Rybelsus making me sick is a common concern among patients prescribed this oral GLP-1 receptor agonist for type 2 diabetes. Nausea, vomiting, and stomach discomfort affect many people starting Rybelsus (semaglutide), particularly during the first few weeks of treatment. These gastrointestinal side effects occur because the medication slows gastric emptying and activates receptors in areas of the brain that control nausea. Whilst these symptoms are usually temporary and improve as your body adapts, understanding why they occur and how to manage them can significantly improve your treatment experience. This article explains the mechanisms behind Rybelsus-related nausea, practical strategies to reduce symptoms, and when to seek medical advice.
Quick Answer: Rybelsus commonly causes nausea and stomach problems because it slows gastric emptying and activates brain receptors that trigger nausea, with symptoms typically improving after the first month of treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which is released from the gut after eating. This medication enhances insulin secretion when blood glucose levels are elevated, suppresses glucagon release, and importantly, slows gastric emptying—the rate at which food leaves the stomach.
The mechanism that makes Rybelsus effective for glycaemic control is also responsible for many of its gastrointestinal side effects. By delaying gastric emptying, Rybelsus causes food to remain in the stomach for longer periods, which can trigger feelings of fullness, bloating, and nausea. Additionally, GLP-1 receptors are present in areas of the brain that control appetite and nausea, particularly in the area postrema—a region involved in the vomiting reflex. Activation of these receptors can directly stimulate nausea and, in some cases, vomiting.
It is important to understand that feeling sick when taking Rybelsus is a recognised and common adverse effect, not an indication of treatment failure. According to the UK Summary of Product Characteristics (SmPC), gastrointestinal symptoms are the most frequently reported side effects, particularly during the initial weeks of treatment. Most patients experience a reduction in these symptoms over time as the body adapts to the medication. However, for some individuals, nausea can persist or become severe enough to warrant dose adjustment or alternative treatment options.
While rare, it's important to be aware that severe, persistent abdominal pain (especially if radiating to the back) with or without vomiting could indicate pancreatitis, a serious condition requiring immediate medical attention and discontinuation of Rybelsus. Similarly, symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice) also require prompt medical assessment.
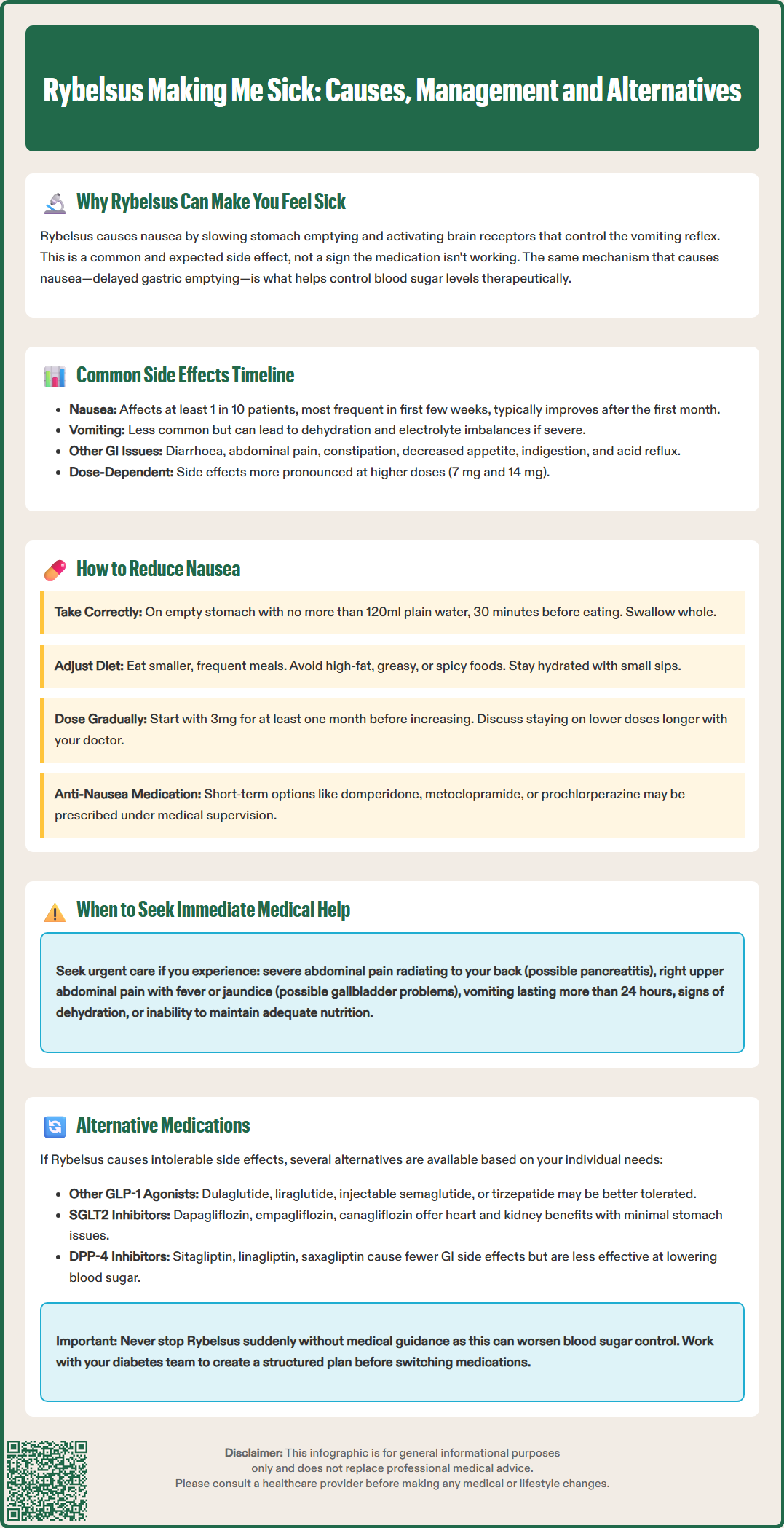
Nausea is the most commonly reported side effect of Rybelsus, classified as 'very common' (affecting ≥1/10 patients) in the UK SmPC. This symptom typically begins within the first few weeks of starting treatment or after a dose increase. The nausea is usually mild to moderate in severity and tends to improve after the first month, though some patients continue to experience intermittent symptoms throughout treatment.
Vomiting occurs less frequently than nausea but is still classified as 'common' (affecting ≥1/100 to <1/10 patients). Vomiting is more likely to occur during the dose escalation phase and may be triggered by large meals or fatty foods. Persistent vomiting can lead to dehydration and electrolyte imbalances, and in severe cases, may contribute to acute kidney injury. It is important to maintain adequate fluid intake and seek medical advice if vomiting becomes frequent or severe.
Other gastrointestinal problems commonly associated with Rybelsus include:
Diarrhoea – classified as 'common' in the SmPC
Abdominal pain or discomfort – classified as 'common'
Constipation – classified as 'common'
Decreased appetite – which can contribute to improved glycaemic control
Dyspepsia (indigestion) – classified as 'common'
Gastro-oesophageal reflux – classified as 'common'
These side effects are generally dose-dependent, meaning they are more pronounced at higher doses (7 mg and 14 mg) compared to the starting dose of 3 mg. According to the SmPC, patients should be monitored during dose escalation, and dose increases should only occur after at least one month at the current dose to allow for gastrointestinal adaptation.
It's worth noting that when Rybelsus is used in combination with insulin or sulfonylureas (such as gliclazide), there is an increased risk of hypoglycaemia. Your healthcare provider may need to reduce the dose of these medications when starting Rybelsus to minimise this risk.
There are several evidence-based strategies that can help minimise nausea and improve tolerability when taking Rybelsus. Firstly, it is essential to take the medication correctly. Rybelsus must be taken on an empty stomach with no more than 120 ml (half a glass) of plain water, at least 30 minutes before the first food, drink, or other oral medications of the day. The tablet should be swallowed whole; do not split, crush, or chew it. Taking it with food, other beverages, or insufficient water significantly reduces absorption and effectiveness.
Dietary modifications can substantially reduce nausea:
Eat smaller, more frequent meals rather than large portions
Avoid high-fat, greasy, or spicy foods, which delay gastric emptying further
Limit foods with strong odours that may trigger nausea
Stay well-hydrated throughout the day with small, frequent sips of water
Avoid lying down immediately after eating
Consider bland, easily digestible foods such as toast, crackers, or rice during periods of nausea
Timing and dose escalation are critical. The standard dosing schedule begins with 3 mg once daily for at least one month before increasing to 7 mg, and then to 14 mg if needed. Some patients benefit from remaining on the lower dose for longer periods to allow better gastrointestinal adaptation. Discuss with your GP or diabetes specialist nurse whether a slower titration schedule might be appropriate for you.
If nausea persists despite these measures, anti-emetic medications may be considered for short-term use under medical supervision. Options include:
Domperidone: Only at the lowest effective dose and for a maximum of one week. Not suitable for patients with cardiac conditions or those taking medications that prolong the QT interval or strong CYP3A4 inhibitors.
Metoclopramide: For short-term use only (maximum 5 days) due to risk of neurological side effects.
Prochlorperazine: May cause drowsiness and anticholinergic effects.
Some patients find that ginger supplements or acupressure wristbands provide symptomatic relief, though evidence for these approaches is limited.
When to seek medical advice: Contact your GP or diabetes team immediately if you experience severe, persistent abdominal pain (especially if radiating to the back), as this could indicate pancreatitis. Also seek prompt medical attention for severe or persistent vomiting (more than 24 hours), signs of dehydration (dark urine, dizziness, reduced urination), or if nausea significantly impacts your ability to maintain adequate nutrition. If you cannot contact your GP, call NHS 111 or attend an urgent care centre if symptoms are severe.
If gastrointestinal side effects remain intolerable despite dose adjustment and supportive measures, several alternative treatment options are available for type 2 diabetes management. The choice of alternative depends on individual factors including glycaemic control, weight, cardiovascular risk, renal function, and patient preference.
Other GLP-1 receptor agonists may be considered, though they share a similar side effect profile. Injectable formulations such as dulaglutide, liraglutide, exenatide or injectable semaglutide have different pharmacokinetic properties and some patients may find them better tolerated, though individual responses vary. Weekly injections may provide different side effect patterns compared to daily oral Rybelsus. Tirzepatide, a dual GIP/GLP-1 receptor agonist, is another option where appropriate. NICE guidance (NG28) supports the use of GLP-1 receptor agonists in patients with inadequate glycaemic control on metformin and other oral agents, particularly in specific patient groups.
SGLT2 inhibitors such as dapagliflozin, empagliflozin, or canagliflozin represent an alternative class with cardiovascular and renal benefits. These medications work by increasing urinary glucose excretion and are generally well-tolerated gastrointestinally. However, they carry different risks including genital infections and, rarely, diabetic ketoacidosis. NICE recommends SGLT2 inhibitors for patients with type 2 diabetes, particularly those with established cardiovascular disease or chronic kidney disease.
DPP-4 inhibitors (gliptins) such as sitagliptin, linagliptin, or saxagliptin offer a milder glucose-lowering effect with minimal gastrointestinal side effects. Whilst less effective than GLP-1 agonists for HbA1c lowering, they are well-tolerated and may be appropriate for patients who cannot tolerate Rybelsus.
Other options include insulin therapy (if glycaemic targets are not met with oral agents), pioglitazone (though weight gain is common), or optimising existing metformin therapy. A combination approach using lower doses of multiple agents may improve tolerability whilst maintaining glycaemic control.
Your diabetes healthcare team will conduct a comprehensive review considering your HbA1c, weight, cardiovascular risk factors, renal function, and treatment preferences to identify the most appropriate alternative. It is important not to stop Rybelsus abruptly without medical guidance, as this may lead to deterioration in blood glucose control. A structured treatment plan should be agreed before discontinuing any diabetes medication.
If you experience side effects from Rybelsus or any medication, you can report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Nausea from Rybelsus typically begins within the first few weeks of starting treatment and usually improves after the first month as your body adapts to the medication. Some patients experience intermittent symptoms throughout treatment, particularly after dose increases.
Anti-emetic medications such as domperidone or metoclopramide may be prescribed for short-term use under medical supervision to manage persistent nausea. Always consult your GP or diabetes specialist before taking any anti-sickness medication alongside Rybelsus.
Seek immediate medical attention if you experience severe, persistent abdominal pain (especially radiating to the back), persistent vomiting for more than 24 hours, signs of dehydration, or symptoms of gallbladder disease such as right upper quadrant pain, fever, or jaundice. Contact your GP or call NHS 111 if symptoms are severe.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.