
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone that plays a vital role in regulating blood glucose, appetite, and metabolic health. Produced in the gut after eating, GLP-1 stimulates insulin release, suppresses excess glucose production, and promotes feelings of fullness. Whilst pharmaceutical GLP-1 receptor agonists have gained prominence for managing type 2 diabetes and weight, many people seek natural ways to enhance their body's own GLP-1 production. Evidence-based dietary choices, lifestyle modifications, and behavioural strategies can support natural GLP-1 secretion, offering a foundation for long-term metabolic health without medication. This article explores practical, clinically informed approaches to optimising your natural GLP-1 response.
Quick Answer: You can increase GLP-1 naturally by consuming protein-rich foods, dietary fibre, healthy fats, maintaining regular meal patterns, exercising consistently, and ensuring adequate sleep quality.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) is a naturally occurring hormone produced primarily by specialised L-cells in the lining of your small intestine and colon. This incretin hormone plays a crucial role in regulating blood glucose levels, appetite, and overall metabolic health. When you eat, GLP-1 is released into your bloodstream, where it performs several vital functions that influence how your body processes food and manages energy.
The primary actions of GLP-1 include stimulating insulin secretion from pancreatic beta cells in response to elevated blood glucose (importantly, this insulin release is glucose-dependent, reducing hypoglycaemia risk), suppressing glucagon release (which prevents the liver from producing excess glucose), and slowing gastric emptying. This coordinated response helps maintain stable blood sugar levels after meals. Additionally, GLP-1 acts on receptors in the brain's appetite centres, particularly the hypothalamus, promoting feelings of satiety and reducing food intake.
Why GLP-1 matters for metabolic health cannot be overstated. Adequate GLP-1 activity is associated with better glycaemic control, healthy weight management, and potential metabolic benefits. Research suggests that individuals with type 2 diabetes often have impaired GLP-1 secretion or response, contributing to poor glucose regulation. Some preclinical studies suggest GLP-1 may have beneficial effects on pancreatic beta cells, though long-term preservation of function in humans remains unproven.
Understanding how to naturally optimise your body's GLP-1 production through diet, lifestyle, and behavioural modifications offers an evidence-based approach to supporting metabolic health. Whilst pharmaceutical GLP-1 receptor agonists (such as semaglutide and liraglutide) have gained attention for diabetes and weight management, enhancing your natural GLP-1 response through physiological means provides a foundation for long-term health without medication.
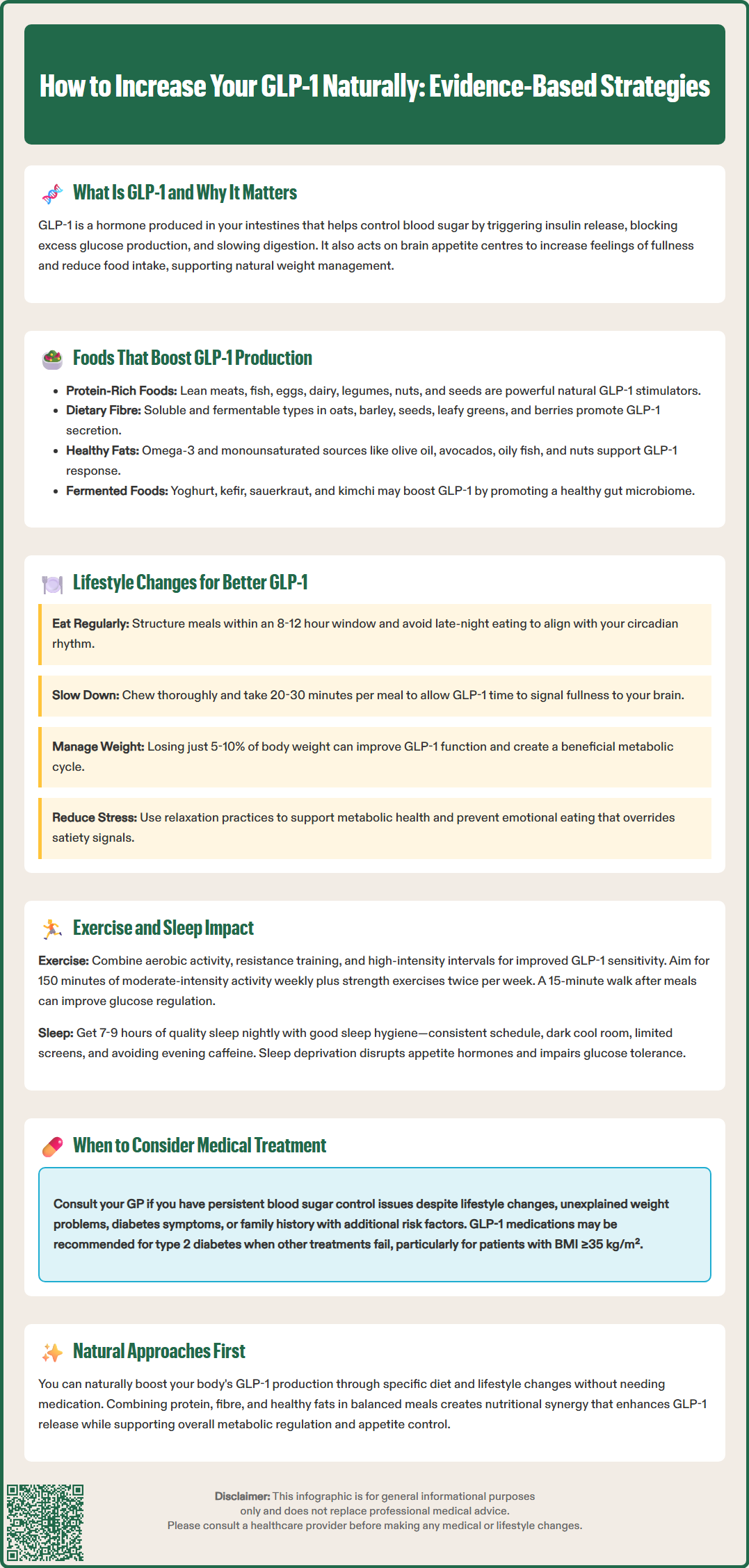
Dietary choices significantly influence GLP-1 secretion, with certain nutrients and food components demonstrating particularly strong effects on incretin hormone release. Understanding which foods stimulate GLP-1 can help you structure meals that naturally enhance metabolic regulation and appetite control.
Protein-rich foods are among the most potent natural GLP-1 stimulators. Studies have shown that dietary protein triggers substantial GLP-1 release, with whey protein demonstrating especially pronounced effects. Good protein sources include:
Lean meats, poultry, and fish
Eggs and dairy products
Legumes such as lentils, chickpeas, and beans
Nuts and seeds
Dietary fibre, particularly soluble and fermentable types, promotes GLP-1 secretion through multiple mechanisms. When gut bacteria ferment fibre in the colon, they produce short-chain fatty acids (SCFAs) such as butyrate, propionate, and acetate, which directly stimulate L-cells to release GLP-1. Excellent fibre sources include oats, barley, flaxseeds, chia seeds, vegetables (especially leafy greens and cruciferous varieties), and fruits such as berries and apples.
Healthy fats may support GLP-1 response, though evidence is mixed and context-dependent. Foods containing omega-3 fatty acids and monounsaturated fats such as olive oil, avocados, oily fish (salmon, mackerel, sardines), and nuts can be included as part of a balanced diet aligned with the NHS Eatwell Guide.
Fermented foods containing probiotics may indirectly support GLP-1 production by promoting a healthy gut microbiome, though robust human evidence remains limited. Yoghurt, kefir, sauerkraut, and kimchi can contribute to beneficial bacterial populations that may help enhance incretin hormone secretion. Combining these food groups in balanced meals—such as grilled salmon with quinoa and roasted vegetables—creates nutritional synergy that can support natural GLP-1 release whilst providing comprehensive nutrition.
Beyond specific foods, broader lifestyle patterns may influence GLP-1 secretion and function. Implementing evidence-based behavioural modifications can create an internal environment that supports incretin hormone activity and metabolic health.
Meal timing and eating patterns may affect GLP-1 dynamics, though evidence is still emerging. Some research suggests that eating regular, structured meals rather than constant grazing may support GLP-1 response. There is limited evidence that time-restricted eating (consuming food within a consistent 8–12 hour window) might influence incretin hormone secretion, though more research is needed. Avoiding late-night eating aligns with your body's circadian rhythm, potentially supporting hormonal responses including GLP-1 release.
Mindful eating practices can complement natural GLP-1 effects. Eating slowly and chewing thoroughly allows more time for GLP-1 to signal satiety to your brain, potentially reducing overall food intake. Studies show that rapid eating is associated with reduced satiety hormone responses and increased risk of obesity and metabolic syndrome. Taking time to complete a meal (around 20–30 minutes is a practical strategy) gives your incretin hormones adequate time to exert their appetite-suppressing effects.
Weight management itself influences GLP-1 function. Excess adiposity, particularly visceral fat, is associated with impaired incretin effect in type 2 diabetes. Even modest weight loss (5–10% of body weight) can improve metabolic hormone dynamics. This creates a beneficial cycle: lifestyle changes that promote GLP-1 release support weight management, which in turn may enhance GLP-1 function.
Stress reduction may also play a role, as chronic psychological stress and elevated cortisol levels can impair metabolic hormone regulation. Whilst there is no definitive link established between stress management techniques and GLP-1 specifically, practices such as meditation, yoga, and adequate relaxation support overall metabolic health. Managing stress also helps prevent emotional eating patterns that override natural satiety signals, including those mediated by GLP-1.
Physical activity and sleep quality represent two critical lifestyle factors that influence metabolic health, with varying effects on GLP-1 and other regulatory hormones.
Exercise and GLP-1 dynamics present a complex relationship. Acute exercise can alter gut hormone levels, with evidence on GLP-1 being mixed—several studies show increases in GLP-1 with exercise, while others show minimal changes or decreases. However, regular physical activity improves insulin sensitivity and metabolic health, which may enhance the body's responsiveness to GLP-1 over time. Studies suggest that consistent exercise training supports overall incretin hormone function and metabolic regulation.
Different exercise modalities offer complementary benefits:
Aerobic exercise (walking, cycling, swimming) performed regularly improves overall metabolic health and may enhance GLP-1 sensitivity
Resistance training builds muscle mass, which increases metabolic rate and improves glucose disposal
High-intensity interval training (HIIT) has shown promise for improving insulin sensitivity and metabolic markers
The timing of exercise relative to meals may matter. Post-meal physical activity (such as a 15-minute walk after eating) can improve glucose regulation, though these benefits may occur independently of specific GLP-1 changes. The NHS recommends at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous activity weekly, plus strength exercises on two or more days.
Sleep quality and duration profoundly affect metabolic hormones, including those regulating appetite and glucose metabolism. Sleep deprivation disrupts multiple hormonal systems, increasing ghrelin (hunger hormone) whilst reducing leptin (satiety hormone). Whilst direct evidence linking sleep specifically to GLP-1 is still emerging, poor sleep is associated with impaired glucose tolerance and increased appetite—conditions that GLP-1 normally helps regulate.
Aim for 7–9 hours of quality sleep nightly to support optimal metabolic function. Sleep hygiene practices include maintaining consistent sleep-wake times, creating a dark and cool sleeping environment, limiting screen exposure before bed, and avoiding caffeine and large meals in the evening. Adequate sleep supports the body's natural circadian rhythms, which influence hormone secretion patterns throughout the day.
Whilst natural approaches to enhancing GLP-1 provide valuable metabolic benefits, certain clinical situations warrant consideration of pharmaceutical GLP-1 receptor agonists. Understanding when lifestyle modifications alone may be insufficient helps ensure appropriate and timely medical intervention.
NICE guidelines recommend GLP-1 receptor agonists for specific patient populations with type 2 diabetes. These medications (including semaglutide, dulaglutide, and liraglutide) are typically considered when:
Metformin and other oral medications have not achieved adequate glycaemic control
The patient has a BMI ≥35 kg/m² (or lower thresholds, typically by around 2.5 kg/m², for people of certain ethnic backgrounds including South Asian)
Weight loss would benefit other obesity-related comorbidities
Insulin therapy is being considered but would have significant occupational implications or weight gain is a concern
Continuation criteria apply: for example, treatment should reduce HbA1c by at least 11 mmol/mol (1.0%) and weight by at least 3% at 6 months to be continued.
For weight management in people without diabetes, NICE recommends considering semaglutide 2.4 mg (Wegovy) for adults with a BMI ≥35 kg/m² (or lower thresholds for certain ethnic groups) and at least one weight-related comorbidity. Treatment must be provided by specialist weight management services, is limited to a maximum of 2 years, and requires specific weight loss targets to continue. It should be part of a comprehensive weight management programme including dietary modification, physical activity, and behavioural support.
You should consult your GP if you experience:
Persistent difficulty managing blood glucose despite lifestyle modifications
Unexplained weight gain or inability to lose weight despite sustained efforts
Symptoms of diabetes (excessive thirst, frequent urination, unexplained fatigue)
Family history of type 2 diabetes combined with other risk factors
Important safety considerations: GLP-1 receptor agonists are prescription medications with potential adverse effects, most commonly gastrointestinal symptoms (nausea, vomiting, diarrhoea). Cautions include history of pancreatitis, gallbladder disease, and diabetic retinopathy (particularly with semaglutide). When combined with insulin or sulfonylureas, dose adjustments may be needed to prevent hypoglycaemia. Pregnancy is a contraindication for semaglutide 2.4 mg (Wegovy). Your healthcare provider will assess your individual circumstances to determine whether GLP-1 therapy is appropriate. Report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Natural GLP-1 enhancement through diet and lifestyle remains valuable even when medication is prescribed, as these approaches work synergistically to optimise metabolic health.
Protein-rich foods (lean meats, fish, eggs, legumes), dietary fibre (oats, vegetables, berries), healthy fats (oily fish, nuts, olive oil), and fermented foods (yoghurt, kefir) stimulate natural GLP-1 production. Combining these in balanced meals creates nutritional synergy that supports incretin hormone release.
Acute exercise effects on GLP-1 are mixed, but regular physical activity improves insulin sensitivity and may enhance GLP-1 responsiveness over time. The NHS recommends at least 150 minutes of moderate-intensity activity weekly plus strength exercises for optimal metabolic health.
NICE recommends GLP-1 receptor agonists for type 2 diabetes when metformin and other oral medications fail to achieve adequate glycaemic control, particularly with BMI ≥35 kg/m² or weight-related comorbidities. Consult your GP if you experience persistent difficulty managing blood glucose or unexplained weight issues despite lifestyle modifications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.