
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes, whilst Crohn's disease is a chronic inflammatory bowel condition requiring careful management. Many patients wonder whether Mounjaro and Crohn's disease are compatible, particularly given the medication's gastrointestinal side effects. Whilst Crohn's disease is not an absolute contraindication, the decision requires individualised assessment based on disease activity, symptom burden, and potential risks. This article examines the safety considerations, potential complications, and alternative options for patients with Crohn's disease considering Mounjaro therapy.
Quick Answer: Mounjaro is not specifically contraindicated in Crohn's disease, but use requires careful individualised assessment, particularly in patients with active disease or severe gastrointestinal symptoms.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. For weight management, tirzepatide is marketed as Zepbound, though availability may vary. It is administered as a once-weekly subcutaneous injection and represents a novel class of medication known as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The mechanism of action involves mimicking two naturally occurring incretin hormones that regulate blood glucose and appetite. By activating both GIP and GLP-1 receptors, Mounjaro enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. This dual action contributes to improved glycaemic control and significant weight loss in clinical trials.
In the UK, Mounjaro is available through NHS prescription for eligible patients with type 2 diabetes in line with NICE Technology Appraisal guidance (TA848). Starting doses begin at 2.5 mg weekly (an initiation dose not intended for glycaemic control), with gradual titration up to a maintenance dose of 5 mg, 10 mg, or 15 mg, depending on individual response and tolerability.
Important safety considerations include:
Not recommended in patients with severe gastrointestinal disease, including severe gastroparesis
Risk of pancreatitis (discontinue if suspected)
Potential for gallbladder disease (cholelithiasis, cholecystitis)
Risk of dehydration potentially leading to acute kidney injury
Increased hypoglycaemia risk when used with insulin or sulfonylureas
Potential worsening of diabetic retinopathy, particularly with rapid glycaemic improvement
Reduced oral contraceptive effectiveness (additional contraception advised for 4 weeks after starting and after each dose increase)
Not recommended during pregnancy or breastfeeding
Patients considering Mounjaro should understand that it is not a short-term solution but rather part of a comprehensive approach to metabolic health that includes dietary modification, physical activity, and ongoing medical supervision.
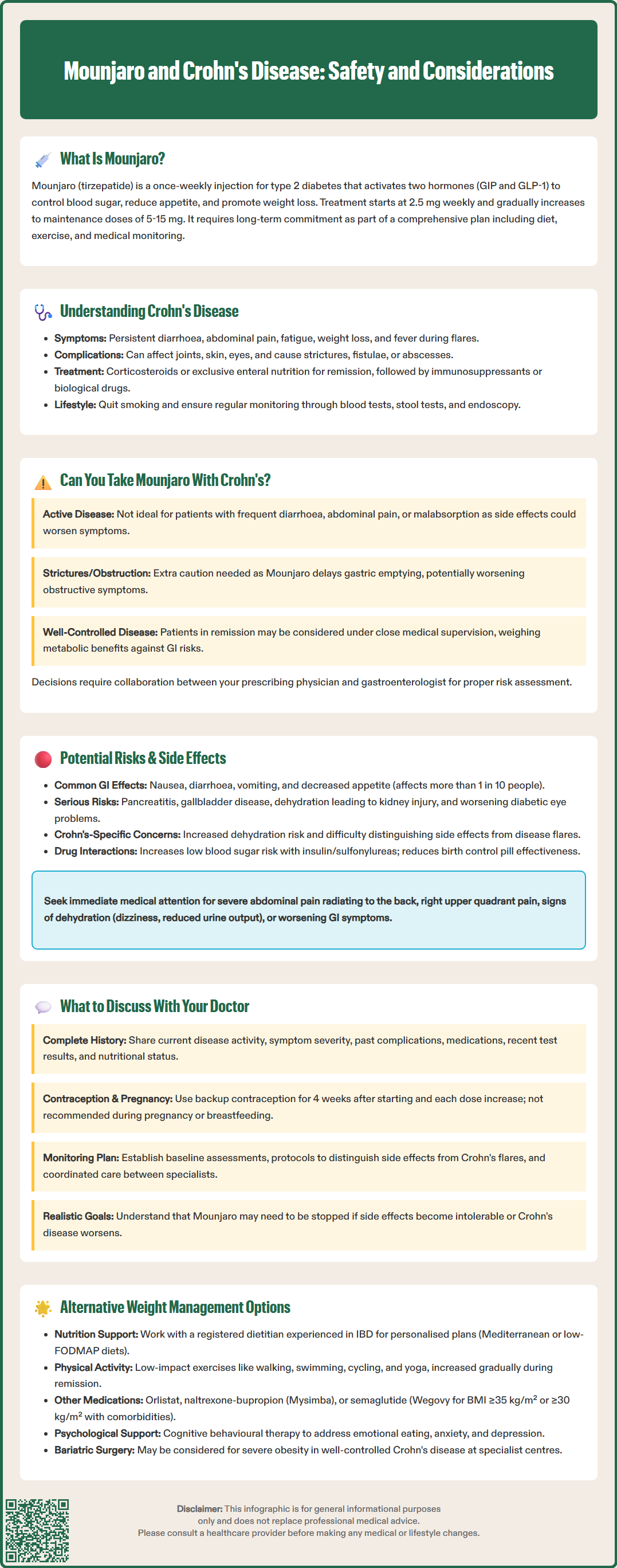
Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract from mouth to anus, though it most commonly involves the terminal ileum and colon. The condition is characterised by transmural inflammation, meaning it affects the full thickness of the bowel wall, and typically follows a relapsing-remitting course with periods of active disease (flares) and remission.
Common symptoms include persistent diarrhoea (which may be bloody), abdominal pain and cramping, fatigue, unintended weight loss, reduced appetite, and fever during active flares. Patients may also experience extra-intestinal manifestations such as arthritis, skin lesions (erythema nodosum, pyoderma gangrenosum), eye inflammation (uveitis), and oral ulcers. Complications can include strictures, fistulae, abscesses, and malnutrition due to malabsorption.
According to NICE guidance (NG129), management of Crohn's disease involves inducing and maintaining remission through pharmacological therapy, nutritional support, and sometimes surgical intervention. First-line treatments for inducing remission typically include corticosteroids (prednisolone or budesonide) or exclusive enteral nutrition, particularly in children. Maintenance therapy often involves immunosuppressants such as azathioprine, mercaptopurine, or methotrexate, and biological therapies including:
Anti-TNF agents (infliximab, adalimumab)
Anti-integrins (vedolizumab)
Anti-IL-12/23 (ustekinumab)
Anti-IL-23 (risankizumab)
Regular monitoring through clinical assessment, inflammatory markers (CRP, faecal calprotectin), and endoscopic evaluation helps guide treatment decisions. Patients require multidisciplinary care involving gastroenterologists, IBD specialist nurses, dietitians, and sometimes colorectal surgeons.
Patients should seek urgent medical attention if they experience severe, persistent abdominal pain with vomiting or fever, signs of bowel obstruction, significant rectal bleeding, or perianal pain/swelling suggesting abscess. Smoking cessation is strongly recommended as smoking worsens disease outcomes. Appropriate vaccinations and bone health monitoring are also important aspects of comprehensive care.
The question of whether patients with Crohn's disease can safely use Mounjaro requires careful consideration, as there is no official contraindication specifically listing Crohn's disease in the Summary of Product Characteristics (SmPC) for tirzepatide. However, the SmPC does state that use is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. The decision must be individualised based on disease activity, gastrointestinal symptoms, and overall clinical status.
Patients with active Crohn's disease experiencing frequent diarrhoea, abdominal pain, or malabsorption may not be ideal candidates for Mounjaro, primarily because the medication's gastrointestinal side effects could exacerbate existing symptoms or make it difficult to distinguish between disease flare and medication-related adverse effects. Additionally, patients with strictures or a history of bowel obstruction require particular caution, as delayed gastric emptying—a therapeutic effect of GLP-1 receptor agonists—could theoretically worsen obstructive symptoms, though this remains a theoretical concern requiring individualised assessment.
Conversely, patients with well-controlled Crohn's disease in remission who require treatment for type 2 diabetes may be considered for Mounjaro therapy under close medical supervision. The potential metabolic benefits must be weighed against gastrointestinal risks on an individual basis. There is currently limited published data specifically examining tirzepatide use in IBD populations, so clinical decisions rely on extrapolation from GLP-1 receptor agonist class effects and individual patient factors.
It is essential that any decision to prescribe Mounjaro to a patient with Crohn's disease involves collaboration between the prescribing physician (endocrinologist or GP) and the patient's gastroenterologist. This multidisciplinary approach ensures comprehensive risk assessment and appropriate monitoring strategies are in place before initiating therapy.
Gastrointestinal adverse effects are among the most commonly reported side effects of Mounjaro and other GLP-1 receptor agonists. According to the SmPC, the following frequencies have been observed:
Nausea (very common: may affect more than 1 in 10 people)
Diarrhoea (very common: may affect more than 1 in 10 people)
Vomiting (very common: may affect more than 1 in 10 people)
Constipation (common: may affect up to 1 in 10 people)
Abdominal pain and discomfort (common: may affect up to 1 in 10 people)
Decreased appetite (very common: may affect more than 1 in 10 people)
These effects typically diminish over time as the body adjusts to the medication, and gradual dose escalation helps minimise their severity. However, for patients with Crohn's disease, distinguishing between medication side effects and disease flare becomes challenging, potentially delaying appropriate management of IBD exacerbation.
More serious gastrointestinal concerns include pancreatitis. Patients should be counselled to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back, and treatment should be discontinued if pancreatitis is suspected. Gallbladder disease (cholelithiasis, cholecystitis) has also been reported with GLP-1 receptor agonists, and patients should be advised to report symptoms such as right upper quadrant pain, nausea, or vomiting.
For Crohn's disease patients, particular concerns include:
Dehydration risk from combined diarrhoea (disease-related and medication-induced), which may lead to acute kidney injury
Malabsorption potentially worsened by rapid gastrointestinal transit
Difficulty monitoring disease activity due to overlapping symptoms
Nutritional compromise in patients already at risk of deficiencies
Patients should maintain adequate hydration, monitor for signs of dehydration (dizziness, reduced urine output, dry mouth), and report any worsening gastrointestinal symptoms promptly to their healthcare team. If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk.
Before initiating Mounjaro therapy, patients with Crohn's disease should have a comprehensive discussion with their healthcare provider covering several critical areas. Full disclosure of your IBD history is essential, including:
Current disease activity status (active flare versus remission)
Frequency and severity of symptoms (diarrhoea episodes, abdominal pain)
Previous complications (strictures, fistulae, abscesses, surgeries)
Current Crohn's medications and their effectiveness
Recent inflammatory markers and endoscopic findings
Nutritional status and any existing deficiencies
Medication interactions and safety considerations should be reviewed carefully:
If you use oral contraceptives, be aware that tirzepatide may reduce their effectiveness. Additional contraception is advised for 4 weeks after starting treatment and after each dose increase.
If you are pregnant, planning pregnancy, or breastfeeding, tirzepatide is not recommended.
If you have diabetes and use insulin or sulfonylureas, discuss hypoglycaemia risk and potential dose adjustments.
If you have diabetic retinopathy, discuss monitoring requirements, as rapid improvement in blood glucose can worsen retinopathy.
The delayed gastric emptying caused by Mounjaro may affect the absorption of oral medications. Medications with narrow therapeutic windows may need dosing adjustments.
Alternative treatment options should be explored, particularly if the primary indication is weight management rather than diabetes control. For some Crohn's patients, addressing inflammation and achieving disease remission may naturally improve metabolic parameters without additional pharmacotherapy.
Monitoring plans must be established before starting treatment, including:
Baseline assessment of disease activity and nutritional status
Clear protocols for distinguishing medication side effects from disease flare
Defined thresholds for contacting the IBD team or prescriber
Regular follow-up appointments during dose titration
Coordination between gastroenterology and endocrinology/primary care teams
Patients should also discuss their treatment goals and expectations, understanding that if gastrointestinal side effects prove intolerable or disease control deteriorates, Mounjaro may need to be discontinued. Having realistic expectations and a clear plan for managing potential complications helps ensure patient safety and treatment success.
For patients with Crohn's disease who require weight management but for whom Mounjaro may not be suitable, several alternative approaches merit consideration. The optimal strategy depends on individual circumstances, disease activity, and metabolic goals.
Lifestyle interventions remain the foundation of weight management for all patients, including those with IBD. Working with a registered dietitian experienced in inflammatory bowel disease is particularly valuable, as they can develop personalised nutrition plans that support both weight management and IBD control. The low-FODMAP diet, whilst primarily used for irritable bowel syndrome, may help some Crohn's patients identify trigger foods whilst maintaining nutritional adequacy. Anti-inflammatory dietary patterns, such as the Mediterranean diet, may offer dual benefits for metabolic health and IBD management, though evidence specific to Crohn's disease remains limited.
Structured physical activity programmes tailored to individual capabilities can support weight management without exacerbating IBD symptoms. Low-impact activities such as walking, swimming, cycling, and yoga are generally well-tolerated and provide cardiovascular and metabolic benefits. Patients should be encouraged to increase activity gradually, particularly during remission periods.
Alternative pharmacological options may include:
Orlistat – a lipase inhibitor that reduces fat absorption. However, gastrointestinal side effects including steatorrhoea may be problematic for IBD patients, and fat-soluble vitamin supplementation may be necessary.
Naltrexone-bupropion combination (Mysimba) – acts centrally to reduce appetite, with fewer direct gastrointestinal effects. Contraindicated in uncontrolled hypertension, seizure disorders, and certain other conditions.
Semaglutide (Wegovy) – a GLP-1 receptor agonist approved for weight management in the UK under NICE TA875 for adults with a BMI of at least 35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) and at least one weight-related comorbidity. It shares similar gastrointestinal side effect profiles with tirzepatide.
Access to NHS weight management services follows a tiered approach. Patients may be referred to Tier 3 specialist weight management services for multidisciplinary support before considering pharmacotherapy or surgical options.
Psychological support through cognitive behavioural therapy or counselling may address emotional eating, body image concerns, and the psychological impact of living with chronic illness. Many Crohn's patients experience anxiety and depression, which can influence eating behaviours and weight management success.
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) and well-controlled Crohn's disease, bariatric surgery may be considered in specialist centres (Tier 4 services) with experience in IBD populations, though this requires careful multidisciplinary assessment. The decision must account for surgical risks, potential impact on IBD management, and long-term nutritional implications.
Ultimately, the most effective approach combines multiple strategies tailored to individual needs, preferences, and disease characteristics, with ongoing support from a multidisciplinary team including gastroenterologists, dietitians, endocrinologists, and mental health professionals where appropriate.
Mounjaro is not specifically contraindicated in Crohn's disease, but it is not recommended for patients with severe gastrointestinal disease. Patients with well-controlled Crohn's in remission may be considered for treatment under close medical supervision, whilst those with active disease should generally avoid it due to overlapping gastrointestinal side effects.
Very common side effects include nausea, diarrhoea, vomiting, and decreased appetite, affecting more than 1 in 10 people. Common side effects include constipation and abdominal pain. These effects typically diminish over time but may be difficult to distinguish from Crohn's disease symptoms.
Discuss your current Crohn's disease activity status, symptom frequency, previous complications, current medications, and recent test results. Ensure coordination between your gastroenterologist and prescribing doctor, establish clear monitoring protocols, and discuss alternative treatment options if Mounjaro proves unsuitable.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.