
Does Ozempic make you hungry? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes that typically reduces appetite by mimicking natural hunger-regulating hormones. Most patients report decreased hunger and enhanced satiety whilst taking this medication. However, some individuals experience increased hunger, particularly during initial dose titration or due to blood glucose fluctuations. Understanding how Ozempic affects appetite, why responses vary, and when to seek medical advice ensures safe, effective diabetes management. This article explores the mechanisms behind Ozempic's appetite effects and provides practical guidance for managing unexpected hunger whilst on treatment.
Quick Answer: Ozempic typically reduces hunger rather than increasing it, though some individuals may experience increased appetite during initial treatment or due to blood glucose fluctuations.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Its primary mechanism of action involves mimicking the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
When administered, Ozempic binds to GLP-1 receptors in multiple areas of the body, including the pancreas, gastrointestinal tract, and importantly, the hypothalamus—the brain region responsible for regulating hunger and satiety. According to the Ozempic SmPC, the medication works by stimulating glucose-dependent insulin secretion, suppressing glucagon release, and slowing gastric emptying, which prolongs the feeling of fullness after meals. Many people report reduced appetite whilst taking Ozempic.
Clinical trials have demonstrated that semaglutide is associated with reduced appetite and decreased food intake for many patients. This appetite-suppressing effect is one of the reasons semaglutide (in higher doses marketed as Wegovy) has been approved for weight management in the UK. Research suggests the medication may enhance satiety signals and potentially affect food reward mechanisms, making it easier for many individuals to adhere to reduced-calorie diets.
However, individual responses to Ozempic can vary considerably. Whilst many patients report feeling less hungry, some individuals may experience different effects on their appetite. Understanding how Ozempic typically functions helps patients recognise what to expect and identify when their experience differs from the norm, which may warrant discussion with their healthcare provider.
It's important to note that hypoglycaemia (low blood sugar) risk with semaglutide alone is low, but this risk increases when used in combination with insulin or sulfonylureas.
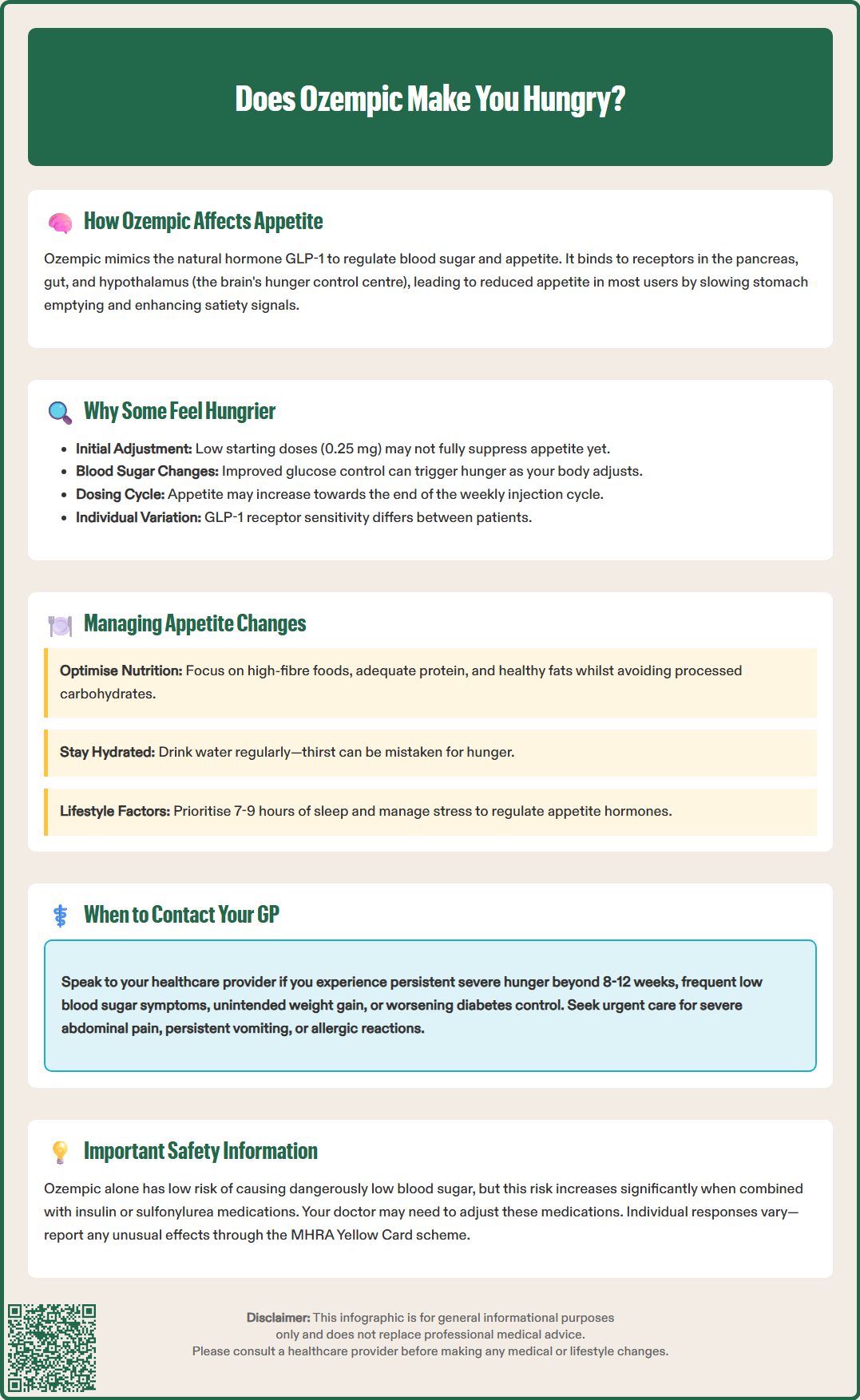
Although Ozempic is designed to reduce appetite, some people report increased hunger whilst taking the medication. This seemingly paradoxical response can occur for several reasons, and understanding these factors is important for both patients and clinicians.
Dosage and titration timing may play a significant role. Ozempic is typically initiated at 0.25 mg weekly for four weeks, then increased to 0.5 mg, with potential further increases to 1 mg or 2 mg depending on glycaemic control and tolerability. Some patients may experience increased hunger during the initial low-dose phase before the appetite-suppressing effects become fully established. Additionally, if the dose remains subtherapeutic for an individual's physiology, the expected appetite reduction may not materialise.
Blood glucose fluctuations represent another important consideration. As Ozempic improves glycaemic control in people with type 2 diabetes, some patients may experience relative hypoglycaemia—blood glucose levels that, whilst not dangerously low, are significantly lower than their previous baseline. This can trigger hunger signals as the body adapts to improved glucose regulation. It's important to note that hypoglycaemia is uncommon with semaglutide alone; the risk increases when combined with insulin or sulfonylureas, and doses of these medications may need review if hunger or hypoglycaemic symptoms occur.
Individual biological variation in GLP-1 receptor sensitivity, metabolism, and hormonal regulation means that not everyone responds identically to the medication. Factors such as concurrent medications, underlying health conditions, stress levels, sleep quality, and dietary composition can all influence appetite regulation. There is no official link establishing that Ozempic universally increases hunger; rather, these represent individual variations in treatment response that merit clinical attention and potential management adjustments.
Some patients may also notice appetite variations within the weekly dosing interval, with potential increases in hunger towards the end of the week before the next dose is due.
If you experience increased hunger whilst taking Ozempic, several evidence-based strategies can help manage this unexpected response whilst maintaining the medication's therapeutic benefits for diabetes control.
Dietary modifications form the cornerstone of appetite management. Focus on consuming:
High-fibre foods such as vegetables, pulses, and whole grains, which promote satiety and slow digestion
Adequate protein at each meal (lean meats, fish, eggs, dairy, or plant-based alternatives) to enhance fullness
Healthy fats in moderate amounts (nuts, seeds, avocado, olive oil) which may help with satiety, though be aware these could worsen gastrointestinal symptoms in some people taking GLP-1 medications
Regular meal timing to establish consistent eating patterns and prevent excessive hunger
Avoid highly processed foods, refined carbohydrates, and sugary items that can cause rapid blood glucose spikes and subsequent hunger. Staying well-hydrated is equally important, as thirst can sometimes be mistaken for hunger.
Monitor blood glucose as advised in your diabetes care plan. Routine self-monitoring is not universally recommended for all people with type 2 diabetes, but may be advised during medication adjustments, illness, or if you take insulin or medications with hypoglycaemia risk. If readings suggest hypoglycaemia or significant fluctuations, contact your healthcare provider, as adjustments to diabetes medications may be necessary.
If you experience symptoms of hypoglycaemia (shakiness, sweating, confusion, hunger), take 15-20g of fast-acting carbohydrate (e.g., glucose tablets, fruit juice), recheck after 15 minutes, and follow with a longer-acting carbohydrate if needed. Seek medical advice if hypoglycaemia occurs repeatedly.
Lifestyle factors significantly influence appetite regulation. Prioritise:
Adequate sleep (7–9 hours nightly), as sleep deprivation increases hunger hormones
Stress management through relaxation techniques, as chronic stress affects appetite regulation
Regular physical activity, which can help regulate appetite hormones and improve insulin sensitivity
These strategies should be implemented gradually and monitored for effectiveness. If increased hunger persists despite these interventions, medical review is warranted to ensure optimal treatment outcomes.
Whilst some appetite variation is normal when starting Ozempic, certain situations warrant prompt discussion with your GP or diabetes specialist nurse to ensure safe and effective treatment.
Contact your healthcare provider if you experience:
Persistent or severe hunger that doesn't improve after the initial titration period (typically 8–12 weeks)
Unintended weight gain whilst taking Ozempic, particularly if accompanied by increased appetite
Symptoms of hypoglycaemia including shakiness, sweating, confusion, or palpitations, especially if occurring frequently
Difficulty managing your diabetes with worsening HbA1c levels or consistently elevated blood glucose readings
Significant changes in eating patterns or concerns about disordered eating behaviours
Seek urgent medical attention if you develop:
Severe, persistent abdominal pain (with or without vomiting) which could indicate pancreatitis
Symptoms of gallstones such as pain in the upper right abdomen, particularly after eating
Persistent vomiting leading to dehydration
Signs of allergic reaction such as rash, swelling, or difficulty breathing
Your GP may need to review your treatment plan, which could involve adjusting the Ozempic dose, evaluating the timing of administration, or assessing interactions with other medications. If you're also taking insulin or sulfonylureas and experiencing hunger or hypoglycaemia symptoms, these medications may need dose adjustment.
NICE guidance (NG28) recommends regular review of patients on GLP-1 receptor agonists, typically at around 6 months, to assess treatment response. NICE advises continuing treatment only if there is a clinically meaningful HbA1c reduction (for example ≥11 mmol/mol [1%]) and weight loss of at least 3% of initial body weight. However, don't wait for a scheduled appointment if you have concerns—early intervention can prevent complications.
Your healthcare team can provide personalised advice based on your individual circumstances, medical history, and treatment goals. They may refer you to a dietitian for specialist nutritional support or adjust your overall diabetes management strategy.
If you suspect you're experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Increased hunger on Ozempic may occur during initial low-dose titration before appetite-suppressing effects fully establish, or due to relative hypoglycaemia as your blood glucose improves. Individual biological variation in GLP-1 receptor sensitivity can also affect appetite response, warranting discussion with your healthcare provider if hunger persists.
Ozempic alone rarely causes hypoglycaemia, but the risk increases when combined with insulin or sulfonylureas. Some patients experience relative hypoglycaemia—blood glucose lower than their previous baseline—which can trigger hunger signals as the body adapts to improved glucose control.
Contact your GP if you experience persistent severe hunger beyond the initial 8–12 week titration period, unintended weight gain, frequent hypoglycaemia symptoms, or difficulty managing your diabetes. Your healthcare provider may need to adjust your Ozempic dose or review other diabetes medications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.