Some patients taking Ozempic (semaglutide) for type 2 diabetes report noticing changes in body odour, though this is not listed as an official side effect in UK prescribing information. Whilst no direct causal link has been established in clinical trials, several physiological mechanisms related to the medication's effects—including metabolic changes from weight loss, altered digestion, and dietary modifications—may theoretically explain these anecdotal observations. Understanding why body odour might change during Ozempic treatment, and knowing practical management strategies, can help patients continue their diabetes therapy with confidence whilst addressing this concern appropriately.
Quick Answer: Ozempic (semaglutide) is not officially linked to body odour changes, but metabolic shifts from weight loss, gastrointestinal effects, and dietary modifications may theoretically contribute to anecdotal reports.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK specifically for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that helps regulate blood sugar levels and appetite.
The medication is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. Ozempic works through several mechanisms: it stimulates insulin secretion when blood glucose levels are elevated, suppresses the release of glucagon (a hormone that raises blood sugar), slows gastric emptying to reduce post-meal glucose spikes, and acts on appetite centres in the brain to promote satiety. These combined effects help improve glycaemic control and often lead to weight loss as a secondary benefit.
In the UK, Ozempic is prescribed according to NICE guidelines (NG28) for type 2 diabetes management, typically when metformin and other treatments have not achieved adequate blood sugar control. NICE recommends GLP-1 receptor agonists for people with a BMI ≥35 kg/m² (or lower in certain ethnic groups), or when obesity-related complications are present, or when insulin would have significant occupational implications. It's important to note that while Ozempic may cause weight loss, it is not licensed for weight management in the UK (Wegovy is the licensed semaglutide product for weight management).
The MHRA-approved starting dose is 0.25 mg weekly for 4 weeks (to minimise gastrointestinal side effects), then increased to 0.5 mg weekly. If necessary, the dose may be increased to 1 mg or 2 mg weekly after at least 4 weeks at each dose level.
Patients should be aware of important safety considerations, including risks of pancreatitis, gallbladder disease, and potential worsening of diabetic retinopathy (particularly with rapid improvement in blood glucose). Whilst Ozempic has proven effective for diabetes management, understanding how the medication works helps explain some of the bodily changes that can occur, including alterations in metabolism and digestion that may indirectly affect body odour.
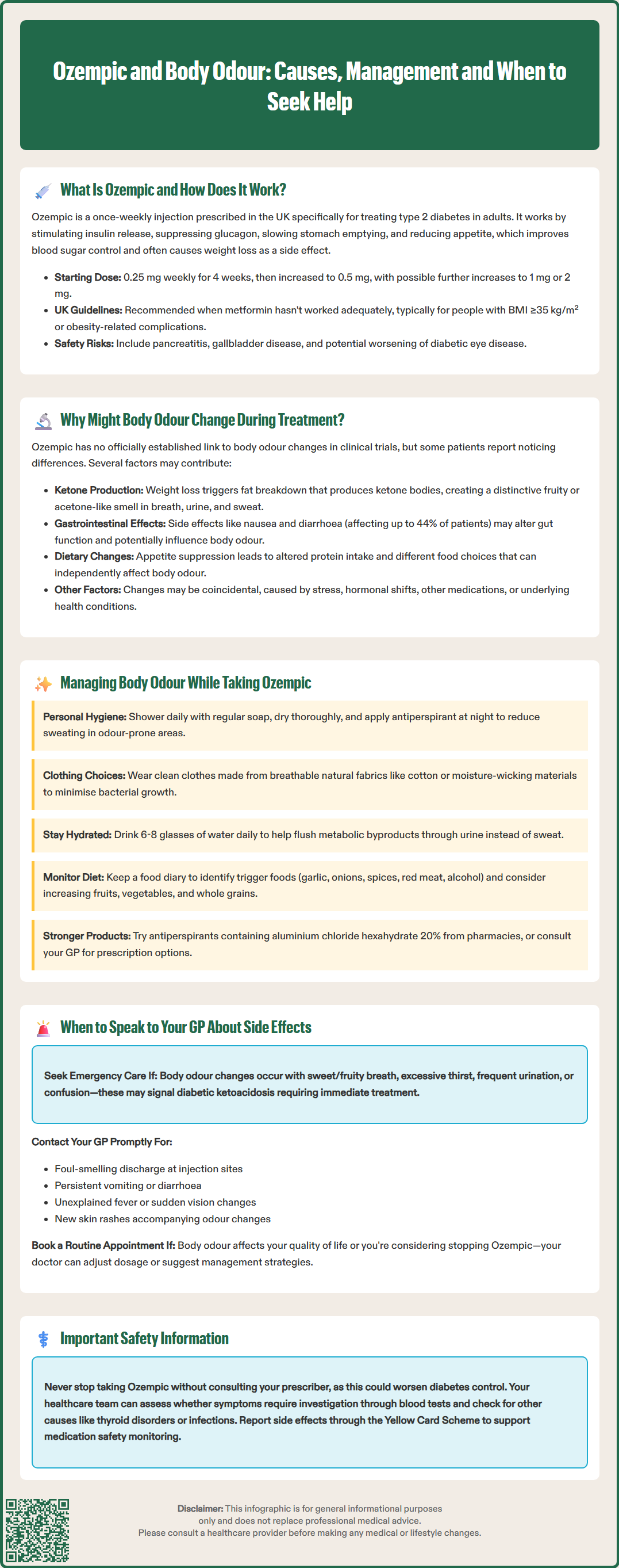
There is no official, direct link established between Ozempic and changes in body odour in clinical trials or the MHRA/emc Summary of Product Characteristics (SmPC). However, some patients report noticing differences in their body odour whilst taking semaglutide, and several physiological mechanisms may theoretically explain these anecdotal observations.
Metabolic changes represent the most plausible explanation. When Ozempic promotes weight loss, the body breaks down stored fat through a process called lipolysis. This metabolic shift can produce ketone bodies, which are released through breath, urine, and sweat, potentially creating a distinctive odour that some describe as fruity or acetone-like. This is particularly relevant for patients experiencing significant weight reduction. It's important to distinguish mild nutritional ketosis (generally benign) from diabetic ketoacidosis (a medical emergency), which is rare with GLP-1 receptor agonists alone but can occur if insulin doses are reduced too quickly.
Gastrointestinal effects are among the most common side effects of Ozempic, affecting up to 44% of patients in clinical trials. These include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. Altered digestion and gut transit time might hypothetically influence the gut microbiome, though evidence directly linking this to body odour changes is limited. Delayed gastric emptying, a therapeutic effect of the medication, might also contribute to digestive changes that could indirectly affect odour.
Dietary modifications often accompany Ozempic treatment. The medication's appetite-suppressing effects typically lead patients to eat less and make different food choices. Changes in protein intake, consumption of certain vegetables (particularly cruciferous varieties), or alterations in hydration status can all influence body odour. While increased sweating is not listed as a common side effect of semaglutide in the SmPC, patients taking Ozempic alongside insulin or sulfonylureas should be aware that sweating can be a symptom of hypoglycaemia.
It's important to note that body odour changes could also be coincidental or related to other factors such as stress, hormonal fluctuations, other medications, or underlying health conditions rather than directly caused by Ozempic itself.
If you notice changes in body odour whilst taking Ozempic, several practical strategies can help manage this concern whilst continuing your diabetes treatment.
Maintain excellent personal hygiene as your first line of defence:
Shower or bathe daily, paying particular attention to areas prone to sweating such as underarms, feet, and groin
Use regular soap and water (antibacterial soap is not usually necessary and may irritate skin with frequent use)
Ensure thorough drying after washing, as bacteria thrive in moist environments
Apply antiperspirant (which reduces sweating) rather than just deodorant, preferably at night when sweat glands are less active
Wear clean clothes daily, choosing natural, breathable fabrics like cotton or moisture-wicking materials
Dietary adjustments may prove beneficial. Stay well-hydrated by drinking 6–8 glasses of water daily (as recommended by the NHS), as this helps flush metabolic byproducts through urine rather than sweat. Consider keeping a food diary to identify whether specific foods (such as garlic, onions, spices, red meat, or alcohol) correlate with odour changes. Increasing your intake of fresh fruits, vegetables, and whole grains whilst moderating protein consumption may help.
Monitor your blood glucose levels as recommended by your diabetes care team. Ketone testing is not routinely needed unless you are unwell, have very high glucose levels, or experience symptoms such as excessive thirst or unusual fatigue. If you're concerned about ketones, discuss appropriate monitoring with your healthcare provider.
Review your medication routine with your pharmacist. Ensure you're storing Ozempic correctly and using proper injection technique, as these factors don't directly cause odour but ensure optimal medication effectiveness. Some patients find that the gradual dose escalation recommended for Ozempic helps their body adjust to metabolic changes more smoothly.
If simple measures don't resolve the issue, products containing aluminium chloride hexahydrate 20% (available from pharmacies) may be more effective than standard antiperspirants. For persistent problems, your GP can consider prescription options.
Whilst changes in body odour alone are not typically a medical emergency, certain circumstances warrant professional medical advice to ensure your safety and treatment effectiveness.
Seek urgent medical attention (call 999, go to A&E, or contact NHS 111) if:
Body odour changes are accompanied by a sweet, fruity breath smell, excessive thirst, frequent urination, fatigue, or confusion — these could indicate diabetic ketoacidosis (DKA), a serious complication requiring immediate treatment
You experience severe, persistent abdominal pain (especially radiating to the back) with or without vomiting, which could indicate pancreatitis
You develop severe pain in the upper right abdomen, fever, or yellowing of the skin/eyes, which might suggest gallbladder problems
Contact your GP promptly if:
You notice unusual or foul-smelling discharge from injection sites, which might suggest infection
Odour changes coincide with persistent gastrointestinal symptoms such as vomiting or diarrhoea that could lead to dehydration
You develop unexplained fever, night sweats, or unintentional weight loss beyond what's expected with treatment
You experience sudden changes in vision, particularly if you have pre-existing diabetic retinopathy
The odour is accompanied by skin changes, rashes, or other new symptoms
Arrange a routine appointment to discuss:
Persistent body odour concerns that affect your quality of life or confidence, even if not medically serious
Any side effects that make you consider stopping Ozempic, as your doctor may adjust your dose or suggest alternative management strategies
Questions about whether your symptoms are normal or require investigation
Your healthcare team can perform a comprehensive assessment including review of your diabetes control (HbA1c levels), kidney and liver function tests, and evaluation for other potential causes of odour changes such as thyroid disorders, infections, or medication interactions. They may also refer you to a dermatologist if a primary skin condition is suspected.
Do not stop taking Ozempic without speaking to your prescriber, as this could affect your diabetes control. The benefits of improved glycaemic management typically outweigh minor side effects, and your medical team can help you find solutions that allow you to continue treatment safely and comfortably. You can report any suspected side effects directly to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk), contributing to ongoing medication safety monitoring.
No direct link between Ozempic and body odour is established in clinical trials or UK prescribing information. However, metabolic changes from weight loss, gastrointestinal effects, and dietary modifications associated with the medication may theoretically contribute to odour changes reported anecdotally by some patients.
Maintain excellent personal hygiene, stay well-hydrated, use antiperspirants, wear breathable fabrics, and monitor your diet. If odour changes are accompanied by sweet breath, severe abdominal pain, or other concerning symptoms, seek urgent medical attention as these could indicate serious complications.
Do not stop Ozempic without consulting your prescriber, as this could compromise your diabetes control. Speak to your GP or diabetes care team about your concerns—they can help you find management strategies or adjust your treatment plan whilst maintaining effective glycaemic control.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.