 30%. Available as prescription-strength Xenical® and over-the-counter Alli® (lower dose). Whilst generally well-tolerated, it can cause gastrointestinal side effects (steatorrhoea, faecal urgency) that may be problematic in Crohn's disease. Licensed for BMI ≥30 kg/m² or ≥28 kg/m² with comorbidities
Naltrexone-bupropion combination (Mysimba®): Licensed in the UK but with limited NHS availability as NICE terminated its technology appraisal. May be considered under specialist advice; acts centrally to reduce appetite
Setmelanotide: Reserved for specific genetic obesity syndromes (e.g., POMC/PCSK1/LEPR deficiency, Bardet-Biedl syndrome) under specialist supervision
Non-pharmacological interventions form the cornerstone of weight management and may be particularly appropriate:
Structured lifestyle programmes: NICE recommends multicomponent interventions including dietary modification, increased physical activity, and behavioural strategies. Tier 2 and Tier 3 weight management services provide intensive support
Dietetic input: Specialist dietitians can develop individualised plans accommodating Crohn's-related dietary restrictions whilst achieving caloric deficit
Psychological support: Cognitive behavioural therapy and motivational interviewing address eating behaviours and emotional factors
Physical activity programmes: Tailored exercise plans considering Crohn's-related fatigue and extra-intestinal manifestations
Bariatric surgery represents the most effective long-term weight management intervention for severe obesity. NICE criteria include BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities, with consideration for BMI 30-34.9 kg/m² with recent-onset type 2 diabetes and lower thresholds for some ethnic groups. Patients with Crohn's disease require careful pre-operative assessment, as previous intestinal surgery, active inflammation, or malnutrition may affect surgical candidacy and outcomes. Procedures such as sleeve gastrectomy or gastric bypass should only be considered in specialist centres with expertise in both bariatric surgery and IBD management.
The optimal approach requires individualised assessment considering disease activity, nutritional status, comorbidities, and patient preferences, delivered through multidisciplinary collaboration between gastroenterology, dietetics, and weight management services.
Current limited evidence does not suggest GLP-1 agonists worsen Crohn's disease, but their gastrointestinal side effects may complicate symptom monitoring. Ideally, these medications should be started when Crohn's disease is in remission, with close collaboration between your gastroenterology and diabetes/obesity teams.
The most common gastrointestinal side effects include nausea, vomiting, diarrhoea, constipation, and abdominal pain. These symptoms may overlap with Crohn's disease symptoms, making it challenging to distinguish medication side effects from disease flares without careful monitoring.
Alternatives include orlistat (though it may cause gastrointestinal side effects), structured lifestyle programmes with dietetic support, psychological interventions, tailored physical activity, and bariatric surgery for eligible patients. The optimal approach requires individualised assessment considering your Crohn's disease activity and nutritional status.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.