
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed for weight management in the UK, but many patients experience burping and flatulence during treatment. These digestive side effects occur because Saxenda slows gastric emptying and alters gut motility—mechanisms that contribute to weight loss but can cause uncomfortable gas symptoms. Whilst these effects are common, particularly during the first few weeks of treatment, they typically improve as your body adjusts to the medication. Understanding why these symptoms occur and how to manage them effectively can help you continue treatment more comfortably.
Quick Answer: Saxenda causes burping and flatulence by slowing gastric emptying and altering gastrointestinal motility, which are therapeutic mechanisms that also lead to gas accumulation and belching.
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities. It is also authorised for weight management in adolescents aged ≥12 years weighing >60 kg. The medication works by mimicking the natural hormone GLP-1, which regulates appetite and food intake through several mechanisms in the body.
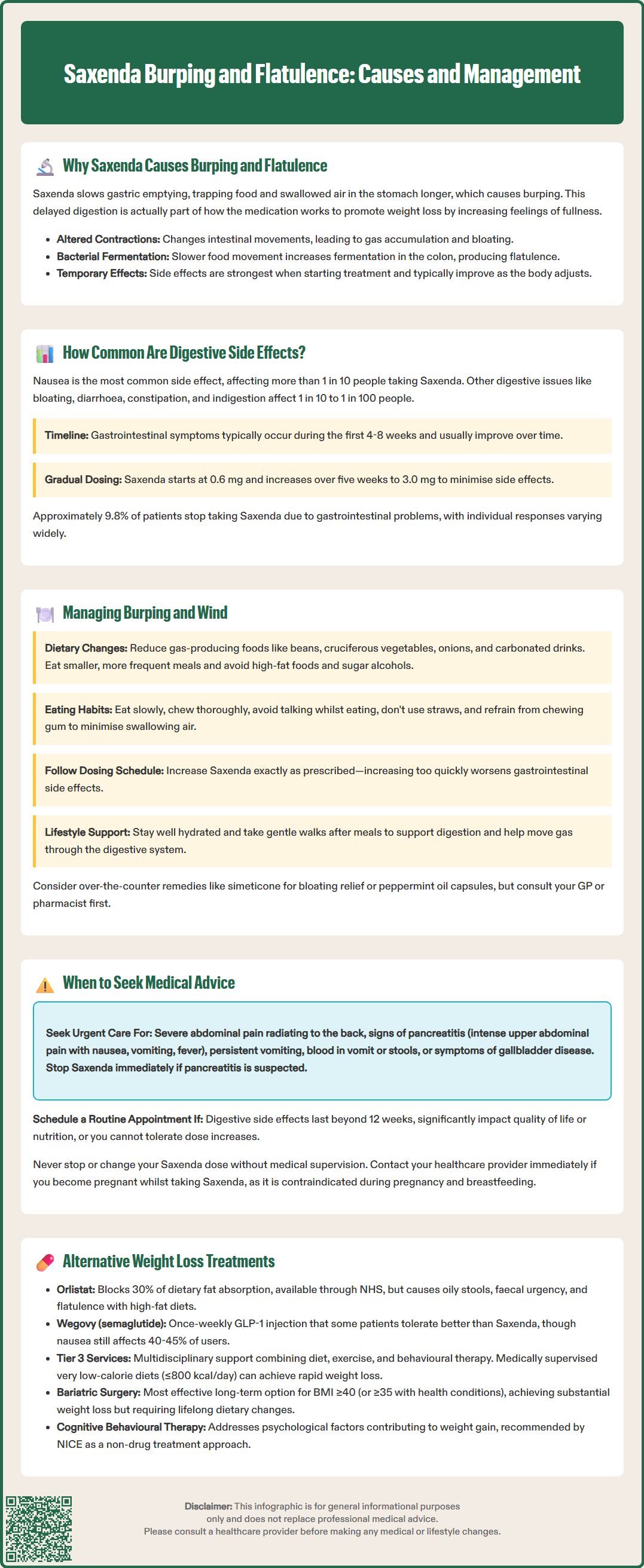
The primary reason Saxenda causes burping and flatulence relates to its effect on gastric emptying . Liraglutide significantly slows the rate at which food moves from the stomach into the small intestine. This delayed gastric emptying is actually one of the therapeutic mechanisms that contributes to weight loss, as it promotes feelings of fullness and satiety. However, when food remains in the stomach for longer periods, it can lead to belching (eructation) due to retained contents and swallowed air.
Additionally, Saxenda affects gastrointestinal motility throughout the digestive tract. The medication can alter the normal rhythmic contractions of the intestines, potentially leading to gas accumulation and bloating. When food moves more slowly through the intestines, this can increase bacterial fermentation in the colon, resulting in flatulence.
These gastrointestinal effects are dose-dependent and typically most pronounced during the initial titration phase of treatment when the body is adjusting to the medication. Most patients find these symptoms improve with continued treatment as the body adapts to the medication's effects.
Gastrointestinal side effects are among the most frequently reported adverse reactions with Saxenda treatment. According to the MHRA-approved Summary of Product Characteristics (SmPC) and clinical trial data, digestive symptoms affect a substantial proportion of patients, particularly during the early stages of therapy.
Nausea is the most common gastrointestinal side effect, classified as 'very common' (affecting more than 1 in 10 people). Other digestive symptoms are classified as 'common' (affecting between 1 in 10 and 1 in 100 people), including:
Flatulence
Eructation (burping)
Abdominal distension and bloating
Diarrhoea
Constipation
Dyspepsia (indigestion)
These symptoms are most common during the first 4-8 weeks of treatment, with the majority of patients experiencing improvement over time as the body adapts to the medication.
The frequency and severity of these side effects are closely linked to the dose escalation schedule. Saxenda is initiated at 0.6 mg daily and gradually increased over five weeks to the maintenance dose of 3.0 mg daily. This titration approach is specifically designed to improve gastrointestinal tolerability, though some patients still experience significant symptoms.
Clinical trials show that approximately 9.8% of patients discontinue Saxenda treatment due to gastrointestinal adverse events. Individual variation in response is considerable, with some patients experiencing minimal digestive upset whilst others find the symptoms more troublesome.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereSeveral evidence-based strategies can help minimise burping and flatulence whilst taking Saxenda. These approaches focus on dietary modifications, eating behaviours, and lifestyle adjustments that work synergistically with the medication.
Dietary modifications are particularly effective:
Reduce gas-producing foods: Temporarily limit beans, lentils, cruciferous vegetables (broccoli, cauliflower, cabbage), onions, and carbonated beverages
Eat smaller, more frequent meals: This approach works with Saxenda's mechanism by preventing stomach overload
Avoid high-fat foods: Fatty meals delay gastric emptying further, potentially exacerbating symptoms
Limit polyols: Sorbitol, mannitol, xylitol and other polyols found in sugar-free products can increase gas production
Keep a food diary: Identify personal trigger foods that worsen symptoms
Eating behaviour adjustments can significantly reduce air swallowing (aerophagia):
Eat slowly and chew food thoroughly
Avoid talking whilst eating
Don't use straws for drinking
Refrain from chewing gum
Ensure dentures fit properly if applicable
Practical management strategies include:
Maintain the prescribed titration schedule: Never increase the dose faster than recommended, as this increases gastrointestinal side effects
Stay well hydrated: Adequate fluid intake supports digestive function
Regular gentle exercise: Walking after meals can help move gas through the digestive system
Consider probiotics: Whilst evidence is limited, some patients report benefit from probiotic supplements, though you should discuss this with your GP or pharmacist first
Over-the-counter remedies such as simeticone (activated dimeticone) may provide symptomatic relief for bloating and trapped wind. Peppermint oil capsules are another option that some patients find helpful, though these may worsen heartburn in susceptible individuals. Always inform your prescriber about any additional medications or supplements you're taking to avoid potential interactions.
Whilst burping and flatulence are generally benign side effects of Saxenda, certain symptoms warrant prompt medical attention. It is crucial to distinguish between expected, manageable side effects and signs of potentially serious complications.
Contact your GP or prescribing clinician urgently if you experience:
Severe or persistent abdominal pain, particularly if it radiates to the back or is accompanied by vomiting
Signs of pancreatitis: intense upper abdominal pain, nausea, vomiting, and fever (this is a rare but serious adverse effect of GLP-1 receptor agonists)
Persistent vomiting that prevents you from keeping down food or fluids, risking dehydration
Blood in vomit or stools, which could indicate gastrointestinal bleeding
Severe diarrhoea lasting more than 48 hours, particularly if accompanied by dehydration symptoms
Symptoms of gallbladder disease: pain in the upper right abdomen, particularly after eating fatty foods, along with nausea or jaundice
If pancreatitis is suspected, stop Saxenda immediately and seek urgent medical review; do not restart unless pancreatitis has been ruled out.
Arrange a routine appointment if:
Digestive side effects persist beyond 12 weeks without improvement
Symptoms significantly impact your quality of life or ability to maintain adequate nutrition
You're unable to tolerate the dose escalation schedule
You experience unexplained weight loss beyond expected therapeutic effects
New or worsening symptoms develop after the initial adjustment period
Consider discontinuation and medical review if gastrointestinal symptoms are severe enough to affect your daily activities or nutritional intake. Your prescriber may recommend temporarily reducing the dose, pausing treatment, or considering alternative weight management options. Do not stop or change your dose without medical advice; people with diabetes may need their medicines adjusted.
Saxenda is contraindicated during pregnancy and breastfeeding. If you become pregnant while taking Saxenda, contact your healthcare provider immediately.
You can report any suspected side effects directly to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk, contributing to ongoing medication safety monitoring.
For patients who cannot tolerate Saxenda's gastrointestinal side effects, several alternative evidence-based weight management options are available, each with different side effect profiles.
Pharmacological alternatives include:
Orlistat is available through the NHS for weight management. It works by inhibiting pancreatic lipase, reducing dietary fat absorption by approximately 30%. Whilst it avoids the upper gastrointestinal effects of Saxenda, orlistat commonly causes oily stools, faecal urgency, and flatulence with discharge, particularly when dietary fat intake is high. NICE recommends orlistat for adults with BMI ≥30 kg/m² (or ≥28 kg/m² with comorbidities) alongside dietary modification.
Wegovy (semaglutide 2.4 mg) is another GLP-1 receptor agonist recently licensed in the UK and recommended by NICE (TA875) for use in specialist weight management services for eligible patients. Whilst it shares a similar mechanism to Saxenda, some patients tolerate it differently due to its once-weekly dosing schedule. However, gastrointestinal side effects remain very common, with nausea affecting approximately 40-45% of users and overall gastrointestinal adverse events occurring in the majority of patients in clinical trials.
Naltrexone/bupropion (Mysimba) is licensed in the UK but not routinely recommended by NICE for NHS use.
Non-pharmacological approaches recommended by NICE include:
Tier 3 weight management services: Multidisciplinary programmes combining dietary advice, physical activity support, and behavioural interventions
Very low-calorie diets (≤800 kcal/day): Medically supervised, time-limited programmes, particularly effective for rapid weight loss in people with type 2 diabetes
Cognitive behavioural therapy (CBT): Addresses psychological factors contributing to weight gain
Bariatric surgery represents the most effective long-term weight loss intervention for eligible patients. NICE recommends considering surgery for adults with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities) when non-surgical measures have been unsuccessful. For people with recent-onset type 2 diabetes, surgery may be considered at lower BMI thresholds (30-34.9 kg/m²). Lower BMI thresholds may also apply for people from certain ethnic groups. Procedures such as gastric bypass or sleeve gastrectomy achieve substantial weight loss but carry surgical risks and require lifelong dietary modifications.
Discuss these alternatives with your GP or specialist weight management service to determine the most appropriate approach based on your individual circumstances, medical history, and treatment goals.
Burping and flatulence are most common during the first 4–8 weeks of Saxenda treatment and typically improve as your body adapts to the medication. Most patients experience significant reduction in these symptoms with continued use.
Over-the-counter remedies such as simeticone (activated dimeticone) may provide symptomatic relief for bloating and trapped wind. Always inform your prescriber about any additional medications or supplements you're taking to avoid potential interactions.
Do not stop Saxenda without medical advice. If you experience severe abdominal pain, persistent vomiting, or signs of pancreatitis, stop the medication immediately and seek urgent medical review. For manageable symptoms, contact your prescriber to discuss dose adjustment or management strategies.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.